1 How to Perform a Focused Pelvic Examination of a Woman With Pelvic Floor Dysfunction
To view the videos discussed in this chapter, please go to expertconsult.com. To access your account, look for your activation instructions on the inside front cover of this book.
Female pelvic floor dysfunction can be broadly categorized into five therapeutic areas:
1. Lower urinary tract symptoms (including incontinence, overactive bladder, and emptying problems)
2. Pelvic support defects (resulting in POP)
3. Defecatory dysfunction (including anal-fecal incontinence, constipation, outlet obstruction)
4. Sexual dysfunction (including dyspareunia, orgasmic dysfunction, and decreased libido)
5. Pelvic pain, which can originate from the bladder, the uterus, the vagina, or the lower gastrointestinal tract
All women with any of the aforementioned conditions should undergo a focused examination of the pelvic floor (Videos 1-1 and 1-2 ![]() ). The goal of the examination is to attempt to correlate the functional abnormality of which the patient complains with the anatomical abnormalities present on examination. It is also important to view the pelvis as a whole and not to focus on one specific area. For example, if a woman complains of stress incontinence, not only should the anterior vaginal compartment be examined, but also the entire pelvic floor should be checked for functional integrity and associated anatomical abnormalities. A systematic pelvic examination can be facilitated by dividing the pelvic floor into six specific anatomical areas:
). The goal of the examination is to attempt to correlate the functional abnormality of which the patient complains with the anatomical abnormalities present on examination. It is also important to view the pelvis as a whole and not to focus on one specific area. For example, if a woman complains of stress incontinence, not only should the anterior vaginal compartment be examined, but also the entire pelvic floor should be checked for functional integrity and associated anatomical abnormalities. A systematic pelvic examination can be facilitated by dividing the pelvic floor into six specific anatomical areas:
1. Distal anterior vaginal wall
2. Proximal anterior vaginal wall
4. Distal posterior vaginal wall
5. Proximal posterior vaginal wall
Assessment in each area should focus on level of support, sensation, and tone.
Assessment of Support and Stress Incontinence
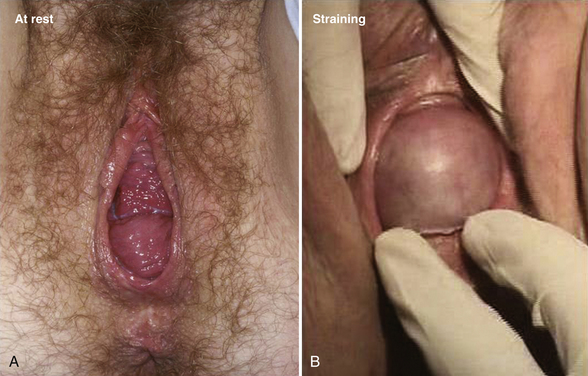
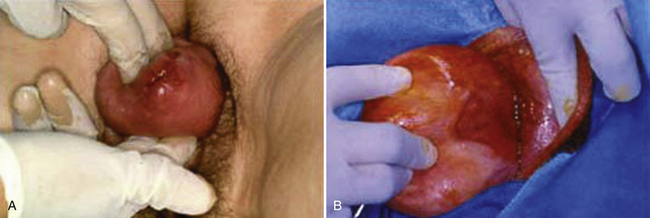
A speculum examination is performed with the posterior blade of a Graves or bivalved speculum (split-speculum technique) in a systematic manner so that the anterior, apical, and posterior compartments of the vagina can be assessed. First the posterior vaginal wall is retracted and assessment is performed for anterior prolapse (cystocele), apical prolapse (prolapse of the cervix or vaginal cuff), and urethral masses (Fig. 1-1). Scarring from previous surgery and the extent of prolapse can be seen during straining (Fig. 1-2). The effect of straining on the external urethral meatus can also be seen. For inspection of the vaginal cuff and apex, two blades can be inserted individually, one anteriorly and one posteriorly, to assess the support of these structures and differentiate apical from anterior defects (Fig. 1-3). In cases in which there appears to be cervical or uterine descent, it is important to differentiate between cervical elongation and true uterine descent (Figs. 1-4 and 1-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree