Nowadays, 5 nonsurgical flexible endoscopic techniques are available for small bowel endoscopy: push enteroscopy (PE), balloon-assisted enteroscopy using 2 balloons (double-balloon enteroscopy [DBE]) or 1 balloon (single-balloon enteroscopy [SBE]), balloon-guided enteroscopy (BGE), and spiral enteroscopy (SE). PE is a cost-saving, easy, and fast procedure for the examination of the proximal jejunum, but for a deep small bowel endoscopy, the other flexible enteroscopic techniques are required. BGE does not play a considerable role in deep small bowel endoscopy. DBE is the oldest flexible enteroscopic technique. Actually, the balloon-assisted enteroscopy (BAE) techniques with one balloon (SBE) or two balloons (DBE) are the mainly used techniques. DBE has become established throughout the world for diagnostic and therapeutic examinations of the small bowel and is now used universally in clinical routine work. DBE is still regarded as the gold standard nonsurgical procedure for deep small bowel endoscopy, because it provides the highest rates of complete enteroscopy, which becomes increasingly useful. The recently introduced SE technique represents a promising method but still needs technical improvement. Larger prospective studies on SE and prospective studies comparing the 3 systems (DBE, SBE, SE) are awaited before conclusive assessments can be made.
Flexible enteroscopy is a more invasive procedure in comparison with the purely diagnostic capsule endoscopy. However, the main advantages of flexible enteroscopy in comparison with other imaging procedures (eg, capsule endoscopy and magnetic resonance Sellink) are that it allows histologic sampling and endoscopic therapy. Nowadays, several techniques are available for the approach of the small bowel, including push enteroscopy (PE), balloon-assisted enteroscopy (BAE) using 2 balloons (double-balloon enteroscopy [DBE]) or 1 balloon (single-balloon enteroscopy [SBE]), balloon-guided enteroscopy (BGE), and spiral enteroscopy (SE). PE became established in the 1980s but is associated with only a limited depth of penetration into the small bowel. This limitation was overcome through the development of BAE using the DBE or SBE technique. In optimal cases, the entire small bowel, or at least considerable proportions of it, can be visualized using balloon enteroscopy (usually by combining the oral and anal examinations). This system has become established throughout the world for diagnostic and therapeutic small bowel examinations and is now being used universally in clinical routine work. In addition to the classic indication for small bowel endoscopy, the DBE or SBE technique has a variety of other potential uses as well, for example, in difficult ileocolonoscopies, for access to the pancreatic and biliary tract in patients with a surgically modified gastrointestinal tract, and for access to the stomach in patients who have undergone bariatric surgery. SE is another promising recently introduced enteroscopic system that is equipped with a raised helix at the tip of the overtube. In contrast to the BAE techniques, which follow the push-and-pull principle, this new enteroscopic technique pleats the small bowel by rotating.
Flexible enteroscopic techniques
PE
Push video enteroscopes are 200- to 250-cm long devices (dependent on type and manufacturer) and might be used with a stiff overtube (85–120 cm) to prevent looping of the enteroscope in the stomach. Although initial studies showed an increase in the depth of insertion with the use of an overtube, later studies with graded-stiffness enteroscopes have questioned the additional value of the overtube. The following are the main advantages of PE: it is easy and quick to perform, it is not a staff-consuming procedure, the overtube is reusable, and there is no need to set up a special system (eg, a pump control system). All these facts avoid extra costs and, therefore, PE is a cost-saving technique for the investigation of the proximal small bowel. PE for the lower digestive tract is not commonly performed because insertion depth of colonoscopy with ileoscopy seems equivalent to lower PE.
BAE
DBE
The DBE system (Fujinon, Inc, Saitama, Japan) consists of a high-resolution video endoscope with a working length of 200 cm and a flexible overtube made of polyurethane. Latex balloons are attached both at the tip of the enteroscope and also on the overtube and they can be inflated with air or deflated using a pressure-controlled pump. At present, 3 different types of devices are available with the DBE system. First type is the EN450-P5 model with a working channel of 2.2 mm and an outer diameter of 8.5 mm. Second is the EN450-T5 model with a working channel of 2.8 mm and an outer diameter of 9.4 mm. The corresponding overtubes have diameters of 12.2 and 13.2 mm with an overall length of 145 cm. Third is the EC450-BI5 model with a length of 152 cm, an outer diameter of 9.4 mm, a working channel of 2.8 mm, and a corresponding overtube with a diameter of 13.2 mm and a length of 110 cm. This device is mainly used for difficult ileocolonoscopy, endoscopic retrograde cholangiopancreatography in surgically altered anatomy, or proximal small bowel endoscopy. The main advantage is that there is no need for specially designed accessories, and all standard equipment can be used.
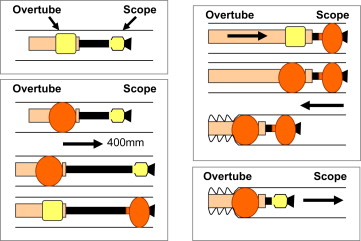
The principle of the DBE technique is based on alternating pushing and pulling maneuvers and alternating inflation and deflation of the balloons, allowing the small bowel to be threaded step-by-step onto the overtube ( Fig. 1 ). Depending on the intention, the pleated small bowel can slip down very fast or slowly from the overtube during withdrawal, using the alternating inflation and deflation of the overtube balloon while pulling back the scope. To optimize the visualization, the balloon at the endoscope tip is used in addition to air insufflation, if necessary. The endoscope balloon can then be partly inflated to a balloon setting pressure of 4 to 5 kPa, helping to pull apart the pleated folds.
SBE
The SBE system was introduced as a simplification of the DBE device. The enteroscope (XSIF Q160Y or SIF-Q180 [Olympus Optical Co, Tokyo, Japan]) is also a high-resolution video endoscope, with a working length of 200 cm. The enteroscope is equipped with a working channel of 2.8 mm diameter and its outer diameter is 9.2 mm. The overtube has an overall length of 140 cm and consists of silicone as well as the balloon at its distal end. In contrast to the DBE system, the balloon is not attached to the tip of the enteroscope, and stable positioning in the small bowel, for example, during advance of the overtube, is achieved by angling the tip of the endoscope or by the so-called power suction. Insufflation of the overtube balloon is performed using a pressure-controlled pump. The small bowel is threaded step-by-step onto the overtube and by alternating pushing and pulling maneuvers.
In principle, the DBE system can also be used as an SBE technique by dispensing with the balloon attached to the enteroscope tip ( Fig. 2 ).

BGE
The BGE system (NaviAid BGE, Smart Medical Systems Ltd, Israel) enables enteroscopy with standard endoscopes and endoscopic equipment. The BGE device comprises a 2-balloon add-on disposable element and an air supply unit to control the inflation and deflation of the balloons. The BGE also follows the push-and-pull principle, but in contrast to DBE and SBE, the guidance during advancement into the small bowel is taken by the balloon, not by the endoscope.
SE
For SE, a special overtube called Discovery Small Bowel (Spirus Medical Inc, Stoughton, MA, USA) has to be used. This overtube consists of polyvinyl chloride and has a length of 118 cm, an outer diameter of 16 mm, and an internal diameter of 9.8 mm. Therefore, both the slim enteroscopes manufactured by Fujinon and Olympus (without overtube or balloon) can be used for SE. The tip of the overtube has a raised hollow spiral that is 5.5 mm high over a length of 21 cm ( Fig. 3 ). In addition, the overtube has 2 handles for manual rotation, a locking device at the proximal part, and an injection port for lubrication. A special jelly has to be used for lubrication. By clockwise rotation of the overtube, the small bowel is pleated onto the overtube, and for withdrawal, counterclockwise rotation is performed.

Examination procedure
Preparation
For all deep small bowel endoscopic techniques, the patients generally only needed to fast before the oral examination (approximately 10–12 hours for food and 2–4 hours for clear liquids). Laxative measures before oral examinations should only be performed in patients with signs of intestinal obstruction or with diabetic neuropathy with delayed transit. For the anal examination, patients should undergo bowel preparation in the same way as for colonoscopy, including splitting, which means taking half of the bowel cleansing solution on the day before enteroscopy and half on the day of the enteroscopy. In patients with constipation or other motility disorders, intensification of the laxative preparation is recommended.
Sedation
Depending on the condition of the patient (eg, age, comorbidities), most examinations can be performed with the patients under conscious sedation in the same way as in colonoscopy and upper gastrointestinal tract endoscopy. For difficult and long investigations or patients who are difficult to handle with conscious sedation, propofol can be used as an alternative. For SE, propofol-based sedation is recommended. General anesthesia with intubation is not customary in Germany and is restricted to individual cases, for example, in children. But in other countries, general anesthesia with intubation is used more often. There is a wide range of sedation options and their selection is related to local conditions and policies.
CO 2 Insufflation
A previous prospective 2-center study demonstrated substantial advantages with regard to patient comfort and insertion depth with the use of CO 2 insufflation instead of air insufflation in DBE. Despite these positive data, however, the use of CO 2 has not yet become generally established.
Fluoroscopy
Depending on the experience of the endoscopist and the patient’s anatomic conditions, radiological fluoroscopy can be used optionally in flexible enteroscopy. Particularly, in the case of adhesions after abdominal surgeries, fluoroscopy is very useful. When stenoses are expected, for example, in patients with Crohn disease, radiology is certainly useful because the radiographic contrast image allows good assessment of the complexity of impassable stenoses.
Therapeutic Interventions
Therapeutic interventions should be generally performed during withdrawal of the instrument to avoid perforation caused by stretching of the small bowel wall during push-and-pull maneuvers or rotation. Endoscopic treatment of angiodysplasias or vascular malformations can be performed during endoscope advancement only if capsule endoscopy had previously shown a solitary or only very few small lesions (<5) to prevent the lesions from being missed between the threaded folds during withdrawal. During withdrawal of the endoscope and therapeutic interventions, spasmolytics improve visualization of the small bowel mucosa by reducing peristalsis of the small bowel. Because of the length of the enteroscopes and loop formation within the small bowel, insertion of accessories through the working channel might be troublesome. In these cases, straightening of the enteroscope position or the flexed enteroscope tip as well as enlargement of small cramped loops under fluoroscopic control is helpful. In addition, lubrication of the working channel with, for example, silicon oil, is recommended to facilitate insertion of devices through the working channel.
In Germany, therapeutic examinations are performed on an inpatient basis, but there might be different ways of management in different countries. Patients should be inquired about symptoms approximately 4 hours after the end of the examination as well as the next day. The method to allow patients only to drink water or tea until the next morning after therapy proved to be worthwhile in the author’s experience.
Measurement of Insertion
PE cannot evaluate the nonoperated small bowel in its entire length, and generally, the reported insertion depths from the oral route are given as postpyloric distance. If an overtube is used, the overtube is held in a stable position during advancement of the enteroscope to avoid looping in the stomach. The enteroscope is inserted as far as possible into the small bowel. After straightening, the scope is pulled back until the pylorus is reached again. The distance in centimeters between the pylorus and the deepest point after straightening of the scope is measured as the insertion depth. In the same way, the distance past the ligament of Treitz can be measured.
All BAE techniques follow the push-and-pull principle. The insertion depth of the endoscope into the small bowel is estimated by recording the net advancement of the endoscope for each push-and-pull maneuver on a standardized documentation sheet. In other words, the endoscopist has to estimate the effective insertion length of the enteroscope by the endoscopic checking of the instrument’s advancement and the length of small bowel released during insertion of the overtube and pulling back of the enteroscope and overtube. At the end of the examination, all the individual lengths advanced are added up. This technique requires some experience but it has been evaluated using an animal model. For SBE with an inverted tip technique, this measurement might not be feasible because during the pull maneuver, the angulated tip of the endoscope obstructs the view and makes it more difficult to estimate the length of each step.
In contrast to the push-and-pull enteroscopic techniques, which measure the insertion depths step-by-step on intubation, the insertion depth during SE is estimated on withdrawal. In other words, the endoscopist has to estimate how much small bowel is released from the overtube on the way back, which might be done in a reliable way by experienced and model-trained enteroscopists. But generally it is only a very rough estimation, which is even more susceptible to bias than the step-by-step measurement of DBE. This estimation is problematic for trials comparing insertion depths of the different enteroscopic techniques. Therefore, the only objective parameter is the rate of complete enteroscopy.
Examination procedure
Preparation
For all deep small bowel endoscopic techniques, the patients generally only needed to fast before the oral examination (approximately 10–12 hours for food and 2–4 hours for clear liquids). Laxative measures before oral examinations should only be performed in patients with signs of intestinal obstruction or with diabetic neuropathy with delayed transit. For the anal examination, patients should undergo bowel preparation in the same way as for colonoscopy, including splitting, which means taking half of the bowel cleansing solution on the day before enteroscopy and half on the day of the enteroscopy. In patients with constipation or other motility disorders, intensification of the laxative preparation is recommended.
Sedation
Depending on the condition of the patient (eg, age, comorbidities), most examinations can be performed with the patients under conscious sedation in the same way as in colonoscopy and upper gastrointestinal tract endoscopy. For difficult and long investigations or patients who are difficult to handle with conscious sedation, propofol can be used as an alternative. For SE, propofol-based sedation is recommended. General anesthesia with intubation is not customary in Germany and is restricted to individual cases, for example, in children. But in other countries, general anesthesia with intubation is used more often. There is a wide range of sedation options and their selection is related to local conditions and policies.
CO 2 Insufflation
A previous prospective 2-center study demonstrated substantial advantages with regard to patient comfort and insertion depth with the use of CO 2 insufflation instead of air insufflation in DBE. Despite these positive data, however, the use of CO 2 has not yet become generally established.
Fluoroscopy
Depending on the experience of the endoscopist and the patient’s anatomic conditions, radiological fluoroscopy can be used optionally in flexible enteroscopy. Particularly, in the case of adhesions after abdominal surgeries, fluoroscopy is very useful. When stenoses are expected, for example, in patients with Crohn disease, radiology is certainly useful because the radiographic contrast image allows good assessment of the complexity of impassable stenoses.
Therapeutic Interventions
Therapeutic interventions should be generally performed during withdrawal of the instrument to avoid perforation caused by stretching of the small bowel wall during push-and-pull maneuvers or rotation. Endoscopic treatment of angiodysplasias or vascular malformations can be performed during endoscope advancement only if capsule endoscopy had previously shown a solitary or only very few small lesions (<5) to prevent the lesions from being missed between the threaded folds during withdrawal. During withdrawal of the endoscope and therapeutic interventions, spasmolytics improve visualization of the small bowel mucosa by reducing peristalsis of the small bowel. Because of the length of the enteroscopes and loop formation within the small bowel, insertion of accessories through the working channel might be troublesome. In these cases, straightening of the enteroscope position or the flexed enteroscope tip as well as enlargement of small cramped loops under fluoroscopic control is helpful. In addition, lubrication of the working channel with, for example, silicon oil, is recommended to facilitate insertion of devices through the working channel.
In Germany, therapeutic examinations are performed on an inpatient basis, but there might be different ways of management in different countries. Patients should be inquired about symptoms approximately 4 hours after the end of the examination as well as the next day. The method to allow patients only to drink water or tea until the next morning after therapy proved to be worthwhile in the author’s experience.
Measurement of Insertion
PE cannot evaluate the nonoperated small bowel in its entire length, and generally, the reported insertion depths from the oral route are given as postpyloric distance. If an overtube is used, the overtube is held in a stable position during advancement of the enteroscope to avoid looping in the stomach. The enteroscope is inserted as far as possible into the small bowel. After straightening, the scope is pulled back until the pylorus is reached again. The distance in centimeters between the pylorus and the deepest point after straightening of the scope is measured as the insertion depth. In the same way, the distance past the ligament of Treitz can be measured.
All BAE techniques follow the push-and-pull principle. The insertion depth of the endoscope into the small bowel is estimated by recording the net advancement of the endoscope for each push-and-pull maneuver on a standardized documentation sheet. In other words, the endoscopist has to estimate the effective insertion length of the enteroscope by the endoscopic checking of the instrument’s advancement and the length of small bowel released during insertion of the overtube and pulling back of the enteroscope and overtube. At the end of the examination, all the individual lengths advanced are added up. This technique requires some experience but it has been evaluated using an animal model. For SBE with an inverted tip technique, this measurement might not be feasible because during the pull maneuver, the angulated tip of the endoscope obstructs the view and makes it more difficult to estimate the length of each step.
In contrast to the push-and-pull enteroscopic techniques, which measure the insertion depths step-by-step on intubation, the insertion depth during SE is estimated on withdrawal. In other words, the endoscopist has to estimate how much small bowel is released from the overtube on the way back, which might be done in a reliable way by experienced and model-trained enteroscopists. But generally it is only a very rough estimation, which is even more susceptible to bias than the step-by-step measurement of DBE. This estimation is problematic for trials comparing insertion depths of the different enteroscopic techniques. Therefore, the only objective parameter is the rate of complete enteroscopy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








