and Christopher Isles2
(1)
Institute of Cardiovascular and Medical Sciences, University of Glasgow, Glasgow, UK
(2)
Dumfries and Galloway Royal Infirmary, Dumfries, UK
Q1 What is hepatorenal syndrome?
Hepatorenal syndrome (HRS) is defined as the occurrence of renal failure in a patient with advanced liver disease in the absence of an identifiable cause of renal failure. It is a diagnosis of exclusion. More commonly a complication of chronic liver disease, HRS will develop in up to 40 % of patients with advanced cirrhosis and ascites by 5 years. HRS can also complicate acute liver failure in those who present with fulminant hepatic failure of any cause (e.g. severe alcoholic or viral hepatitis).
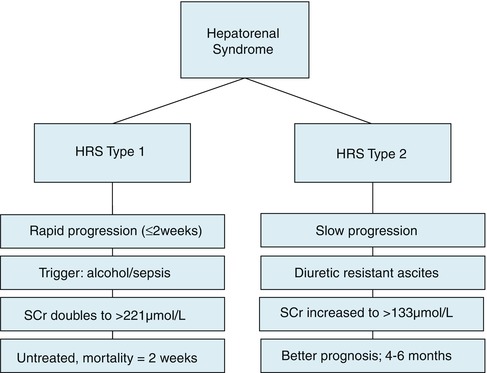
Q2 There are two types of HRS. Discuss.
Type 1 HRS is characterised by doubling of serum creatinine to a final value greater than 221 μmol/l over a period of less than 2 weeks. It is usually triggered by an episode of severe alcoholic hepatitis or by a septic insult such as spontaneous bacterial peritonitis (SBP) in a patient with end stage liver disease. Untreated the median survival of type 1 HRS is approximately 2 weeks.
Type 2 HRS occurs in patients with diuretic resistant ascites. It is characterised by a slower and less progressive rise in serum creatinine to a value exceeding 133 μmol/l. It carries a better prognosis than type 1 HRS with a median survival of 4–6 months (Fig. 13.1).
This is complex. There are at least three key features: Splanchnic vasodilatation in response to nitric oxide produced as a result of decreased hepatic perfusion; impairment of cardiac function due to cirrhotic cardiomyopathy and reduced production of renal prostaglandins which normally dilate the afferent arteriole. All three mechanisms will compromise renal perfusion.
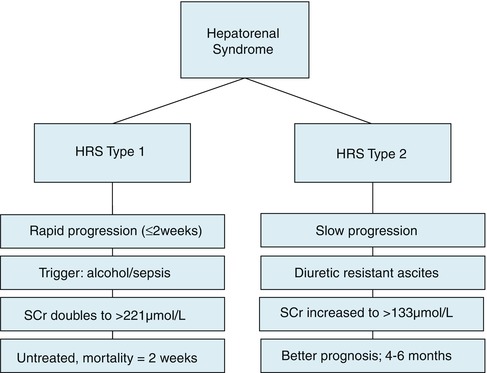
Fig. 13.1
The two types of hepatorenal syndrome
Q3 Describe the pathophysiology of HRS.
Q4 How do you diagnose HRS?
There is no single diagnostic test. Rather HRS is deemed likely in a patient with clinical stigmata of cirrhosis who develops acute kidney injury (type 1) or more slowly progressive renal failure (type 2) in the absence of other obvious causes of acute kidney injury. Diuretic resistant ascites may or may not be present in type 1 and is always present in type 2. Previously, on-going bacterial infection excluded HRS but it is now recognised that bacterial infection and in particular SBP is the most important trigger. The revised International Ascites Club criteria for HRS are shown in the box.
Box 13.1 Criteria for Diagnosis of Hepatorenal Syndrome in Cirrhosis
Cirrhosis with ascites.
Serum creatinine >133 μmol/l.
Absence of shock< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








