Chapter 12 Hepatorenal syndrome
Overview
1. The term hepatorenal syndrome (HRS) was initially applied to many different disorders involving the liver and the kidney.
2. During the 1960s and the 1970s, nephrologists in the United States popularized the term to define renal failure in cirrhosis.
TABLE 12.1 Diagnostic criteria for hepatorenal syndrome
| 1. Cirrhosis with ascites |
| 2. Serum creatinine level greater than 133 μmol/L (1.5 mg/dL) |
| 3. Lack of improvement in serum creatinine level (i.e., lack of a decrease to a level of ≤ 133 μmol/L) after ≥2 days following diuretic withdrawal and volume expansion with albumin; recommended dose of albumin: 1 g/kg of body weight per day up to a maximum of 100 g/day |
| 4. Absence of shock |
| 5. Lack of current or recent treatment with nephrotoxic drugs |
| 6. Absence of parenchymal kidney disease as indicated by proteinuria >500 mg/day, microhematuria (>50 red blood cells/high-power field), and/or abnormal renal ultrasonography |
Definition
1. Renal failure, estimated by a level of serum creatinine greater than 1.5 mg/dL, occurring in a patient with advanced liver disease and portal hypertension
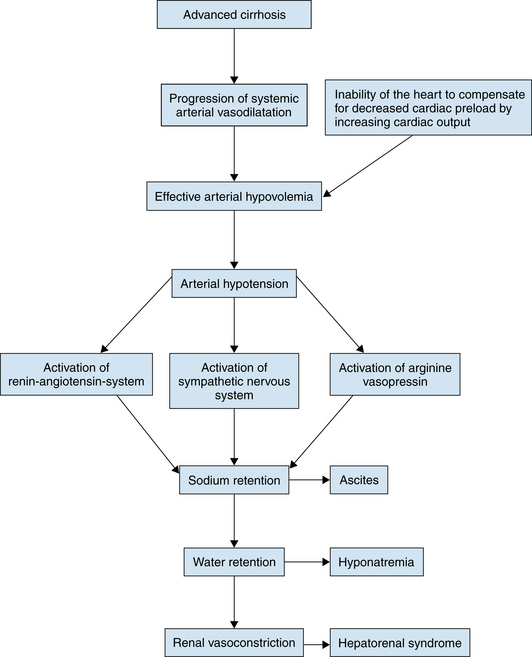
Pathogenesis
3. Systemic hemodynamics
 Hemodynamic alteration results from severe arterial vasodilation located mainly in the splanchnic territory.
Hemodynamic alteration results from severe arterial vasodilation located mainly in the splanchnic territory.
 The hemodynamic profile is characterized by hypervolemia, low arterial pressure, and low systemic vascular resistance.
The hemodynamic profile is characterized by hypervolemia, low arterial pressure, and low systemic vascular resistance.
 In the setting of increased activity of vasoconstrictor systems, marked renal vasoconstriction develops.
In the setting of increased activity of vasoconstrictor systems, marked renal vasoconstriction develops.
 Vasoconstriction occurs not only in renal circulation but also in brachial, femoral, and cerebral blood flow, probably as a compensatory mechanism to counteract splanchnic vasodilation.
Vasoconstriction occurs not only in renal circulation but also in brachial, femoral, and cerebral blood flow, probably as a compensatory mechanism to counteract splanchnic vasodilation.
 HRS has been traditionally assumed to develop in the setting of progression of the hyperdynamic circulation with high cardiac output; however, in few studies assessing cardiovascular function in patients with HRS or refractory ascites, cardiac output was found to be significantly reduced compared with patients without HRS.
HRS has been traditionally assumed to develop in the setting of progression of the hyperdynamic circulation with high cardiac output; however, in few studies assessing cardiovascular function in patients with HRS or refractory ascites, cardiac output was found to be significantly reduced compared with patients without HRS.
 Hemodynamic alteration results from severe arterial vasodilation located mainly in the splanchnic territory.
Hemodynamic alteration results from severe arterial vasodilation located mainly in the splanchnic territory. The hemodynamic profile is characterized by hypervolemia, low arterial pressure, and low systemic vascular resistance.
The hemodynamic profile is characterized by hypervolemia, low arterial pressure, and low systemic vascular resistance. In the setting of increased activity of vasoconstrictor systems, marked renal vasoconstriction develops.
In the setting of increased activity of vasoconstrictor systems, marked renal vasoconstriction develops. Vasoconstriction occurs not only in renal circulation but also in brachial, femoral, and cerebral blood flow, probably as a compensatory mechanism to counteract splanchnic vasodilation.
Vasoconstriction occurs not only in renal circulation but also in brachial, femoral, and cerebral blood flow, probably as a compensatory mechanism to counteract splanchnic vasodilation. HRS has been traditionally assumed to develop in the setting of progression of the hyperdynamic circulation with high cardiac output; however, in few studies assessing cardiovascular function in patients with HRS or refractory ascites, cardiac output was found to be significantly reduced compared with patients without HRS.
HRS has been traditionally assumed to develop in the setting of progression of the hyperdynamic circulation with high cardiac output; however, in few studies assessing cardiovascular function in patients with HRS or refractory ascites, cardiac output was found to be significantly reduced compared with patients without HRS.4. Vasoconstrictor systems
5. Vasodilatory factors
b. Nitric oxide (NO)
 Under normal conditions, NO plays a role in the regulation of glomerular microcirculation, sodium excretion, and renin release.
Under normal conditions, NO plays a role in the regulation of glomerular microcirculation, sodium excretion, and renin release.
 Inhibition of NO does not induce renal vasoconstriction as a result of the compensatory increase of renal PGs.
Inhibition of NO does not induce renal vasoconstriction as a result of the compensatory increase of renal PGs.
 Inhibition of both NO and PGs induces renal vasoconstriction in patients with cirrhosis and ascites.
Inhibition of both NO and PGs induces renal vasoconstriction in patients with cirrhosis and ascites.
 Under normal conditions, NO plays a role in the regulation of glomerular microcirculation, sodium excretion, and renin release.
Under normal conditions, NO plays a role in the regulation of glomerular microcirculation, sodium excretion, and renin release. Inhibition of NO does not induce renal vasoconstriction as a result of the compensatory increase of renal PGs.
Inhibition of NO does not induce renal vasoconstriction as a result of the compensatory increase of renal PGs. Inhibition of both NO and PGs induces renal vasoconstriction in patients with cirrhosis and ascites.
Inhibition of both NO and PGs induces renal vasoconstriction in patients with cirrhosis and ascites.