Chapter 28 Hepatic abscesses and cysts
3 The differentiation between amebic and pyogenic hepatic abscess relies on an adequate history (including travel history), imaging pattern, culture results, and serologic testing.
4 A history of dysentery or diarrhea is present in only 20% of patients with an amebic liver abscess. Amebic liver abscess is readily treated by antibiotics and luminal amebicides.
5 Pyogenic liver abscess is a life-threatening condition, resulting from infected blood or bile. Abscesses are frequently polymicrobial and include anaerobic organisms. Treatment is with appropriate antibiotics and drainage.
Amebic Liver Abscess
Overview
2. Amebic infection may be asymptomatic or may manifest as dysentery, hepatic amebic abscess, or other (rarer) manifestations.
3. The diagnosis and management of hepatic amebic abscess have been revolutionized by advances in imaging and interventional radiology.
Parasitology
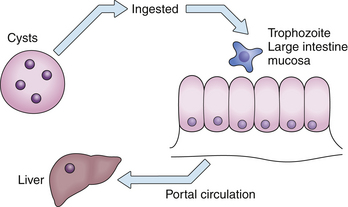
1. Amebic liver abscess is caused by the protozoan E. histolytica. The reservoir of infection is human (Fig. 28.1).
2. The infective form is the cyst (12 μm in diameter), which is ingested. Excystation occurs in the small intestine. The trophozoite (10 to 60 μm) infects the colon and may cause inflammation and dysentery. Amebae spread to the liver through the portal circulation.
3. The cyst is able to survive outside the body for weeks or months, whereas the trophozoite degenerates in minutes.
4. Amebae may be pathogenic or nonpathogenic. The nonpathogenic form has been reclassified as Entamoeba dispar. Pathogenic species can be differentiated from nonpathogenic species by the following:
Epidemiology
1. Infection with E. histolytica affects 10% of the world’s population; 40 to 50 million people develop amebic colitis or amebic liver abscess, and 40,000 to 100,000 deaths occur per year.
2. The prevalence of infection varies from less than 1% in industrialized countries to 50% to 80% in some tropical regions, and it has been found to be 100% in an area of The Gambia.
Pathogenesis
1. In the liver, E. histolytica lyses the host’s tissue with proteolytic enzymes contained in cytoplasmic vacuoles.
2. The hepatic lesion is a well-demarcated abscess consisting of necrotic liver and usually affecting the right lobe. The initial host response to the ameba is neutrophil migration, but the ameba can also lyse neutrophils, thus releasing their enzymes and assisting in the process of tissue destruction.
3. The abscess contains acellular debris; amebic trophozoites are found only at the periphery of the lesion, where they can invade further.
Diagnosis
2. Diagnostic imaging
3. Serologic tests: The detection of antibodies is the mainstay of diagnosis of invasive amebiasis. Available assays include the following:
TABLE 28.1 Laboratory findings in amebic liver abscess
| Laboratory finding | Frequency (%) |
|---|---|
| Leukocytosis | 80 |
| Elevated serum alkaline phosphatase level | 80 |
| Anemia | >50 |
| Increased erythrocyte sedimentation rate | Common |
| Proteinuria | Common |
| Elevated serum aminotransferase levels | Poor prognostic sign |
Complications
Treatment and prognosis
Treatment of amebic liver abscess is usually with drugs alone.
1. Commonly used regimens (administered orally):
 Metronidazole 750 mg three times daily for 5 to 10 days (pediatric, 35 to 50 mg/kg per day in three divided doses for 5 days), or
Metronidazole 750 mg three times daily for 5 to 10 days (pediatric, 35 to 50 mg/kg per day in three divided doses for 5 days), or
 Chloroquine 1 g loading dose for 1 to 2 days, then 500 mg/day (pediatric, 10 mg/kg base) for 20 days. Luminal amebicides must always be used following the aforementioned regimens:
Chloroquine 1 g loading dose for 1 to 2 days, then 500 mg/day (pediatric, 10 mg/kg base) for 20 days. Luminal amebicides must always be used following the aforementioned regimens:




 Metronidazole 750 mg three times daily for 5 to 10 days (pediatric, 35 to 50 mg/kg per day in three divided doses for 5 days), or
Metronidazole 750 mg three times daily for 5 to 10 days (pediatric, 35 to 50 mg/kg per day in three divided doses for 5 days), or Chloroquine 1 g loading dose for 1 to 2 days, then 500 mg/day (pediatric, 10 mg/kg base) for 20 days. Luminal amebicides must always be used following the aforementioned regimens:
Chloroquine 1 g loading dose for 1 to 2 days, then 500 mg/day (pediatric, 10 mg/kg base) for 20 days. Luminal amebicides must always be used following the aforementioned regimens:– Diloxanide furoate 500 mg three times daily (pediatric, 20 mg/kg per day in three divided doses) for 10 days, or
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree