CHAPTER 3 Heller myotomy with toupet or dor fundoplication for achalasia
Step 1. Clinical anatomy
♦ The sling fibers of Willis on the cardia of the stomach provide some competency of the lower esophageal sphincter (LES). Therefore, to completely obliterate these fibers, the myotomy should be carried at least 3 cm onto the stomach.
♦ To ensure an adequate myotomy onto the stomach, both the cardioesophageal fat pad and anterior (left) vagus should be mobilized as they cover the portion of cardia that is included in the myotomy.
♦ In patients with end-stage achalasia and a dilated sigmoid esophagus, the gastroesophageal (GE) junction is often angulated. Therefore, consideration for not doing a fundoplication should be given lest the distal esophagus be angulated more.
Step 2. Preoperative considerations
♦ Manometry is essential to make the diagnosis, demonstrating an aperistaltic esophagus and an incomplete relaxation of the LES.
♦ Upper endoscopy and fluoroscopic evaluation should be used to exclude other pathology and to determine the amount of esophageal dilation.
♦ In patients over 50 years of age, symptoms less than 6 months, or those with significant weight loss (>10 to 20 lbs), CT scan or endoscopic ultrasound should be performed to rule out pseudoachalasia (i.e., a tumor obstructing the esophagus).
♦ In patients with atypical presentations, botulinum toxin A (Botox) can be used as a diagnostic tool to identify those who would benefit from a myotomy.
Positioning
♦ Patients are placed in modified lithotomy with both arms tucked.
♦ A beanbag overhangs the edge of the operative table to form a saddle around the patient’s perineum to avoid sliding.
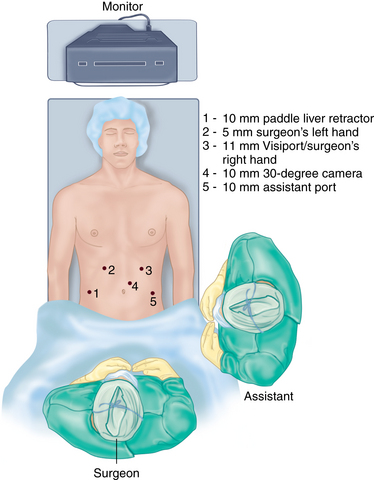
♦ The operative surgeon stands between the patient’s legs with the assistant at the patient’s left side.
♦ Monitors are placed above the patient’s head.
♦ An oral-gastric tube can be used to decompress the stomach and then removed.
♦ After port placement, the patient is placed in steep reverse Trendelenburg position.
Step 3. Operative steps
Port placement
♦ A small incision is made at the left costal margin in the mid-clavicular line.
♦ Pneumoperitoneum is established using a Veress needle, and the abdomen is entered using a Visiport trocar (Covidien; Mansfield, Massachusetts).
♦ The camera port is placed 4 cm left of midline and one hand’s breadth (approximately 10-12 cm) inferior to the left costal margin.
♦ A 10-mm 30-degree laparoscope camera provides superior visualization.
♦ The remaining four ports are placed under direct visualization.
♦ A 5-mm trocar is placed in the right upper quadrant (surgeon’s left hand), a 10-mm trocar is placed in the right lateral quadrant (paddle liver retractor), and 10-mm trocar is placed in the left lower quadrant (assistant port) (Figure 3-1).
Mobilization of esophagus
♦ The left phrenogastric ligament is divided to expose the left crus.
♦ The gastric fundus is mobilized by dividing the short gastric vessels using an ultrasonic dissector.
♦ Posterior attachments between the proximal stomach and retroperitoneum are divided to minimize tension on the subsequent fundoplication.
♦ The left phrenoesophageal membrane is divided.
♦ The gastrohepatic ligament is divided and carried toward the esophageal hiatus to expose the right crus.
♦ The nerves of Latarjet and aberrant or accessory vessels are preserved.
♦ The anterior phrenoesophageal membrane is divided.
♦ The anterior (left) vagus is identified, protected, and separated from the esophagus.
♦ A posterior esophageal window is created, which exposes the confluence of the right and left crus.
♦ The posterior (right) vagus is visualized and protected.
♦ A Penrose drain can be placed around the GE junction to retract the esophagus during the mobilization.
♦ An extensive hiatal and mediastinal esophageal dissection is performed to maximize the length of the myotomy.
♦ The cardioesophageal fat pad attachments to the underlying stomach and esophagus are divided. In doing so, the anterior (left) vagus is preserved and separated from the GE junction.
♦ This fat pad to the left of the anterior (left) vagus is then resected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree