A vast majority of ulcers of the stomach and duodenum are due to H pylori infection or nonsteroidal anti-inflammatory drug (NSAID) usage. In patients with apparent H pylori negative NSAID negative ulcers, it is essential to ensure that the H pylori tests are not falsely negative and that the patient is not taking mucosal damaging drugs unknowingly. There are a variety of rare causes of true H pylori negative NSAID negative ulcers which need to be considered, including underlying cancer/lymphoma, Crohn’s disease, rare infections and the Zollinger Ellison syndrome. Patients with idiopathic ulcers should be maintained on proton pump inhibitor therapy and may require higher doses than traditionally used in H pylori positive ulcers.
The major causes of ulceration of the stomach and duodenum are Helicobacter pylori infection and the use of nonsteroidal anti-inflammatory drugs (NSAIDs) or aspirin. However, some ulcers are apparently unrelated to those risk factors, and there is considerable variation in the reported proportion of such ulcers. Recent reports from North America suggest that up to 50% of ulcers are H pylori negative, whereas in other parts of the world, a proportion of H pylori -negative ulcers remains much lower at less than 5%. At least two factors may explain this marked variation in the reported proportion of ulcers being unrelated to H pylori infection and NSAIDs. The first is the background prevalence of H pylori infection in the community being studied, and the second is the robustness of the exclusion of H pylori infection and of the use of NSAIDs and aspirin ( Fig. 1 ).
The background prevalence of H pylori infection varies markedly between different countries, being almost 100% in some regions of the developing world and less than 10% in highly affluent communities. If one assumes that the risk of developing an ulcer in any country is one in four in an H pylori infected subject and one in 20 in an uninfected subject, one can calculate the effect of the background prevalence of the infection on the proportion of ulcers that are H pylori negative. This simple mathematical calculation indicates that the proportion of H pylori -negative ulcers would be only 5% in a country with a 65% background prevalence of the infection. In contrast, the proportion of H pylori -negative ulcers would be 44% in a country with a 20% background prevalence of H pylori infection. A relatively small decrease in the prevalence of the infection in the community markedly increases the proportion of H pylori- negative to H pylori -positive ulcers, as it simultaneously increases the number of H pylori -negative ulcers and decreases the number of H pylori -positive ulcers. The background prevalence of H pylori infection in Scotland is 65%, which is consistent with 95% of the ulcers occurring in H pylori -infected subjects. In the United States, the prevalence of H pylori infection is much slower at about 30% in the white population, which is consistent with 20% of the ulcer patients being H pylori negative.
If the prevalence of H pylori infection falls over the next few decades, so will the prevalence of ulcer disease. However, a proportion of H pylori -negative ulcers will progressively increase, and they will become a predominant type of ulcer disease.
The falling prevalence of H pylori infection may increase the prevalence of H pylori -negative ulcers as well as the proportion of H pylori -negative to -positive ulcers. It is quite likely that some patients with H pylori -positive ulcers would have developed these ulcers even in the absence of H pylori infection, but because of the infection, they are labeled H pylori -positive ulcers. Only with the fall in H pylori prevalence in the community will these ulcers become apparent as H pylori -negative ulcers and thus will increase the number categorized as H pylori -negative ulcers.
It is unclear whether ulcers that persist after successful H pylori eradication have a similar etiology to ulcers first presenting in the absence of the infection. The proportion of ulcers remaining unhealed following successful eradication of H pylori infection is approximately 10%. Are these ulcers the same as H pylori -negative ulcers with the infection merely having been an innocent bystander due to its high prevalence in the general population? Alternatively, has the infection produced permanent changes to the structure and function of the stomach, which continues to predispose to mucosal ulceration after the organism has been eradicated? The fact that the eradication of H pylori infection cures the great majority of patients with even severe ulcer disease, provided they are not NSAID or aspirin related, points against the infection causing a permanent ulcer diathesis. It would therefore seem most likely that ulcers recurring after H pylori eradication are equivalent to ulcers in patients without evidence of current or previous H pylori infection and should be classified and managed in the same way.
Management of patients with apparent H pylori -negative Nonstreoidal Anti-Inflammatory Drugs-negative ulcers
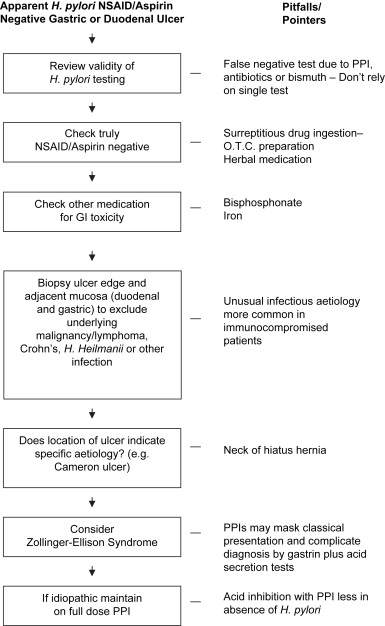
If a patient is found to have ulceration of the stomach or duodenum without evidence of H pylori infection or a history of NSAID/aspirin ingestion, then it is necessary to undertake further investigations to determine the etiology of the ulcer disease. Such investigations are necessary, because they may reveal causes that lead to the need for specific treatment. Merely treating a patient found to have an H pylori -negative NSAID-negative ulcer with acid inhibitory medication is probably inappropriate.
The first consideration in a patient not taking NSAIDs found to have chronic ulceration of the duodenum and stomach and a negative H pylori test is that the test result is a false negative. Several medications frequently prescribed for patients with upper gastrointestinal (GI) symptoms or disease result in false-negative H pylori tests. The elevation of intragastric pH by proton pump inhibitors or high-dose H 2 antagonists markedly reduces the bacterium’s urease activity and may produce false-negative urease tests, including the breath test and the urease strip test. Such therapy also reduces the density of colonization in both the gastric antrum and body. Though patients are advised to stop such medication 2 to 3 weeks before H pylori testing, compliance with this advice is unreliable, particularly in asymptomatic subjects. Many antibiotics, as well as bismuth-containing preparations, will also suppress H pylori infection and its urease activity. Even under optimal conditions, most individual H pylori tests have a sensitivity less than 95%, which means that 1 in 20 infected subjects may be missed.
One situation where H pylori infection is particularly likely to be missed is when a patient presents with acute upper GI bleeding secondary to ulcer disease. The biopsy urease test has a higher false-negative rate in this setting possibly due to the effect of blood in the stomach together with the medications prescribed in the acute clinical situation.
It is extremely important that H pylori is not missed in patients with ulcer disease, as this will deny them the chance of long-term cure of the condition by eradicating the infection. It will also leave them at increased risk of developing ulcer complications over subsequent years. To ensure that H pylori infection is not missed, it is important to take biopsies from both the antrum and body region of the stomach for both histology and urease tests. In addition, it may also be appropriate to check H pylori serology. A recent study has suggested that in some patients with duodenal ulceration, the infection is confined to the duodenal mucosa and eradicating it cures the ulcer disease. Consequently, in patients with duodenal ulceration and no evidence of H pylori in the stomach, biopsies should also be taken from the duodenal mucosa for examination for H pylori organisms.
In addition to thoroughly excluding H pylori infection, it is also important to be certain that the patient is not taking unrecognized NSAIDs or other medication that might be causing the condition. A careful history and examination of recent prescription records are important. Patients should also be carefully questioned about their use of over-the-counter medications including herbal medications, some of which contain salicylates. In some cases, urine and serum analyses to detect surreptitious use of these drugs may be appropriate. Several medications in addition to NSAIDs and aspirin may damage the GI mucosa, including iron, bisphosphonates, and colchicine, and all medicines recently taken by patients should be scrutinized for any potential mucosal-damaging effects. Careful reassessment of the H pylori status and NSAID aspirin usage will reduce the number of unexplained ulcers. However, a small proportion of ulcers does occur in the absence of well-established risk factors and may be related to a variety of other conditions. The one condition not to be missed in patients with unexplained gastric or duodenal ulceration is an underlying tumor. Before a routine biopsy is performed on the ulcers of the stomach to exclude cancer, this is not the practice for duodenal ulceration. However, in a patient with H pylori -negative NSAID-negative duodenal ulceration, the possibility of underlying carcinoma or lymphoma needs to be considered, and this is one situation where biopsies should also be taken from the duodenal ulcer and surrounding duodenal mucosa.
Another cause of gastric and/or duodenal ulceration in patients without H pylori infection and not taking NSAIDs/gastrin is Crohn’s disease. The pattern of upper GI ulceration associated with Crohn’s disease is highly variable. In some patients with Crohn’s disease, the disorder may be confined to the stomach and/or duodenum. Consequently, biopsies should be taken from both the duodenum and stomach in patients with unexplained ulcer disease to check for granulomas and other histologic features of Crohn’s disease. In certain circumstances, investigations of the more distal GI tract may be indicated.
Patients with ulceration of the upper GI tract have been reported to have infections other than H pylori . Goddard and colleagues reported that in duodenal ulceration associated with Helicobacter Heilmannii treating the infection with quadruple anti- H pylori therapy cured the ulcer disease. There are also a number of case reports of chronic gastric ulcers associated with cytomegalovirus infection in immunocompromised patients. The typical inclusion bodies are seen in the gastric biopsies. These ulcers healed following treatment with genciclovir. There is also a report of the presence of the herpes simplex virus in H pylori -negative ulcers, although the nature of the association is unclear.
Cameron and Higgins reported ulceration of the proximal stomach in patients with hiatus hernia and occurring where the gastric mucosa passes through the diaphragmatic hiatus. These ulcers were associated with iron deficiency anemia, although the nature of the association is unclear. The ulcers may be single or multiple. The authors postulated that these ulcers were related to mucosal trauma or ischemia. These Cameron ulcers were described before H pylori infection was recognized, and thus the role of the infection is unclear. However, if ulcers at this site are present in patients with no other explanation or persist after treating H pylori infection, they may well be caused by local mucosal trauma or ischemia.
Gastric ulceration has also been reported following high-dose radiotherapy of the upper abdominal region. This is assumed to have been a direct complication of the therapy, although the H pylori status of the patients has not been documented. For many years, radiotherapy of the thorax has been used to produce experimental duodenal ulcers in laboratory animals. It is thought to exert its effects by interfering with the protective functions afforded by the vagus nerve.
Ulcers may also occur in patients with severe systemic illness, for example, following extensive burns, and these stress ulcers are likely to be independent of H pylori status.
Systemic mastocytosis causes duodenal ulceration due to the histamine stimulating increased acid secretion. Other manifestations of the increased histamine release, including pruritis, flushing, and maculopapular rash, should make one suspect the diagnosis. In addition, a mast cell infiltrate is apparent in gastric and duodenal biopsies. The mechanism of duodenal ulceration in systemic mastocytosis would indicate that it may occur in the absence of H pylori infection, although this has not been formally documented.
Most of the causes of H pylori -negative NSAIDs/aspirin-negative ulcers can be detected by careful clinical history and upper GI endoscopy, including taking adequate biopsies of the ulcer and surrounding tissue and including both the stomach and the duodenum. If this does not provide a satisfactory explanation for mucosal ulceration, then one has to consider the possibility of Zollinger Ellison syndrome.
The Zollinger Ellison syndrome is due to an underlying gastrin-secreting tumor and effects of the hypergastrinemia on the upper GI tract. The constant high levels of gastric acid secretion stimulated by the persisting hypergastrinaemia usually result in severe and multiple ulcers of the stomach and duodenum, and the ulceration often extends into the more distal duodenum. Ulcer complications, including perforation and bleeding, are common, and reflux esophagitis is also associated with the condition. The syndrome may also cause diarrhea, which is thought to be due to the high levels of acid emptying the duodenum, denaturing the duodenal and pancreatic enzymes necessary for normal and esophageal function. Patients may have a family history of endocrine tumors, as the Zollinger Ellison syndrome is sometimes part of a multiple endocrine neoplasia syndrome. The classical description of the Zollinger Ellison syndrome was made before the age of powerful proton pump inhibitor therapy, which effectively suppresses the acid secretion and thus the severe manifestations of the disease. Patients with upper GI symptoms are usually commenced on acid inhibitory therapy before endoscopic investigation, and this may result in the endoscopic features being similar to patients with more common forms of ulcer disease. Proton pump inhibitor therapy also makes the diagnosis of the Zollinger Ellison syndrome by these additional tests more complicated. Interpretation of pentagastrin-stimulated acid output required discontinuation of proton pump inhibitor therapy, and this may be difficult and probably unwise in patients who may have an underlying gastrinoma. Rebound acid hypersecretion during the first few weeks after discontinuing proton pump inhibitor therapy may further complicate the interpretation of acid secretory tests. Serum gastrin may be difficult to interpret due to its increased concentration as a result of the proton pump inhibitor therapy, which will overlap with values in patients with gastrinoma. The most discriminating test in this situation is probably the secretin test. Following intravenous injection of secretin, the serum gastrin increases in patients with gastrinoma but not in control patients. A rise of 120 pg/mL is considered positive. This occurs due to the fact that gastrinomas have secretin receptors. It should, however, be noted that the effects of proton pump inhibitor therapy on the interpretation of the secretin test are not known.
Once all the above investigations have been completed, there remain a very small proportion of patients with apparently idiopathic ulcer disease. Do these patients have a similar unrecognized etiology or are they a heterogeneous group of patients with different unrecognized etiologies? We performed gastric function tests in a small group of subjects with idiopathic gastroduodenal ulceration and observed increased acid output, increased gastrin, and accelerated gastric emptying. Exaggerated gastrin response was also observed by Kamada and colleagues in three of nine idiopathic ulcer patients. These abnormalities resemble those occurring in patients with H pylori infection in whom the exaggerated gastrin caused by the infection leads to increased acid output and thus duodenal ulceration. It was suggested that some unrecognized underlying factor might be reproducing the changes in association with the H pylori infection. However, since then we and others have recognized that discontinuation of proton pump inhibitor therapy can produce the same abnormalities, that is, hypergastrinemia and rebound acid hypersecretion. Most of the patients who have been studied with idiopathic ulcer disease have been on powerful acid inhibitory therapy, and it is now unclear whether the abnormalities reported are indeed related to the underlying disease or related to its treatment with powerful acid inhibitory therapy.
The management of patients with idiopathic ulcers is unclear. The published studies of the value of acid inhibitor therapy in healing ulcers have been performed in patients with H pylori -positive ulcers or with NSAID associated ulcers. Proton pump inhibitor therapy has been shown to be more effective at inhibiting acid secretion in H pylori infected versus uninfected subjects. This can be explained by the fact that such therapy causes an increase in oxyntic mucosal gastritis, which impairs gastric secretion further and augments the pharmacologic effect of the drug. H pylori -negative ulcers are more difficult to manage and more susceptible to complications than traditional ulcers. This may be related to their reduced responsiveness to acid inhibitor therapy, and consequently increased doses of proton pump inhibitor therapy may be appropriate. The natural history of idiopathic ulcers is fully documented due to their rarity. In addition, the role of surgery to reduce gastric acid secretion is unclear. However, my personal experience is that these patients can be successfully managed in the long term on adequate proton pump inhibitor therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





