CHAPTER 20 Hand-assisted right colectomy
Step 1. Surgical anatomy
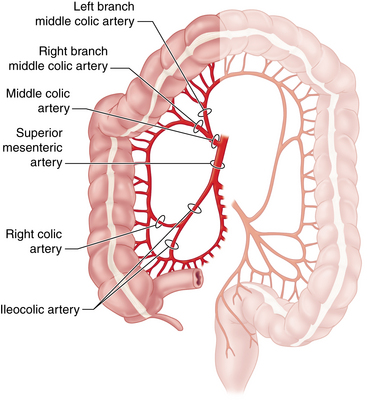
♦ Familiarity with the vascular anatomy of the right colon is essential to the safe conduct of a minimally invasive right colectomy (Figure 20-1). Vascular anatomy also significantly determines resection of colonic malignancies. Several key points guide the laparoscopic surgeon:
 The ileocolic artery (ICA) branches from the superior mesenteric artery (SMA) just over the duodenum after the take-off of the middle colic artery (MCA). It courses obliquely through the mesocolon to terminate at the cecum, giving off a terminal ileal branch that joins with the small bowel arcade from the SMA.
The ileocolic artery (ICA) branches from the superior mesenteric artery (SMA) just over the duodenum after the take-off of the middle colic artery (MCA). It courses obliquely through the mesocolon to terminate at the cecum, giving off a terminal ileal branch that joins with the small bowel arcade from the SMA. The right colic artery is usually a branch of the ICA rather than arising from the SMA as is historically depicted.
The right colic artery is usually a branch of the ICA rather than arising from the SMA as is historically depicted. The MCA proper is typically quite short, branching into two or more arteries (right branch, left branch) just 1 to 2 cm from the aortic origin of the SMA. Rarely is the main MCA itself divided in colon resections. The significant hazard of attempts to control bleeding from a transected main MCA is injury to the SMA.
The MCA proper is typically quite short, branching into two or more arteries (right branch, left branch) just 1 to 2 cm from the aortic origin of the SMA. Rarely is the main MCA itself divided in colon resections. The significant hazard of attempts to control bleeding from a transected main MCA is injury to the SMA. The branches of the MCA are most easily identified from the cranial aspect of the proximal transverse mesocolon. Once these branches and the adjacent mesocolon are transected, the origin of the ICA can be seen retroperitoneally, as can the more medially oriented SMA.
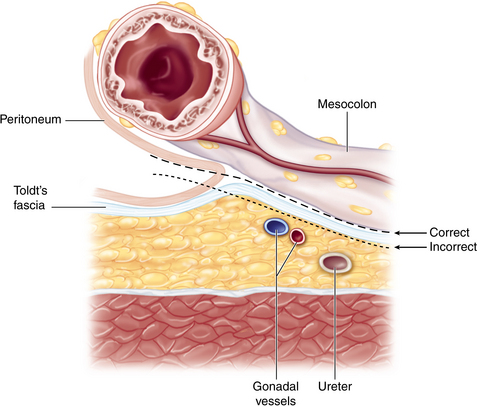
The branches of the MCA are most easily identified from the cranial aspect of the proximal transverse mesocolon. Once these branches and the adjacent mesocolon are transected, the origin of the ICA can be seen retroperitoneally, as can the more medially oriented SMA.♦ The embryologic fusion plane originates laterally at the white line of Toldt, which occurs where the parietal peritoneum fuses with the visceral peritoneal reflection around the colon and its lateral extension (Figure 20-2). The correct dissection plane is the bloodless embryologic fusion plane. When properly mobilized in this plane, the colon reflects medially on its mesentery to become a nearly midline structure. When the dissection is carried posteriorly past the white line of Toldt, violating the parietal peritoneum as it extends across the retroperitoneal structures, the ureter and gonadal vessels are put at risk and mobilization of the colon is limited.
♦ Awareness of the relationships between the cecum, ascending colon, hepatic flexure, and proximal transverse colon to neighboring structures helps to maintain orientation during surgery and prevents injury:
 The duodenal sweep can be appreciated medial and caudal to the hepatic flexure mesocolon. Risk of injury to the portal triad can be averted by avoiding performance of a Kocher maneuver.
The duodenal sweep can be appreciated medial and caudal to the hepatic flexure mesocolon. Risk of injury to the portal triad can be averted by avoiding performance of a Kocher maneuver. The right kidney and Gerota’s fascia are just lateral to the distal ascending colon. Dissection lateral to the embryologic fusion plane can lead to mobilization of the kidney or the second portion of the duodenum (Kocher maneuver).
The right kidney and Gerota’s fascia are just lateral to the distal ascending colon. Dissection lateral to the embryologic fusion plane can lead to mobilization of the kidney or the second portion of the duodenum (Kocher maneuver). The right ureter descends retroperitoneally and is not typically exposed unless dissection is carried posterior to the embryologic fusion plane.
The right ureter descends retroperitoneally and is not typically exposed unless dissection is carried posterior to the embryologic fusion plane. The lesser sac must be entered in order to take down the hepatic flexure and transect the transverse mesocolon and MCA branches. The stomach, the gastrocolic, and the hepatocolic ligaments constitute its anterior boundary. Posteriorly, one finds the pancreas and, to the right, the duodenal sweep.
The lesser sac must be entered in order to take down the hepatic flexure and transect the transverse mesocolon and MCA branches. The stomach, the gastrocolic, and the hepatocolic ligaments constitute its anterior boundary. Posteriorly, one finds the pancreas and, to the right, the duodenal sweep. The liver and gallbladder are superior to the hepatocolic ligament. Failure to appreciate this plane can lead to dissection of the porta hepatis.
The liver and gallbladder are superior to the hepatocolic ligament. Failure to appreciate this plane can lead to dissection of the porta hepatis.♦ Surface anatomy considerations principally help with optimal port placement:
 Preoperative knowledge of a redundant transverse colon would suggest more caudal placement of the periumbilical hand port incision.
Preoperative knowledge of a redundant transverse colon would suggest more caudal placement of the periumbilical hand port incision.Step 2. Preoperative considerations
Patient preparation
♦ Given that the majority of right colectomies are performed for neoplastic diseases (cancer or endoscopically unresectable polyps), staging must be complete before going to the operating room:
 A computed tomography (CT) scan of the chest, abdomen, and pelvis is central to the metastatic workup. A positron emission tomography (PET) scan is sometimes also necessary.
A computed tomography (CT) scan of the chest, abdomen, and pelvis is central to the metastatic workup. A positron emission tomography (PET) scan is sometimes also necessary. The CT scan may also reveal invasion into an adjacent structure, which could preclude a laparoscopic approach.
The CT scan may also reveal invasion into an adjacent structure, which could preclude a laparoscopic approach.♦ Lesions must be appropriately localized preoperatively. Although all of the patient’s physicians are concerned about making the correct diagnosis, only the surgeon has to perform a resection and must manage the technical details of this procedure:
 Review the colonoscopy report; note the expected location of the target lesion and the presence and character (including pathology report) of any other lesions.
Review the colonoscopy report; note the expected location of the target lesion and the presence and character (including pathology report) of any other lesions. Tattoos are critical for smaller or nonpalpable lesions. Note the type of dye used (India ink lasts, methylene blue disperses).
Tattoos are critical for smaller or nonpalpable lesions. Note the type of dye used (India ink lasts, methylene blue disperses).♦ Plan the extent of resection with regard to both margins and vascular ligation:
 The right branch of the MCA should be included for resection of neoplasms of the cecum or the proximal ascending colon.
The right branch of the MCA should be included for resection of neoplasms of the cecum or the proximal ascending colon. For neoplasms of the hepatic flexure or proximal transverse colon, all the MCA branches (or the trunk) must be included.
For neoplasms of the hepatic flexure or proximal transverse colon, all the MCA branches (or the trunk) must be included. For inflammatory bowel disease or other benign indications, there is no need to perform a high ligation of the arteries or regional lymphadenectomy.
For inflammatory bowel disease or other benign indications, there is no need to perform a high ligation of the arteries or regional lymphadenectomy.♦ Past surgical history and an abdominal examination may reveal risks that could present challenges to a minimally invasive approach:
 Surgical scars and history of adhesions or bowel obstruction may alter port site placement or technique of entry.
Surgical scars and history of adhesions or bowel obstruction may alter port site placement or technique of entry.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree