Hand-Assisted Left Colectomy
Matthew G. Mutch
Indications for the use of the hand-assisted approach to a laparoscopic left colectomy are the same as for an open or straight laparoscopic left colectomy. Advantages of the hand-assisted approach depend upon how it is utilized.
Adoption’data have demonstrated faster ascension of the learning curve.
Primary approach’data have shown shorter operative times and no difference in short-term outcomes when compared to the laparoscopic approach.
Difficult cases’the hand-assisted approach has shown benefit in patients with complicated diverticulitis and when utilized for more complicated procedures such as total abdominal colectomy and restorative proctocolectomy.
Alternative to conversion to laparotomy’if a surgeon needs to convert during a laparoscopic left colectomy, the hand-assisted approach offers an alternative to conversion to laparotomy.
There are no absolute contraindications to the utilization of the hand-assisted approach to a laparoscopic left colectomy. The goal is to perform a safe operation whether it is accomplished laparoscopically by hand assistance or by laparotomy. Conversions when preformed in a preemptive manner do not have a negative impact on outcomes (1,2). However, when performed reactively after a complication has occurred, the outcomes are worse than if the procedure had been performed open. There are several relative contraindications to the laparoscopic approach and they are centered on the fact of being able to progress through the operation in a safe manner (3).
Body mass index’Patient habitus, particularly intraperitoneal fat, is one of the best predictors for successful completion of a laparoscopic case. Intraperitoneal fat present makes manipulation of the bowel, its mesentery, and the omentum much more difficult. This problem can be overcome to some extent by the use of the hand.
Extensive adhesions’For patients with a prior history of abdominal surgery, the hand port incision is introduced to allow assessment of the adhesions before committing to
the laparoscopic approach. Extensive intraloop adhesions will require significant time to divide which may potentially lessen the benefit of the laparoscopic approach
Large inflammatory lesions’When the inflammation prevents the safe identification of landmarks and relevant anatomy, the risk of a reactive conversion significantly increases.
Medical issues’Disease such as COPD or cardiac disease needs special attention. The surgeon and anesthesiologist need to determine whether the patient can tolerate the pneumoperitoneum or the extremes of position. If there is evidence that cardiopulmonary function will be compromised, laparoscopy should be avoided.
The incision created for the hand port can be used to visualize the abdomen to determine the feasibility of laparoscopically completing the case.
The preoperative assessment of the patient is dependent upon the specific indication for the operation and should not alter even when an open, laparoscopic, or hand-assisted approach is utilized. The utilization of ureteral stents is left to the discretion of the surgeon and the indication for the procedure. There are two approaches to ureteral stents:
Routinely for ureteral identification
Selectively’utilizing them with the same criteria as used for laparotomy
Room Setup and Patient Position
Mechanical bed’The patient will be put in the extremes of position to facilitate the use of gravity to retract the small bowel.
Modified lithotomy position’The angle at the hip should be less than 10 degrees. Keeping the thigh low and knees adducted will minimize the interference of the patient’s thigh with the instruments during the procedure.
Bean bag’It is helpful to secure the patient to the operating room table. The most effective manner is with the use of a bean bag, which can be attached to the operating table with velcro. This step will allow both of the patient’s arms to be tucked to their side. The patient is them cocooned it the bean bag to prevent them from moving during the operation.
Surgeon’The surgeon stands on the patient’s right side. Typically, the surgeon will place his/her right hand through the port and will use the left hand to hold the laparoscopic instrument. Alternatively, the surgeon may stand between the patient’s legs, place his/her left hand through the hand port, and utilize a left lower quadrant port.
Camera operator’The assistant that operates the camera stands on the right side and to the head of the patient.
First assistant’If an assistant is available, they can stand between the patient’s legs and utilize the left lower quadrant port.
Monitors’The main viewing monitor is placed at the patient’s left flank. It should have the ability to move to the left shoulder when mobilizing the splenic flexure and to the left thigh when dissecting in the pelvis.
Port Placement
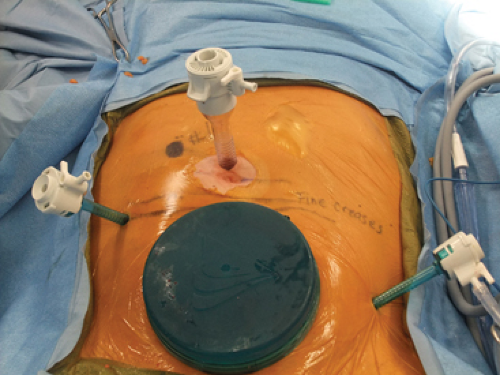
Hand port’The most effective site for placement of the hand port is in the suprapubic position (Fig. 12.1). This position helps to keep the hand out of the path of the camera and it puts the extraction site directly over the rectum to facilitate its division and in performing the anastomosis. The hand port can be placed through either a midline or Pfannenstiel incision.
Camera port’The camera port needs to be placed in the supraumbilical position so that it does not interfere with the skirt of the hand port.
Working ports’The main working port is placed in the right lower quadrant. It should be placed half way between the hand port and the camera port and lateral to the rectus muscle. A second working port is placed in the left lower quadrant, which should be lateral to the rectus and as low as possible. This port is used for retraction and division of the lateral attachments and mobilization of the splenic flexure. The lower it is placed, the lesser time there will be for working in reverse from the camera. A third working port can be placed in the right upper quadrant based on surgeon preference.
Technique
Accessing the retroperitoneum’The patient is placed in steep Trendelenburg and left side up. The small bowel is placed in the right upper quadrant. Using the medial to lateral approach, the superior rectal artery is grasped at the level of the sacral promontory with the surgeon’s right hand (Fig. 12.2A and B). A long incision is made in the peritoneum medial or below the artery. With a longer incision, the exposure of the retroperitoneum will be greater (Fig. 12.3A and B). Once the retroperitoneum is accessed, the sigmoid colon mesentery is elevated and the retroperitoneum is swept down so the left ureter can be identified (Fig. 12.4). After its identification, the left
ureter is then swept down and separated from the mesentery. If the ureter is not identified immediately, there are several alternative approaches. First, the retroperitoneum can be accessed at the level of the inferior mesenteric vein (IMV) (Fig. 12.5). The retroperitoneum is flat in this location. Once the proper plane is identified, it is developed in a caudad direction to connect with the space near the superior rectal artery. Second, the sigmoid colon can be mobilized in a lateral to medial direction to expose and identify the ureter. Finally, if all else fails, the top of the hand port can be removed and the ureter can be identified through the hand port in an open manner.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree