Fig. 2.1
Comprehensive overview of the complex pelvic floor anatomy (caudal view) of a female (Reproduced with permission from Zijta et al. [5])
The piriformis and obturator internus muscles that form the lateral walls of the pelvis are functionally considered as muscles of the lower limb.
Pelvic floor muscles have two major functions: they provide support or act as a “floor” for the abdominal viscera and constrictor or continence mechanism to the urethral, anal, and vaginal orifices (in females).
The skeletal muscles of the pelvic floor include the levator ani muscles complex (that consists of the pubococcygeus, the iliococcygeus, and the puborectalis), the coccygeus (or ischiococcygeus), the external anal sphincter, the striated urethral sphincter, and the deep and superficial perineal muscles. The muscles of the pelvic floor, particularly the levator ani muscles, have a critical role in supporting the pelvic visceral organs and play an integral role in urinary, defecatory, and sexual function.
Pelvic floor muscles have a constant resting tone except during voiding, defecation, and the Valsalva maneuver. This activity serves to close the urethral and anal sphincters, narrow the urogenital hiatus, and provide a constant support for the pelvic viscera. The constant muscle tone of the levator ani and coccygeus muscles prevents the ligaments becoming overstretched and damaged by constant tension [6]. The levator muscles and the skeletal components of the urethral and anal sphincters all have the ability to contract quickly at the time of an acute stress, such as a cough or sneeze, in order to maintain continence and to relax during evacuation.
2.3.1 Pelvic Diaphragm: Levator Ani and Coccygeus Muscles
The levator ani muscle is formed by the iliococcygeus, pubococcygeus, and puborectalis. These muscles can be identified as separate parts by their origin and direction [7,8]. The iliococcygeus originates from the posterior half of the arcus tendinous levator ani (ATLA), a linear thickening of the fascial covering of the obturator internus that runs from the ischial spine to the posterior surface of the ipsilateral superior pubic ramus. It inserts into the last two segments of the coccyx and in the midline of the anococcygeal raphe. The iliococcygeus forms a sheet-like layer and is often largely aponeurotic. The anococcygeal raphe is the interdigitation of the iliococcygeal fibers from both sides and extends from the coccyx to the anorectal junction.
The pubococcygeus originates from the anterior half of the tendinous arc and the periosteum of the posterior surface of the pubic bone at the lower border of the pubic symphysis and inserts on the midline visceral organs (vagina, urethra, anal sphincter complex), the perineal body, the anococcygeal raphe, and the inferior part of the coccyx. The pubococcygeus muscle (also called pubovisceral with the puborectalis) could be further subdivided into the puboperinealis, pubovaginalis, and puboanalis depending on its connections (Fig. 2.2).
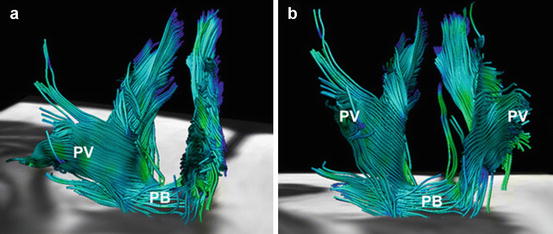
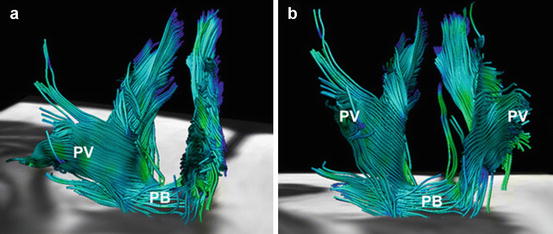
Fig. 2.2
Fiber tractography demonstrates the complex, multidirectional organization of the different pubovisceral (PV) muscle components in a 28-year old female subject in both oblique-anterior (a) and anterior-posterior view (b). At the bottom of the pelvic floor, transverse orientation of the fiber tracts are displayed matching the perineal body (PB) (Reproduced with permission from Zijta et al. [5])
The puborectalis also originates on the pubic bone, but its fibers pass posteriorly and go around the upper part of the anus, where it is attached posteriorly to the anococcygeal ligament, forming a sling around the vagina, the perineal body, and the anorectum and resulting in the anorectal angle. The puborectalis muscle promotes the closure of the urogenital hiatus in cooperation with the pubococcygeus muscle.
Although the puborectalis and external anal sphincter muscle form a functional unit in maintaining continence and has suggested a possible anatomical correlation [9], developmental studies provide evidence that the puborectalis is anatomically a part of the levator ani muscle [10]. The pubococcygeus and puborectalis muscle have intervening and inseparable muscle fibers at their pubic origin, whereas the puborectalis muscle and external anal sphincter muscle have no muscle fiber connection and are separated by connective tissue. Additionally, the puborectalis and external anal sphincter muscle appear at different time points during development [11] and have a different innervation.
The space between the levator ani musculature through which the urethra, vagina, and rectum pass is called the urogenital hiatus. The fusion of levator ani where they meet in the midline is called levator plate.
The fascia covering the levator muscles is continuous with the endopelvic fascia above, perineal fascia below, and obturator fascia laterally.
The arcus tendinous fascia pelvis is a thickening in the obturator fascia and extends from the pubis anteriorly to the ischial spine, providing attachment to the paravaginal connective tissue. Arising from a similar location on the pubis but extending superior to the arcus tendinous fascia pelvis is a thickening of levator ani fascia called arcus tendinous levator ani, which is the origin of the levator ani muscle.
Although most anatomy and surgical texts depict the levator ani muscles as a bowl or funnel-shaped, this reflects the uncontracted state of the muscles as might be seen in a cadaver dissection and not that of a normally functioning levator. In a woman with normal pelvic floor function, the levator ani muscle complex in its tonically contracted state has an intricate three-dimensional structure in which its anterior portion (pubococcygeus and puborectalis) is oriented vertically as a sling around the mid-urethra, vagina, and anorectum and its posterior portion (the iliococcygeus) has a horizontal upwardly biconvex shape resembling a butterfly wing.
Thus, the anterior portion of the levator ani complex serves to close the urogenital hiatus and pull the urethra, vagina, perineum, and anorectum toward the pubic bone, whereas the horizontally oriented posterior portion (levator plate) serves as a supportive diaphragm or “backstop” behind the pelvic viscera.
Loss of normal levator ani tone, through denervation or direct muscle trauma, results in laxity of the urogenital hiatus, loss of the horizontal orientation of the levator plate, and a more bowl-like configuration.
These changes can be bilateral or asymmetric [12].
The coccygeus muscle (also called ischiococcygeus) extends from the ischial spine, courses along the posterior margin of the internal obturator muscle laying on the anterior surface of the sacrospinous ligament, inserts to the lateral part of the coccyx and the lower sacrum, and forms the posterior part of the pelvic diaphragm.
The sacrospinous ligament is at the posterior edge of the coccygeus muscle and is fused with this muscle. The proportions of the muscular and ligamentous parts may vary. The coccygeus is not part of the levator ani, having a different function and origin.
Although the muscles of the pelvic floor were initially thought to have innervation both from direct branches of the sacral nerves on the pelvic surface and via the pudendal nerve on the perineal surface, recent evidences indicate that these standard descriptions are inaccurate and that the levator ani muscles are innervated solely by a nerve traveling on the superior (intrapelvic) surface of the muscles without contribution of the pudendal nerve [13–15]. The nerve supplying the coccygeus muscle and the levator ani muscles (all three) originates from S3, S4, and/or S5. Occasionally, a separate nerve comes directly from S5 to innervate the puborectalis muscle independently.
2.3.2 Perineum, Perineal Membrane, and Perineal Body
Although the area between the vagina and anus is described clinically as the “perineum,” anatomically the perineum is the entirety of the pelvic outlet inferior to the pelvic floor.
The borders of the female perineum are the ischiopubic rami, ischial tuberosities, sacrotuberous ligaments, and coccyx. A line connecting the ischial tuberosities divides the perineum into the urogenital triangle anteriorly, which includes the female external genitalia and is characterized by the perineal membrane, and the anal triangle posteriorly, which contains the anal orifice and the posterior part of the perineum.
In the standing position, the urogenital triangle is oriented horizontally, whereas the anal triangle is tilted upward so that it faces more posteriorly.
Directly below the pelvic diaphragm is the perineal membrane, a triangular-shaped dense fibromuscular tissue that spans the urogenital triangle and attaches laterally to the ischiopubic rami, posteriorly to the perineal body, medially to lateral walls of the vagina and urethra, and apically to the arcuate pubic ligament.
In women, the perineal membrane is traversed by the urethra and vagina through a hiatus (the urogenital hiatus), and the membrane is attached to the lateral vaginal walls. In men, it is a continuous sheet.
Formerly the perineal membrane was named “urogenital diaphragm” and considered to constitute a tri-layered structure of the deep transverse perinei with a superior and inferior fascia. Although historically anatomists and clinicians have used the term urogenital diaphragm to describe this structure, this term has been abandoned because it erroneously implies a muscular diaphragm rather than a thick sheet of connective tissue [16,17].
Moreover, present insights indicate the presence of a musculofascial uni-layer structure. The presence of the superior fascia and deep transverse perinei is questionable [18], and muscle fibers previously considered to constitute the urogenital diaphragm most likely are part of the urethra support mechanism (compressor urethrae and urethrovaginalis part of the external urethral sphincter muscle).
The perineal membrane consists of a ventral and a dorsal component [19].
The ventral component is continuous with the paraurethral and paravaginal connective tissues and arcus tendinous fascia pelvis. It provides attachment to the female striated urogenital sphincter muscles and the vestibular bulbs and clitoris fuse to its inferior surface. The dorsal component attaches laterally to the ischiopubic rami on each side and medially to the vagina and the perineal body.
The urogenital triangle is divided into a superficial and deep perineal space by the perineal membrane.
The superficial perineal space lies between the perineal membrane and the subcutaneous tissues and contains the superficial perineal muscles (ischiocavernosus, bulbospongiosus or bulbocavernosus, superficial transverse perineal muscles), the erectile tissue of the clitoris, the vestibular bulbs, and Bartholin’s glands.
The superficial transverse perinei, the bulbospongiosus, and the ischiocavernosus are the external genital muscles and form the most superficial component of the pelvic floor. The superficial transverse perinei that originate from the ischial tuberosity on each side and insert on the perineal body has a supportive function; the bulbospongiosus and the ischiocavernosus play a role in sexual function. The ischiocavernosus muscle arises from the ischial tuberosity and the clitoral crura along the inferior portion of the ischiopubic ramus and inserts on to the body of the clitoris. The bulbocavernosus muscle runs on either side of the vagina and attaches to the perineal body posteriorly and the body of the clitoris anteriorly.
The superficial transverse perinei spans the posterior edge of the perineal membrane and inserts at the external sphincter and perineal body or point.
In women, the superficial transverse perineal muscle is directly superior to the external sphincter, often with some overlap. In men, the superficial perineal muscle is directly anterior to the external sphincter.
The superficial Colles fascia of the urogenital triangle forms a clear, surgically recognizable plane beneath the skin of the anterior perineum. It is firmly attached posteriorly to the fascia over the superficial transverse perinei and the posterior limit of the perineal membrane. Laterally, it is attached to the margins of the ischiopubic rami as far back as the ischial tuberosities. From here it runs more superficially to the skin of the urogenital triangle, lining the external genitalia before running anteriorly into the skin of the lower abdominal wall where it is continuous with the membranous fascia of Scarpa.
The deep perineal space lies just deep to the perineal membrane and inferior to the levator ani muscles. Within this thin space lie the external urethral and the urethrovaginalis sphincter, compressor urethrae, and deep transverse perineal muscles [20].
These muscles lie superior to the perineal membrane in the deep perineal space that is continuous with the pelvic cavity. The superior fascia of these muscles is continuous with the endopelvic fascia.
The urethrovaginalis and compressor urethrae muscles provide accessory sphincter function to the urethra. The urethrovaginalis muscle surrounds the distal urethra and vagina without passing between them and therefore acts as a sphincter to the vagina as well as to the distal urethra. The deep transverse perineal muscle, along with its superficial counterpart, serves to stabilize the position of the perineal body and inferior border of the perineal membrane.
The pudendal nerve is the main sensory and motor nerve of the perineum. It arises from the ventral rami of S2–S4 (with S3 providing the largest contribution), runs underneath the piriformis, and exits the pelvis through the greater sciatic foramen. It passes just behind the ischial spine and reenters the pelvis through the lesser sciatic foramen. The pudendal nerve then runs in the Alcock’s canal (pudendal canal) in the obturator fascia and ventral to the sacrotuberous ligament before separating into several terminal branches that terminate within the muscles and skin of the perineum [21,22]. As it enters the perineum, the pudendal nerve lies on the lateral wall of the ischiorectal fossa and divides into three branches: the inferior rectal, perineal, and dorsal nerve of the clitoris [23]. The dorsal nerve of the clitoris lies on the perineal membrane along the ischiopubic ramus and on the anterolateral surface of the clitoris, one on each side, and supplies the clitoris. The perineal nerve divides into several branches and supplies the bulbocavernosus, ischiocavernosus, superficial transverse perineal muscles, and the skin of the medial portion of labia majora, labia minora, and vestibule.
The perineal body (also named the central perineal tendon) is a pyramidal fibromuscular structure in the midline between the anus and vagina with the rectovaginal septum at its cephalad apex. It marks the point of convergence of the bulbospongiosus muscle, superficial and deep transverse perinei, perineal membrane, external anal sphincter, posterior vaginal muscularis, and fibers from the puborectalis and pubococcygeus. It represents a connection point between superficial and deep muscles of the pelvic floor [24] and plays an important role in support of the distal vagina and in normal anorectal function.
It has been suggested that the perineal body is not the site of insertion of perineal muscles but the site along which muscle fibers of these muscles and the external anal sphincter pass uninterrupted from one side to the other [25].
Acquired weakness or damages of the perineal body may predispose the pelvic organs to defects such as rectocele, prolapse, and enterocele [17,25,26].
Sex-related differences in perineal structures included a more superiorly located superficial transverse perineal muscle in women than in men. The central perineal tendon in men is a central muscular insertion point, with a cleavage plane with external anal sphincter; in women, it represents an area where muscle fibers converge, decussate, and imbricate [27], and there is no clear boundary between the perineal body and external sphincter.
Moreover, the perineal body could be considered as the center of female perineum and pelvic floor, while in male it is slightly more anterior and the anus is in a central position.
2.3.3 Urethral Sphincter Complex and Urethral Continence Mechanism
The urethra is a small complex tube with a mucous membrane that connects the urinary bladder to the genitals for the removal of fluids to the exterior of the body [28].
After leaving the bladder, the male urethra travels through the center of the prostate gland, enters the base of the penis, and ends as a urinary meatus at the tip of the penis. The average length of the male urethra is about 22 cm [29].
In females, the urethra is shorter (is about 3.5–4 cm long and averages 6 mm in diameter), slightly curved, and lies directly behind the symphysis pubis. After leaving the bladder it passes from the retropubic space, perforates the perineal membrane, and ends with its external orifice in the vestibule directly above the vaginal opening [30]. Throughout most of its length, the urethra is fused to the anterior vaginal wall. Although in females the urethra is used only for urinating, the relationship of the urethra with the vagina is functionally important to the muscular pelvic floor [31].
Histologically, the urethra has four distinct layers: mucosa, submucosa, smooth muscle internal urethral sphincter (IUS), and striated external urethral sphincter (EUS) (Fig. 2.3).
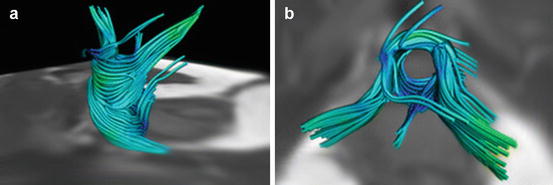
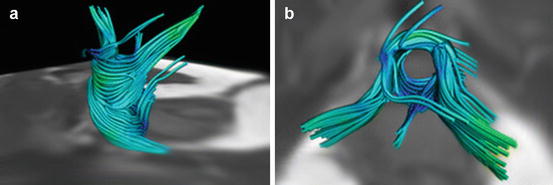
Fig. 2.3
Fiber trajectories reflecting the urethral sphincter complex with an anterolateral (a) and cranial view (b) (Reproduced with permission from Zijta et al. [5])
The urethral mucosa extends from the bladder transitional epithelium to the external meatus and is primarily nonkeratinizing squamous epithelium. It is derived from the urogenital sinus along with the lower vagina and vestibule. It is hormonally sensitive and undergoes changes with stimulation [32]. The hormonally sensitive submucosal tissue contains a rich and prominent vascular plexus. These vascular cushions, along with the urethral mucosa, provide a watertight closure of the mucosal surface with an increase in blood flow that may occur with an increase in pressure on abdominal vessels [33] and account for approximately one-third of the urethral resting tone, while the internal and external urethral sphincters account for the remainder [34].
The IUS is located at the inferior end of the bladder and the proximal end of the urethra, and it is contiguous with that of the detrusor, forming a horseshoe-like arrangement with oblique and longitudinal smooth muscle fibers, with a few circularly oriented outer fibers [35].
The function of the longitudinal smooth muscle fibers is probably related to a filler volume control, and their presence may improve the efficiency of the sphincter mechanism by allowing closure of the urethral lumen with only a small amount of circular muscle shortening [36].
Because the IUS is composed of smooth muscle, it is not under voluntary control and is controlled through the autonomic nervous system [37].
The skeletal muscle component of the urethral sphincter consists of the external urethral sphincter (also called sphincter urethrae) along with the previously described compressor urethrae and urethrovaginalis muscles. These three muscles, which function as a single unit, have been called striated urogenital sphincter [20]. Together, they are approximately 2.5 cm long and encircle the urethra in its midportion from just below the bladder neck to the perineal membrane within the deep perineal space. They are located at the distal inferior end of the bladder in females [38] and at the level of the membranous urethra and the distal prostate in males [39].
The striated urogenital sphincter provides approximately one-third of the urethral resting tone and is responsible for the voluntary and reflex increases in intraurethral pressure needed to maintain continence. Unlike the IUS, the EUS is mainly composed of skeletal muscle and it is voluntarily controlled through the somatic nervous system [40]. The EUS plays a role in squeezing the urethra and closing where the urethra exits the body.
In female, where the EUS is more elaborate and the urogenital sphincter system more evident, the urethral sphincter surrounds the urethra in the middle third of its length, starting from the base of the bladder and as a continuation of the peripheral component of the compressor urethral muscle.
The compressor urethral muscle fibers begin as a small tendon attaching to the ischiopubic ramus in the lateral side. This muscle expands to the anterior surface of the urethra and is a continuation of the corresponding fibers of the opposite side of the body. It then forms a broad arcing muscle. The role of the compressor urethral muscles is to squeeze the urethra from its ventral part. This muscle can affect pulling caudally and inferiorly the urethral meatus and assist the urethral elongation as a way of providing continence. The urethrovaginal sphincter is a thin, flat, and broad muscle that intermingles ventrally with the compressor urethral muscle. These muscle fibers begin on the ventral side of the urethra and extend dorsally along the lateral wall of the urethra and the vagina to the beginning of the vestibular bulb. These fibers are continuous with the posterior vagina and correspond to the muscle of the opposite side. The contraction of these fibers leads to constriction of both the vagina and the urethra [41,42].
In male, the muscle fibers inferior to the caudal prostate are circular and form the external sphincter of the membranous urethra. The external fibers arise from the junction of the inferior rami of the pubis and ischium. The external sphincter lies in the urogenital hiatus of the pelvic diaphragm, and the EUS fills the area between the pudendal canals below the pelvic diaphragm [41]. The external sphincter muscle is surrounded by fibrous integument. This fibrous integument is a continuation of the prostatic sheath, which is derived from extraperitoneal connective tissue.
In addition to the muscular and vascular tissue of the urethra, there is a considerable quantity of connective tissue interspersed within the muscle and submucosa. This tissue contains collagen and elastin fibers and is thought to add to urethral closure passively. Lastly, a series of glands are found in the submucosa, mainly along the vaginal surface of the urethra [43]. They are most predominant in the middle and lower third of the urethra.
Normal urethral function depends upon normal support of the urethra as well as its intrinsic sphincter mechanism. As with vaginal support, dynamic interaction between the levator ani muscle complex and the connective tissue supports of the urethra is essential.
The requirements for continence, according to a hammock-like supportive system, include a quiescent bladder, functioning musculofascial supports (composed of periurethral endopelvic fascia and anterior vaginal wall), and a functional urethral sphincter mechanism [44], where urethral support is provided by a coordinated action of fascia and muscles acting as an integrated unit under neural control. The fascial attachments connect the periurethral tissue and anterior vaginal wall to the arcus tendinous at the pelvic sidewall, whereas the muscular attachments connect the periurethral tissue to the medial border of the levator ani. This musculofascial support provides a hammock onto which the urethra is compressed during increases in intra-abdominal pressure. Increased intra-abdominal pressure, as with a cough or sneeze, causes compression of the urethra against this hammock-like layer, thereby compressing the urethral lumen closed. The stability of the suburethral layer depends on the intact connection of the anterior vaginal wall and its connective tissue attachments to the arcus tendinous fasciae pelvis and levator ani muscles. These attachments allow the pelvic floor muscle’s normal resting tone to maintain the position of the urethra and bladder neck. They are also responsible for the posterior movement of the vesical neck seen at the onset of micturition (when the pelvic floor relaxes) and for the elevation noted when a patient is instructed to arrest her urinary stream. Defects in these attachments can result in proximal urethral support defects (urethral hypermobility) or anterior vaginal wall prolapse (cystocele) and can contribute to stress urinary incontinence [2].
Furthermore, failure of one of the support components will not invariably produce stress incontinence because of the compensatory effect of the other components. This may explain why some women with hypermobility have no incontinence.
The innervation of the urethral sphincter is from both the somatic and the autonomic nervous systems.
The striated sphincter is innervated by the pudendal nerve from the S2 to S4 nerve roots.
The sympathetic innervation of the bladder begins at the lower thoracic and upper lumbar spinal cord segments (T10 to L2) and results in the closing of the IUS. Parasympathetic activity causes the bladder to contract and allows the internal sphincter to open [45]. The combination of functional innervations via the somatic pudendal nerve and autonomic innervation manages urination.
2.3.4 Anal Sphincter Complex and Anal Continence Mechanism
The anal sphincter complex can be considered as a multilayered cylindrical structure, with a smooth internal sphincter, the intersphincteric space with the longitudinal layer, and the outer striated external muscle layer (Fig. 2.4). The normal anal canal length is between 3 and 6 cm, depending on gender and age, but the functional anal canal (high-pressure zone) is slightly shorter. Relevant sex-related differences included a significantly shorter external sphincter in women than in men both laterally and anteriorly [27].
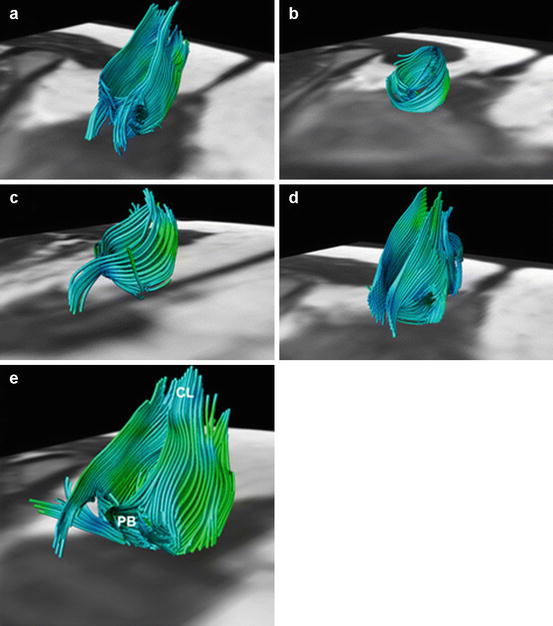
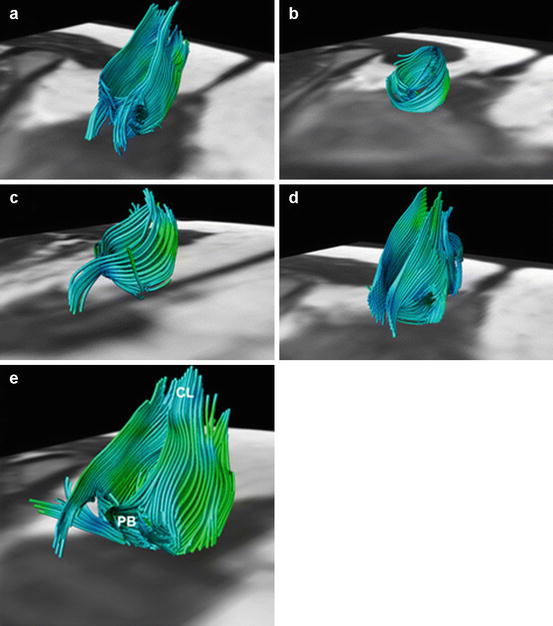
Fig. 2.4
Fiber trajectories representing the anal sphincter complex in five female subjects: 28, 32, 24, 27, and 31 years of age, respectively (a–e). Not all extrapolated fiber trajectories, matching the appearance of the anal sphincter complex, were perfectly circularly orientated. This might be attributed to both the predefined fiber angle cutoff point and the potential inaccurate fiber tractography based on signal originating from various muscles and ligamentous structures converging and interweaving in this area (e.g., perineal body (PB) and coccygeal ligament (CL)) (e) (Reproduced with permission from Zijta et al. [5])
Circular muscle layer of the rectum expands caudally into the anal canal and becomes the internal anal sphincter (IAS). The circular muscles in the sphincteric region are thicker than those of the rectal circular smooth muscle, about 2–5 mm, crossed by septa in between the muscle bundles.
The internal sphincter, about 3 mm in length and shorter than the external anal sphincter, does not extend to the lower edge of the anal canal but ends approximately 1 cm above this level. The lower muscular part of the anal sphincter therefore is only constituted by the external sphincter.
The internal sphincter has an intrinsic, sinusoidal “slow wave” activity with a frequency of 20–40 cycles per minute and is primarily responsible for the resting tone of the anus [46]. It contributes about 85 % of the resting anal sphincter pressure, which is measured at between 40 and 90 mmHg in health [47]. Weakness or disruption of the internal anal sphincter results in the passive leakage of fecal contents and incontinence of flatus [48].
Similarly to the IAS, the longitudinal muscles (LM) of the rectum extend into the anal canal in the space between the IAS and the external anal sphincter EAS. The longitudinal layer receives contributions from the levator ani, particularly the puboanalis [49,50], so it is also referred to as the conjoined tendon (muscle).
The structural function of LM consists in connecting the visceral and somatic parts of the anal sphincter complex. The LM may give rise to medial extensions that cross the internal anal sphincter to contribute to the smooth muscle of the submucosa (musculus canalis ani, sustentator tunicae mucosae, Treitz muscle, musculus submucosae ani) [51]. Fine and Lawes also described a longitudinal layer of muscle lying on the inner aspect of the internal sphincter arising from the conjoined longitudinal muscle and named it muscularis submucosae ani [52]. Moreover, some fibers of the longitudinal muscle that traverse the internal sphincter and become inserted just below the anal valves anchoring the submucosa were called by Parks mucosal suspensory ligament [53]. Other fibers cross the subcutaneous part of the EAS to become the muscle corrugator ani. Some authors consider that the meshwork formed by the conjoined longitudinal muscle may minimize functional deterioration of the sphincters after surgical division and act as a support to prevent hemorrhoidal and rectal prolapse [54,55].
Histologically, ganglionic cells and Vater-Pacinian-like corpuscles can be identified inside the LM. Morphology, topography, and histology of the LM suggest that this muscle also participates in maintaining anorectal continence, probably with a sensitive function of control related to anal canal distension.
The external sphincter is a cylindrical striated muscle under voluntary control that constitutes the outer layer of the anal sphincter complex and comprises fast and slow twitch types, which allow it to maintain sustained tonic contraction at rest and also allow it to contract rapidly with voluntary squeeze.
However, the EAS contributes a small part to the resting anal tone [47]. Rather, in its primary function of voluntary contraction, pressures of between 50 and 200 mmHg can be generated (approximately double than the resting pressure), significantly reduced in case of denervation or damages, as in obstetric injuries [56].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





