CHAPTER 18 Female Incontinence and Vesicovaginal Fistula
![]() Define urinary incontinence.
Define urinary incontinence.
Urinary incontinence is the complaint of any involuntary leakage of urine and is considered to be a storage symptom. This is often socially embarrassing and impacts negatively on a patient’s quality of life. It is important to confirm the fluid lost as urine and rule out fluid from another source, that is, peritoneal or uterine. Furthermore, one must identify the urine is per urethra and not from a urinary fistula or ectopic ureter. In addition, urinary leakage may need to be distinguished from sweating or vaginal discharge.
![]() What are other storage symptoms as defined by the International Continence Society?
What are other storage symptoms as defined by the International Continence Society?
• Frequency is the complaint by the patient who considers that he/she voids too often by day. Although variable in nature (fluid intake, comorbidities, and hours of sleep), frequency can be defined as voiding > 8 times in a 24-hour period.
• Nocturia is the complaint that the individual is interrupted from sleep to void one or more times.
• Urgency is the complaint of a sudden compelling desire to pass urine, which is difficult to defer. It can be difficult to measure.
• It is important to further characterize these symptoms with a 1- or 3-day bladder diary recording of micturition episodes, voided volumes, and fluid intake.
![]() Describe the symptoms associated with the various types of urinary incontinence.
Describe the symptoms associated with the various types of urinary incontinence.
• Urge urinary incontinence is the complaint of involuntary leakage accompanied by or immediately preceded by urgency.
• Stress urinary incontinence is the complaint of involuntary leakage on effort, exertion, sneezing, or coughing.
• Mixed urinary incontinence is the complaint of involuntary leakage associated with urgency in addition to exertion, effort, sneezing, or coughing.
• Continuous urinary incontinence is the complaint of continuous involuntary loss of urine.
• Nocturnal enuresis is the complaint of involuntary loss of urine that occurs during sleep.
• Postvoid dribble is the term used to describe involuntary loss of urine after voiding, usually after rising from the toilet.
• Overflow incontinence is any involuntary loss of urine associated with overdistension of the bladder.
![]() Can stress incontinence induce urge incontinence?
Can stress incontinence induce urge incontinence?
Yes. Urgency may result from compensatory responses initiated in the incontinent patient. For example, once the initial symptom of stress incontinence is noticed, the patient may urinate frequently to keep the bladder empty, thus reducing the chance of stress-related incontinent episodes. As the bladder accommodates to these lower volumes, decreased bladder capacity and/or compliance may ensue. Subsequently, when the bladder distends beyond its reduced functional capacity, the patient experiences sensory urgency, frequency, and urinary incontinence.
Alternatively, urgency as a physiologic response may be a product of urine passage into the proximal urethra. This activates somatic afferent nerves in the pudendal nerve that produce a detrusor contraction by activating the pontine micturition center through the micturition reflex and the resultant stress leakage, termed “stress-induced detrusor overactivity.” Correction of the stress incontinence may eliminate the urgency.
![]() List the components of normal urinary continence in response to increases in abdominal stress.
List the components of normal urinary continence in response to increases in abdominal stress.
Normal continence in the female is a product of several forces working together. These forces include the proper anatomic location of the sphincteric unit, the critical functional and anatomic urethral length, the mucosal coaptation of the urethral surface, and the increased urethral pressure generated by reflex pelvic contractions at the time of stress. Failure of one of the components of this delicate balance will not invariably produce stress incontinence because of the compensatory effect of the other forces.
![]() Describe the urethral “washer effect.”
Describe the urethral “washer effect.”
The female urethra consists of a 4-cm tube of inner epithelium and outer muscularis. The infolded epithelium is enclosed by a rich vascular sponge, which in turn is surrounded by a fibromuscular and smooth muscle coat. This submucosa, consisting of loosely woven connective tissue scattered throughout with smooth muscle bundles and an elaborate vascular plexus, provides a compressive “washer effect” vital to the mechanism of continence. The effectiveness of this washer is thought to be estrogen dependent.
![]() List the structures that compose the female sphincteric unit.
List the structures that compose the female sphincteric unit.
The sphincteric unit has an internal and external sphincter. The internal sphincter, involuntary smooth muscle, is located at the bladder neck. The external sphincter is located at the midurethral complex which consists of skeletal muscle (slow and fast twitch) that is under voluntary control.
![]() List the structures that provide normal pelvic support.
List the structures that provide normal pelvic support.
• The fascia of the pelvic floor may be collectively referred to as the levator fascia or endopelvic fascia. Although the fascia works in an integrated fashion to provide pelvic support, certain areas of the fascia have been separately described because of their importance in supporting individual female pelvic structures.
• The pubourethral ligaments connect the midportion of the urethra with the inner surface of the inferior pubis. Laterally, this midportion of the urethra is supported by segments of the levator fascia just below their attachments to the pubis. Collectively, these may be referred to as the midurethral complex.
• The urethropelvic ligaments (periurethral fascia) connect the proximal urethra and bladder neck laterally to the tendinous arch of the obturator muscle.
• The vesicopelvic ligaments (pubocervical fascia) connect the bladder base laterally to the tendinous arch of the obturator muscle.
• The cardinal-sacrouterine ligaments connect the uterine cervix and isthmus to the sacral vertebrae.
• The broad ligaments connect the uterine body to the pelvic sidewall.
![]() Describe outlet abnormalities associated with urinary incontinence.
Describe outlet abnormalities associated with urinary incontinence.
Urethral hypermobility: The pelvic floor fails to support the vesical neck and proximal urethra. This results in either the vesical neck and proximal urethra being situated below the inferior margin of the symphysis pubis at rest or they descend from a position situated above the inferior margin of the symphysis pubis during strain.
Intrinsic sphincter deficiency (ISD): The internal urethral sphincter fails to maintain continence even at low detrusor pressures (0—60 cm H2O) with resultant leakage of urine per urethra.
![]() Define detrusor overactivity.
Define detrusor overactivity.
Detrusor overactivity is a urodynamic observation characterized by involuntary detrusor contractions during the filling phase, which may be spontaneous or provoked. It can be further classified as either neurogenic detrusor overactivity when there is a relevant neurological condition (previously termed “detrusor hyperreflexia”) or idiopathic detrusor overactivity when there is no defined cause (previously termed “detrusor instability”).
![]() Is urge incontinence the same as detrusor overactivity?
Is urge incontinence the same as detrusor overactivity?
Sometimes. Urge incontinence implies involuntary bladder contractions that may or may not be associated with urine leakage. These may not be identifiable on urodynamics given that patients can suppress involuntary contractions.
![]() What is bladder compliance?
What is bladder compliance?
Bladder compliance describes the relationship between bladder volume and detrusor pressure and is dependent upon the viscoelastic properties of the detrusor. Compliance is calculated by dividing the change in volume by the change in detrusor pressure during 2 specific points at the time of filling cystometry: (1) at the start of the bladder filling and (2) at cystometric capacity or immediately before the start of any detrusor contraction that causes significant leakage. The result is expressed in mL/cm H2O.
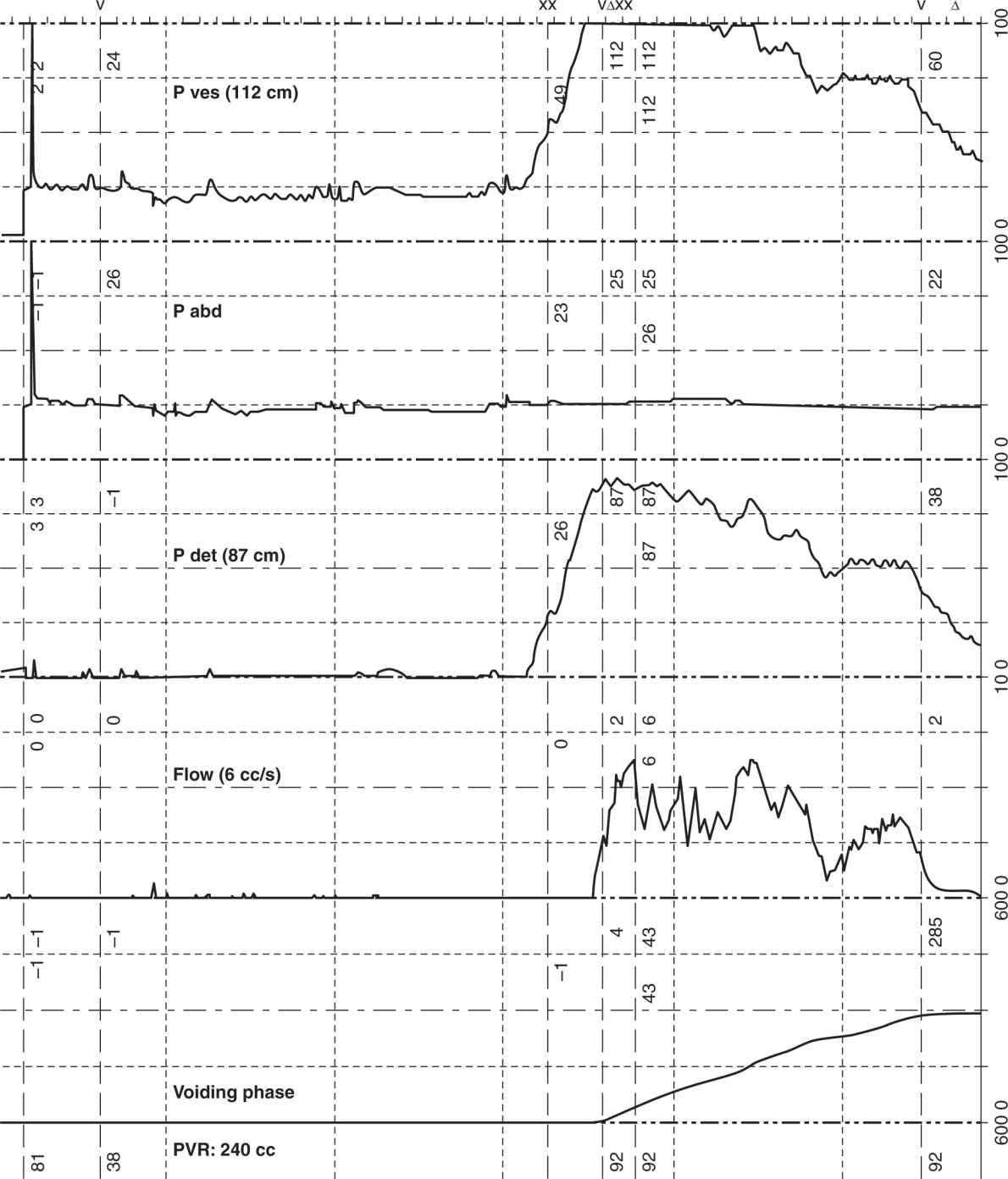
![]() Distinguish between abdominal, Valsalva, and detrusor leak point pressures (LPP).
Distinguish between abdominal, Valsalva, and detrusor leak point pressures (LPP).
Abdominal/Valsalva LPP: Intravesical pressure at which urine leakage occurs due to increased abdominal pressure in the absence of a detrusor contraction. In the normal patient, urine loss should never occur during abdominal straining even at high pressures.
Detrusor LPP: Lowest detrusor pressure at which urine leakage occurs in the absence of either a detrusor contraction or increased abdominal pressure. In the normal patient, urine exits the urethra at relatively low bladder pressures during voiding. A detrusor LPP greater than 40 cm H2O has been used to identify patients with neurologic abnormality who may be at risk for upper tract damage. Detrusor LPP can be measured during involuntary detrusor contraction in patients with detrusor overactivity.
![]() What is the role of the history?
What is the role of the history?
Because urinary symptoms may be similar despite disparate etiologies, the history is often nondiagnostic when considering female urinary incontinence. There is a 30% error in diagnosing stress urinary incontinence if only the history is used. Evaluation of the incontinent female must include a history, physical examination, and adjuvant testing. However, because more than one symptom is often present, it is essential to determine the relative severity of each complaint. It is important to focus on the chief presenting symptom in deciding the next diagnostic or therapeutic step.
![]() Describe the key components of an initial evaluation of female urinary incontinence.
Describe the key components of an initial evaluation of female urinary incontinence.
• Q-tip test: Assesses mobility of the urethra. With stress, the tail of the applicator will transcribe an arc of 0° to 30° in most women. Movement of greater than 35° suggests urethral hypermobility.
• Stress testing: Assesses urethral leak with stress. With the bladder full (ie, at least 200—300 mL), the patient is asked to cough or strain. The patient with stress incontinence will immediately lose urine as a brief, small squirt associated with the stress. The position is variable. Eighty percent of patients will leak in the lithotomy position; an additional 10% of patients will leak at an incline of 45°, while the final 10% of patients will only leak in the standing position.
• Speculum examination: Assesses concomitant pelvic floor defects. Urethral hypermobility may be measured with a Q-tip, but a speculum exam is necessary to evaluate the anterior vaginal wall, the vaginal apex, an enterocele, a rectocele, the anal sphincter, and the perineal body.
• Bladder or voiding diary: Measures the voided volumes, daytime frequency, incontinence episodes, pad usage, and other information such as fluid intake, degree of urgency, and leakage during a defined period (ie, 1- or 3-day interval).
• Pad testing: Assesses the quantity of urine lost during incontinence episodes; methods range from a short provocative test to a 24-hour pad test. Increase of > 15 g in pad weight gain is considered abnormal.
• Postvoid residual: Assesses volume of urine left in bladder after voiding by either an ultrasound bladder scanner or straight catheterization.
![]() What are the AUA guidelines for initial evaluation for female stress incontinence?
What are the AUA guidelines for initial evaluation for female stress incontinence?
• Standards: Focused history and physical, objective demonstration of SUI, PVR, U/A C/S if indicated.
• Recommendation: Characterization of incontinence (stress, urge), frequency and severity, impact on lifestyle expectations of treatment, and additional diagnostic testing if indicated (pad test and/or voiding diary, urodynamic, cystoscopy, and imaging).
![]() What are the indications for urodynamic testing?
What are the indications for urodynamic testing?
• When there is mixed urinary incontinence and the component of stress incontinence is not predominant to the urge incontinence. (A randomized control trial, the VALUE study, suggests that preoperative urodynamics does not affect outcomes or the surgical approach for uncomplicated stress predominant incontinence.)
• When initial evaluation and results of simpler diagnostic tests have been inconclusive.
• When empirical treatments have proved unsuccessful.
• When the patient complains of incontinence but it cannot be demonstrated clinically.
• In symptomatic patients who have previously undergone corrective surgery.
• In patients with an elevated postvoid residual.
• In patients with a history of prior radical pelvic surgery or radiation.
• In patients with known or suspected neurologic disorders to rule out upper tract damage.
• When assessing urethral function (ISD).
• When Grade III or greater pelvic organ prolapse (POP) is present.
• In patients where voiding dysfunction is suspected.
![]() During urodynamic testing of a female with clinically demonstrable stress incontinence, you find that she does not leak with a catheter in place. What should be done next?
During urodynamic testing of a female with clinically demonstrable stress incontinence, you find that she does not leak with a catheter in place. What should be done next?
The catheter should be removed as there is a 50% chance that the patient will leak during urodynamic testing.
![]() What are the indications for cystoscopy?
What are the indications for cystoscopy?
In all patients with urgency as a complaint, bladder pathology such as bladder stone, bladder diverticula, bladder cancer, and carcinoma in situ must be ruled out. All patients with hematuria or sterile pyuria should undergo cytologic examination, cystoscopy, and upper tract evaluation. It is more controversial, but patients with pure stress urinary incontinence may undergo preoperative cystoscopy to evaluate for incidental coexisting disease if suspected, especially those with history of radiation, prior pelvic, or incontinence surgery.
![]() Describe several radiographic evaluations useful in assessing female urinary incontinence.
Describe several radiographic evaluations useful in assessing female urinary incontinence.
• Cystogram with voiding films (VCUG): Often obtained videourodynamics, these tests are useful in comparing resting and straining films. Lateral films are helpful in identifying urethral position at rest and hypermobility with straining. These standing lateral films are also useful in assessing the degree of cystocele if present. Urinary leak may be observed on the lateral straining films.
• Ultrasound: Useful in identifying urethral mobility and prolapse, ultrasound can be performed transabdominally, transrectally, or transvaginally. The quality of the examination is highly dependent upon the skills of the ultrasonographer.
• MRI: Usually reserved for cases of more severe prolapse, the dynamic MRI of the pelvis is very helpful in identifying cystocele, uterine prolapse, and rectocele. It is also useful in revealing any concomitant pelvic pathology when hysterectomy is being considered as part of pelvic repair. Use of the HASTE sequence MRI is particularly helpful in identifying urologic pathology.
![]() What is the role of Kegel exercises and estrogens in female urinary incontinence?
What is the role of Kegel exercises and estrogens in female urinary incontinence?
• Kegel exercises: If performed properly and diligently, Kegel exercises can strengthen the levator musculature, which can lead to an increase in urethral pressure, better urethral reflex response to stresses, reduction of cystocele, and improved cough-urethra pressure transmission in stress urinary incontinence. These exercises are also useful for urge incontinence. By increasing pudendal activity to the sphincter muscles, this may in turn stimulate a reflexive inhibitory input to the detrusor, thereby suppressing involuntary bladder contractions.
• Estrogens: Lack of estrogen causes the urethral mucosa and underlying blood vessels to atrophy, leading to a decreased compressive washer effect. Estrogen causes hypertrophy and thickening of the urethral mucosa and engorgement of the blood vessels beneath. Estrogen should be given vaginally for optimal improvement of OAB symptoms and urge incontinence. Studies have failed to show an improvement of SUI with estrogen replacement.
![]() Identify several behavioral modifications which should be offered as first-line standard treatments for a woman with urge incontinence.
Identify several behavioral modifications which should be offered as first-line standard treatments for a woman with urge incontinence.
• Kegel exercises or pelvic floor muscle training: see above.
• Timed voiding: Instruct the patient to void on a timed schedule. The specific interval should be based on voiding before the development of urgency. Increase the interval after several weeks without urgency.
• Prompted voiding: Instruct the patient not to delay voiding. Additionally, the patient must concentrate on completely relaxing and emptying the bladder during the void.
• Fluid restriction: Limit the fluid intake for patients to 4 to 6 glasses per day. Avoid caffeine-containing beverages and fluid consumption after dinner.
• Avoidance of bladder irritants: Eliminate bladder irritants such as alcohol and caffeine, which can exacerbate lower urinary tract symptoms and have a diuretic effect.
![]() List the various pharmacologic treatments for a woman with urge incontinence.
List the various pharmacologic treatments for a woman with urge incontinence.
• Anticholinergics: AUA guidelines recommend anticholinergics as a (standard) treatment with extended release preferred over immediate release to minimize side effects. They antagonize the muscarinic receptors of the bladder resulting in increased total bladder capacity, decreased amplitude of bladder contraction, and increased bladder volume before first bladder contraction.
• B3 agonists (Mirabegron): Selectively activates the B3 receptor in the dome of the bladder that causes the detrusor muscle to relax and increases bladder capacity. Side effects include an increase in blood pressure, nasal congestion, fatigue, constipation, and tachycardia. It received FDA approval June, 2012. This may offer more treatment options to those that have intolerable side effects or contraindications (closed angle glaucoma) to anticholinergics.
• Antispasmodics: Primarily cause relaxation of detrusor smooth muscle in addition to anticholinergic effects and local anesthetic effects.
• Tricyclic antidepressants: Unique in the ability to increase urethral outlet resistance due to adrenergic stimulation on the smooth muscle of the bladder neck and proximal urethra in addition to anticholinergic effects, direct detrusor relaxation, and a sedative action that may be related to antihistaminic properties (eg, imipramine hydrochloride and amitriptyline hydrochloride). Due to multiple effects of TCA they may be useful in treating mixed urinary incontinence.
• Calcium channel blockers: Uncommon as first-line agents, calcium channel blockers inhibit the inflow of calcium after membrane depolarization and have the potential of relaxing the smooth muscle of the bladder (eg, nifedipine).
![]() What are the treatment options in patients with refractory urge incontinence?
What are the treatment options in patients with refractory urge incontinence?
• Botox injection: Inhibits acetylcholine release from presynaptic cholinergic nerve terminals to suppress unstable contractions (only FDA approved for refractory neurogenic OAB). This occurs by interfering with the docking of vesicles at presynaptic nerve ending by targeting of SNARE protein formation through cleaving of SNAP-25.
• Sacral neuromodulation: Uses electrical stimulation of the sacral nerve root of S3, which results in afferent inhibition of sensory processing in the spinal cord. Studies suggest that it has a conditioning effect on neural excitability and can restore neural equilibrium between facilitatory and inhibitory influences. Although, the exact mechanism of action in each of these conditions may be different.
• Percutaneous tibial nerve stimulation: Electrical stimulation of the posterior tibial nerve transmits the electrical pulse to sacral plexus which modulates afferent sensation and may have a conditioning effect on the bladder. This exact mechanism is uncertain, but is believed to function similarly to sacral neuromodulation. This involves intermittent weekly treatments for 3 months and then monthly thereafter. There are other alternative treatment schedules and these must be continued to have benefits.
• Bladder augmentation: Allows for increased total bladder capacity and physical interruption of the overactive detrusor muscle. It is used as a last resort after exhausting all possible pharmacologic interventions for urge incontinence.
![]() Surgical implanted sacral neuromodulation devices or sacral nerve stimulation is targeted at which sacral nerve and how successful is it?
Surgical implanted sacral neuromodulation devices or sacral nerve stimulation is targeted at which sacral nerve and how successful is it?
Optimally, the S3 sacral nerve root. Only one side is typically treated. Stimulation of S3 results in bellows and plantar flexion of the great toe. Approximately 75% of otherwise intractable cases of urge incontinence report significant improvement with this therapy. Approximately 50% are completely dry.
![]() Is sacral nerve stimulation useful in urinary retention? Can it be used in men?
Is sacral nerve stimulation useful in urinary retention? Can it be used in men?
Yes to both.
![]() Tricyclic antidepressants like imipramine are reasonably effective in what proportion of patients with incontinence?
Tricyclic antidepressants like imipramine are reasonably effective in what proportion of patients with incontinence?
Improvement is reported in approximately 60% and may be especially useful for those with mixed urinary incontinence by increasing the outlet at the bladder neck and relaxing the detrusor, as explained previously.
Intravesical capsaicin desensitizes unmyelinated (c-fibers) afferent nerves. It is most useful in patients who demonstrate bladder hypersensitivity on an ice water test. Improvement of 40% to 100% has been reported.
![]() Describe the nerve control of bladder function.
Describe the nerve control of bladder function.
It is much more effective than oral forms. Plasma and tissue levels are higher and side effects are low as hepatic metabolism is avoided.
![]() How effective is intravesical oxybutynin?
How effective is intravesical oxybutynin?
It is much more effective than oral forms. Plasma and tissue levels are higher and side effects are low as hepatic metabolism is avoided.
Sympathetic stimulation causes bladder relaxation and tightens the sphincter (think storage). Innervation comes mostly from the hypogastric nerve: T11-L2.
Parasympathetic stimulation causes bladder contractions and relaxation of the internal sphincter (think voiding). Innervation comes through the pelvic nerve from the S2-4 sacral plexus. Overactive bladder anticholinergic medications typically work here.
Somatic (voluntary) control of the external sphincter and pelvic floor muscles is provided by the pudendal nerve which also comes from the S2-4 sacral plexus. When stimulated, it tightens the sphincter.
![]() What is the current role for needle suspension for stress urinary incontinence?
What is the current role for needle suspension for stress urinary incontinence?
Needle suspension prevents urethral descent with stress. It has been effective in the treatment of urethral hypermobility but does not affect incontinence due to ISD.
![]() What is the role for urethral bulking agents for stress urinary incontinence?
What is the role for urethral bulking agents for stress urinary incontinence?
Various materials have been injected in the urethra either through the periurethral or transurethral methods as a bulking agent to treat urinary incontinence. The ideal injectable agent should be biocompatible, nonantigenic, noncarcinogenic, and nonmigratory. It is effective in the treatment of intrinsic sphincter deficiency, but does not affect incontinence due to urethral hypermobility.
![]() What is the role for suburethral sling surgery for stress urinary incontinence?
What is the role for suburethral sling surgery for stress urinary incontinence?
Suburethral (pubovaginal) sling procedures effectively prevent urethral descent with stress and improve the urethral washer effect. Therefore, slings are equally effective for urethral hypermobility and ISD. However, there are increased postoperative risks of retention with detrusor overactivity.
![]() An elderly woman presents with urinary urgency and frequency. Ultrasound evaluation determines her postvoid residual to be 350 mL. What is the diagnosis?
An elderly woman presents with urinary urgency and frequency. Ultrasound evaluation determines her postvoid residual to be 350 mL. What is the diagnosis?
This patient has detrusor overactivity with impaired contractility, which generally presents commonly in the elderly patients. Treatment is difficult since pharmacologic treatment of the detrusor overactivity often exacerbates the retention. This optimally requires clean intermittent catheterization that is often difficult in the elderly population. It is important to rule out large cystocele or other co-existing anatomic abnormalities, which can “kink” the urethra and cause increased bladder outlet resistance.
![]() A 46-year-old woman, gravida 4, para 4, presents with urgency, frequency, and urinary incontinence. Physical examination is normal, Marshall test is negative, and urodynamic evaluation reveals a normally compliant bladder without involuntary bladder contractions. What is the diagnosis?
A 46-year-old woman, gravida 4, para 4, presents with urgency, frequency, and urinary incontinence. Physical examination is normal, Marshall test is negative, and urodynamic evaluation reveals a normally compliant bladder without involuntary bladder contractions. What is the diagnosis?
This patient has classic urge incontinence. It is important to focus on the chief presenting symptom in evaluating a patient with urinary incontinence. Despite the obstetrical history and the lack of involuntary bladder contractions, the diagnosis remains urge incontinence. The absence of detrusor overactivity on a single urodynamic study does not exclude its diagnosis.
![]() A woman presents with complaints of urgency and precipitous voiding shortly following a cough or sneeze. What is the diagnosis?
A woman presents with complaints of urgency and precipitous voiding shortly following a cough or sneeze. What is the diagnosis?
This patient has stress-induced urge incontinence. Stress incontinence is the involuntary loss of urine during coughing, sneezing, or increases in intra-abdominal pressure. The described patient loses urine after the intraabdominal pressure has returned to normal and continues to empty her bladder precipitously. This suggests an involuntary bladder contraction occurring due to the stress stimulus.
![]() A woman presents with urodynamically demonstrated stress incontinence with urinary urgency. What is the treatment of choice?
A woman presents with urodynamically demonstrated stress incontinence with urinary urgency. What is the treatment of choice?
First treat the stress incontinence. Urgency may result from compensatory responses initiated by the incontinent patient. Alternatively, urgency may be a product of urine passage into the proximal urethra with stress leakage. In 65% of patients with mixed stress and urge incontinence, correction of the stress incontinence will resolve the urgency. However, if the urgency component is successfully treated medically, many patients are satisfied without the surgery.
![]() A woman presents with urinary incontinence immediately following a repair of a large cystocele. What is the diagnosis?
A woman presents with urinary incontinence immediately following a repair of a large cystocele. What is the diagnosis?
Occult stress urinary incontinence. The full bladder contributes to normal continence by creating a valvular effect through limited posterior rotation of the bladder base against a well-supported urethra during stress. Cystoceles exacerbate this valvular effect and may mask underlying urethral dysfunction. Correction of a large cystocele in this setting leads to incontinence due to either urethral hypermobility or ISD.
![]() A woman with stage 2 symptomatic POP without incontinence is scheduled to have vaginal prolapse repair. Should she undergo a concomitant midurethral sling?
A woman with stage 2 symptomatic POP without incontinence is scheduled to have vaginal prolapse repair. Should she undergo a concomitant midurethral sling?
Yes. Placement of a midurethral sling will reduce her odds of developing occult stress incontinence based on one randomized control trial (OPUS). Potential for increased complications from placement of the sling include UTI, major bleeding, bladder perforation, and incomplete bladder emptying which should be discussed in preoperative counseling. The number needed to treat (NNT) is 6 to prevent 1 episode of occult SUI.
![]() What are the differences between the retropubic (TVT) and transobturator (TOT) midurethral slings?
What are the differences between the retropubic (TVT) and transobturator (TOT) midurethral slings?
In the majority of the trials, both treatments had equivalent outcomes for SUI. The complications differed with TOT having more chronic thigh and groin pain and the TVT has more bladder perforation and voiding dysfunction. In patients with ISD, TVT may improve outcomes.
![]() A woman complains of incomplete emptying and straining to void 4 weeks after a retropubic (TVT) is performed. What is her diagnosis during the voiding UDS and what should be her treatment?
A woman complains of incomplete emptying and straining to void 4 weeks after a retropubic (TVT) is performed. What is her diagnosis during the voiding UDS and what should be her treatment?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


