Normal Continence
Continence is a balance between the ability of the anal sphincter mechanism to withstand the propulsive efforts of the distal intestine, which depends on motility patterns and adequate rectal capacitance. The anal sphincter and pelvic floor form a complex mechanism with motor and sensory nerve components.
Take your hands if you will and cup them. Put in them a mixture of gas, liquid and solid, And try to let only the gas escape—your will fail! The anal sphincter mechanism can do this. Furthermore, the sphincter mechanism can tell Whether you are with friends or alone, Whether you are sitting or standing, or whether you have your pants on or off. There is no muscle that is so prepared to preserve the dignity of mankind Yet so ready to come to one’s relief.
—ROBERT W. BEART, JR, MD
The anal sphincter mechanism includes the anal sphincter itself and the levator ani (see
Chapter 1). The latter forms the pelvic floor. It is composed of three parts, including the ischiococcygeus, the pubococcygeus, and the puborectalis (see
Figures 1-11 and
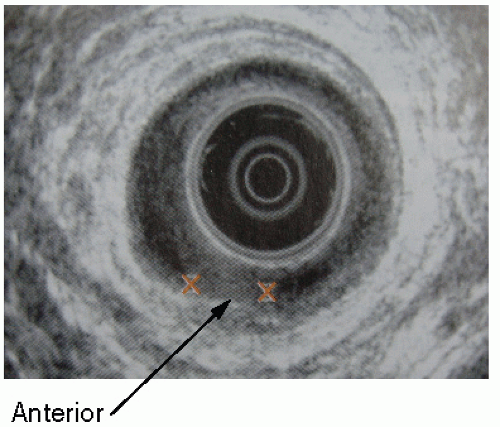
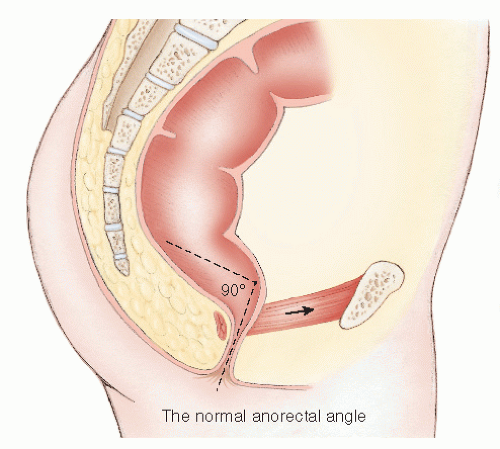
1-12). The first two form a muscular sheet across the pelvic outlet with attachments to the back of the pubis, the obturator fascia, and the coccyx. This is penetrated in the midline by the urethra, vagina, and gut tube in female and by the urethra and gut tube in male. The puborectalis arises on each side from the back of the pubis and passes posteriorly to form a sling around the gut tube. This and the levator ani are in a constant state of tonic activity mediated by muscle spindles located in the levator ani. As a result, the puborectalis draws the gut tube forward to create an angle between the rectum and anal canal. Under normal resting conditions, the long axes of each form an angle, the anorectal angle, which is about 90 to 100 degrees. The puborectalis sling marks the functional junction between the anal canal and the rectum and is easily palpable on digital examination (
Figure 16-2).
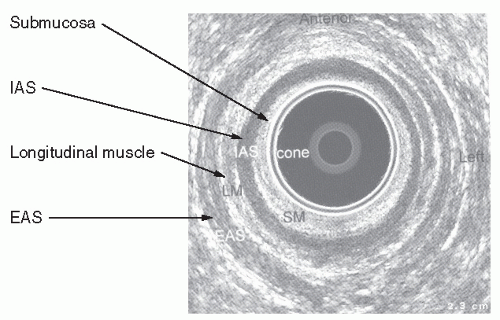
The anal canal comprises the internal and external sphincters and its epithelial lining, which is richly supplied by sensory nerves. The internal sphincter is responsible for 70% of the resting tone.
27 It is maximally contracted at rest and shows reflex relaxation in response to distension of the rectum. This is referred to as the rectoanal inhibitory reflex (RAIR), which is under autonomic control and requires an intact submucous nervous plexus for it to function.
267 The pelvic floor musculature relaxes during defecation. Sensory factors include the sampling reflex that is disordered in incontinence.
178 It has been estimated that about 15% of anal resting tone is due to the hemorrhoidal complexes.
261 The longitudinal length of the anal sphincter complex in female is less than that of male.
493
Causes of Incontinence
A classification of the causes of incontinence is shown in
Table 16-2.
Increased Intestinal Propulsion
Fecal incontinence can be due to uncontrollable defecation as a result of inflammatory or functional disease of the rectum and more proximal bowel. Diarrheal disorders associated with urgency include any form of proctitis, but in clinical practice ulcerative colitis or Crohn’s disease are the most important. Infective proctocolitides, dysentery, is usually self-limiting or responds to treatment, but it is necessary to consider this in the differential diagnosis of incontinence, particularly because the incidence of infective proctocolitis is increasing in Western society, especially in institutions (see
Chapter 33). Organisms responsible include among others
Shigella, Clostridium difficile, and
Campylobacter. C. difficile and ulcerative colitis can present in an identical manner. There has been an “alarming” increase in
C. difficile- associated disease (CDAD) in the United States. This has been dramatic in patients with inflammatory bowel disease (IBD). Rodemann and colleagues reported that between 1998 and 2004 in the United States, CDAD in ulcerative colitis patients rose from 18.4 to 57.6 (more than threefold) per 1,000 admissions.
379 In endemic areas,
Entamoeba histolytica should be borne in mind.
Urgency may be the predominant feature in some patients with irritable bowel syndrome. It is important to recognize this because surgery has no role to play in the treatment, although neuromodulation may have a place.
Urgency incontinence may also occur as a result of inadequate capacitance of the rectum or “neorectum” in patients who have undergone restorative surgery or radiotherapy. In colorectal practice where many patients will have had a low anterior resection, for example, this form of incontinence is fairly common. Functional symptoms after anterior resection are referred to as the anterior resection syndrome and include the frequent passage of small-volume stool with passive and sometimes urgency incontinence. Those with this disorder may also have a weak sphincter (see next section).
Intrinsic Sphincter Incompetence
The anal sphincter mechanism may be unable to retain stool and flatus if it suffers damage to its nerve supply or as a consequence of direct trauma. Myopathic degeneration can also occur. There is a gradual physiologic weakening with age that can be identified by physiologic testing.
205
Age
Attempts have been made to compare functional estimations of anal sphincter capacity in the elderly population with younger individuals. Bannister and coworkers measured anorectal function in 37 elderly patients and compared the results with 48 young, physiologically normal subjects.
18 The former had lower anal pressures, required lower rectal volumes to inhibit anal sphincter tone, and had increased rectal pressures as measured by balloon distension, implying lower compliance. Some suggest that internal anal sphincter dysfunction may be the important factor.
21 Others believe that, especially in women, the pudendal and somatic pelvic nerves are injured when there is perineal descent on straining such as occurs with aging or during childbirth.
244 Many geriatricians believe that fecal incontinence is more likely to be due to a remediable cause, such as fecal
impaction, rather than to dementia, the postmenopausal state, or to old age.
283
Neurologic Disease
Any neurologic disease may affect bowel control. Upper and lower motor neuron lesions seen in general neurologic diseases, injury to the spinal cord or cauda equina, spina bifida, and neuropathies can all be responsible. In diabetes mellitus,
484 there may be the dual factors of diarrhea from autonomic neuropathy and diffuse sphincter weakness due to the neuropathy.
General neurologic diseases including multiple sclerosis
206 and Parkinson’s disease can be associated with incontinence. It is clearly necessary to be aware of the possibility of these when assessing the patient. Dementia due to cerebral degeneration in the elderly has already been mentioned. It and presenile dementia are among the most common causes of incontinence. Other conditions leading to cerebral damage include cardiovascular accident, trauma, and tumor.
Spinal cord injury results in weakness of the pelvic floor muscles, but it can also lead to failure of rectal evacuation, impaction, and soiling. Reflex defecation precipitated by sensory cutaneous stimulation above the level of the lesion may be maintained.
Trauma to the cauda equina, with damage to sacral 4 and 5 segments, causes lower motor paralysis of the pelvic floor and sphincter muscles. Voluntary contraction of the levator ani and external sphincter is reduced or absent depending on the severity of the lesion. Internal sphincter tone is preserved, however, because this is mediated by autonomic activity. There is sensory loss of the perineal skin and of the anorectum and patulousness after digital examination (
Figure 16-3).
Spina bifida occurs in association with meningocele or myelomeningocele. Involvement of sensory or motor nerves may produce urinary and fecal incontinence and, with time, rectal prolapse, which will further exacerbate the incontinence. This condition is described in
Chapter 21.
Rectal impaction causes internal sphincter relaxation through activation of the RAIR, owing to distension of the rectum by stool. This is a temporary effect that will resolve once the impaction is treated. Schiller and colleagues, in their study of 16 diabetic patients, concluded that incontinence was due to internal anal sphincter dysfunction and that those without diarrhea have no impairment of fecal control.
400
Idiopathic Incontinence (Pudendal Neuropathy)
Idiopathic incontinence is the term used to describe denervation injury to the sphincter muscle that occurs for no apparent cause. Habitual straining during defecation, nerve entrapment, the preprolapse state, and the descending perineum syndrome have all been implicated. It may be seen after traumatic obstetrical delivery.
The condition was first formally defined by Parks and colleagues
352 in a group of patients with incontinence or rectal prolapse associated with diffuse weakness of the anal sphincter muscles. Biopsies taken from the external sphincter showed histologic evidence of atrophy of type I fibers. These patients also had neurophysiologic evidence of denervation as determined by single-fiber electromyographic (EMG) studies. This technique enables an estimate of the ratio of nerve to muscle fibers in the motor neuron unit. When denervation occurs, there is reinnervation by branching of intact nerve axons in an attempt to reach denervated muscle fibers. Consequently, the ratio of nerve to muscle fibers increases, and this can be detected neurophysiologically by direct recording of a needle electrode introduced through the skin into a nerve ending.
320 In addition, measurement of the speed of conduction in the pudendal nerve showed the latency to be increased.
227 Further studies in patients with idiopathic incontinence identified that most also have degenerative changes in the internal sphincter.
245,266 It was postulated that the neuropathic changes might be due to damage to the pudendal nerve through stretching, thereby causing a degree of apraxia as might occur with excessive descent of the pelvic floor, such as in the descending perineum syndrome or during childbirth. It is unlikely that stretching occurs at the level of the ischial spine because at this level the pudendal nerve has not yet branched to supply the sphincter, perineum, and clitoris. Computer modeling has hypothesized that potential stretch during delivery is more likely to damage the inferior rectal nerve.
263Objective evidence of a sensory deficit can be found in patients with idiopathic neuropathic incontinence, as would be expected in the presence of nerve damage. Others have supported the hypothesis that sensory function may be an independent factor contributing to continence.
22,31The normal anal canal is extremely sensitive to temperature. Moreover, there appears to be a temperature gradient between the rectum and the anal canal.
308,309 Ambulatory pressure monitoring has shown that the sphincter relaxes several times an hour, allowing equalization of rectal and anal pressures, which permits entry of small amounts of rectal contents into the anal canal.
307 This so-called sampling reflex may be lost with neuropathic change. Patients with idiopathic incontinence have reduced thermal sensation at all levels within the anal canal when compared with normal individuals.
306 Another report from the same unit involving patients with hemorrhoids and others with incontinence showed reduced sensation in incontinence but also in those with hemorrhoids, albeit to a lesser degree.
308 Others have challenged the importance of thermal sensitivity on the basis that the maximum temperature difference was merely 0.13° and was in the region of the anorectal junction.
381 Such a
difference was considered too small in their view to have a meaningful role in sampling.
Myopathic Disease
Physiologic
Estrogen and progesterone receptors have been found in the internal sphincter, derived from tissue obtained from hemorrhoidectomy specimens in premenopausal and postmenopausal women. Although none of the differences was considered to be statistically significant, the numbers (17 in each group) were small—a type II error. In premenopausal patients, estrogen receptors were present in 23.5% compared with 11.8% in postmenopausal women. The respective proportions of progesterone receptors were 41.2% and 11.8%.
348
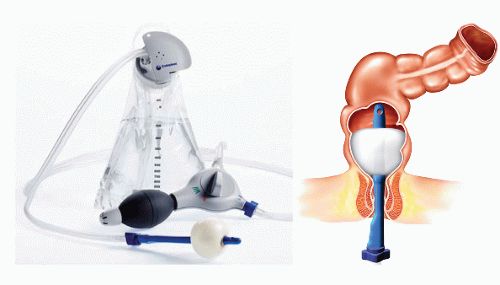
Internal Sphincter Degeneration
Internal sphincter degeneration was described by Vaizey and colleagues in 1997.
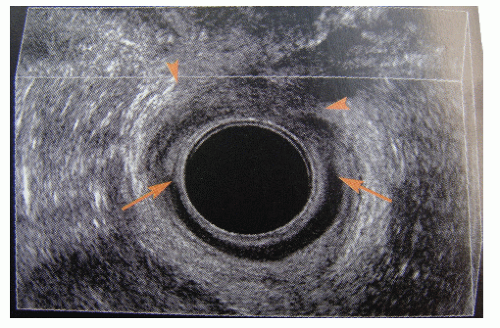
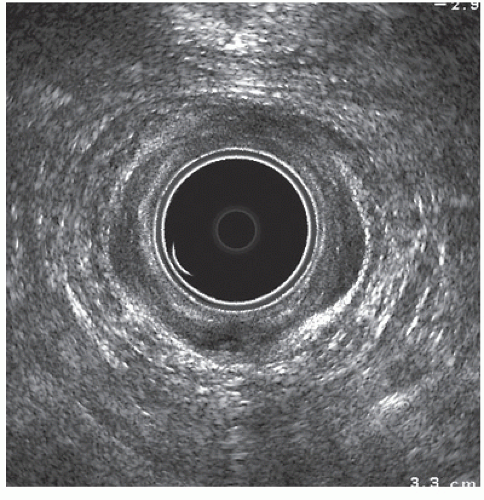
466 They reported a series of 45 patients (35 females) who presented with passive incontinence associated with reduced resting anal and normal squeeze pressures. The pudendal nerve terminal motor latencies (PNTMLs) were normal. The internal sphincter on ultrasound was thinned and showed hypoechoic changes (
Figure 16-4). The increased thickening seen with normal aging is not seen. Such patients may be suitable for neuromodulation (see later).
Scleroderma
Scleroderma is a chronic multisystem disorder characterized by excess deposition of connective tissue in skin and internal organs, associated with microvascular changes and immunologic abnormalities leading to nerve and muscle degeneration. This results in motility disturbances of the gastrointestinal tract. Thus, gastric emptying is delayed in up to 75% of patients, with small bowel involvement occurring in 17% to 57% of patients. The migrating motor complexes are reduced or absent, predisposing to bacterial overgrowth. Barium enema examination demonstrates pancolonic involvement in 10% to 50% of patients associated with wide-mouthed diverticula. Pseudoobstruction may occur. Complications include pneumatosis cystoides intestinalis, stercoral ulceration, and perforation.
Systemic sclerosis may produce incontinence on either a neurologic or a myopathic basis.
66,257 The condition affects the internal sphincter, which shows morphologic changes compatible with both neuropathy and myopathy, with atrophy and fibrosis. Resting tone is reduced, and the RAIR may be absent.
114Anal manometry may demonstrate a reduction or loss of the RAIR. Treatment includes biofeedback, sacral nerve stimulation, and surgery.
114,232
Anorectal Disease
Soiling may occur in anorectal disease from such conditions as hemorrhoids, fissure, and anal fistula, even without surgical intervention. Prolapse of rectal mucosa or hemorrhoids and true procidentia may interfere with closure of the anal canal. With time, the protruding mass stretches the sphincter and may lead to further weakening. In addition, the rectal prolapse is likely to be associated with internal sphincter atrophy and pudendal neuropathy, both of which are factors responsible for its occurrence in the first place. The incontinence is often ameliorated with definitive treatment of the prolapse (see
Chapter 21).
395
Failure of embryologic development of the hindgut, pelvic floor, and related structures results in varying degrees of anatomical and functional deformity. The condition occurs in approximately 1 in 5,000 births. There are several classifications that mostly divide patients into those with a low, intermediate, or high anomaly. A high anomaly is often associated with a degree of sacral agenesis and in addition to anatomical loss of the lower gut tube; there is also sensory and functional loss of that part of the rectum that is present. The anal sphincter mechanism is not developed and may be too weak to maintain continence even after surgical procedures, such as pull-through operations and posterior sagittal anorectoplasty (PSARP). A megarectum may be present.
The adult colorectal surgeon may encounter patients with a congenital anomaly after leaving pediatric care. Many will have undergone surgery in infancy, either in the form of a pull-through procedure or a PSARP.
62,355,356Those with a low anomaly may have been satisfactorily managed by surgical recanalization when the lumen is absent by dilatation of the stenosed anal segment. The functional results may be disappointing. The condition is described in greater detail in
Chapter 3.
Extrarectal Fistula
In this condition, there is an abnormal communication between the intestine above the level of the anal sphincter and the outside, usually the perianal skin. Etiologies and associated conditions include neoplasms, inflammatory conditions (Crohn’s disease, diverticular disease), and anastomotic leakage. A fistula from an intra-abdominal organ to the perineum or vagina will result in fecal incontinence. A pouch-vaginal fistula is one of the most common conditions encountered in colorectal surgical practice.
185,412 Management is directed to the cause of the fistulization. This can be located in the intestine, the female genital tract, or to the urologic system.
Figure 16-5 demonstrates a fistula to
the perineum from a segment of diverticular disease of the sigmoid colon. The diagnosis and management of extrarectal fistula will be dealt with in
Chapter 14.
Trauma
The anal sphincter mechanism can be damaged by direct injury in the form of surgery, itself, or by civilian or military trauma. It can also be damaged during childbirth. In the practice of colon and rectal surgery, childbirth injury is now the most common cause of traumatic incontinence.
Obstetrical Injury
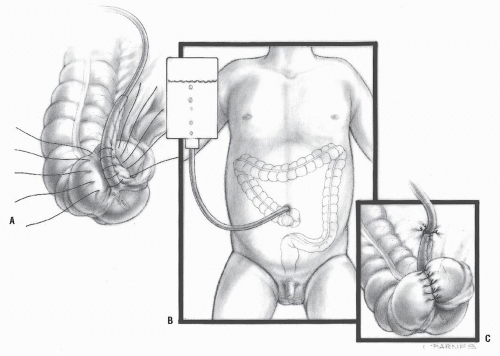
Direct Sphincter Trauma and Nerve Damage
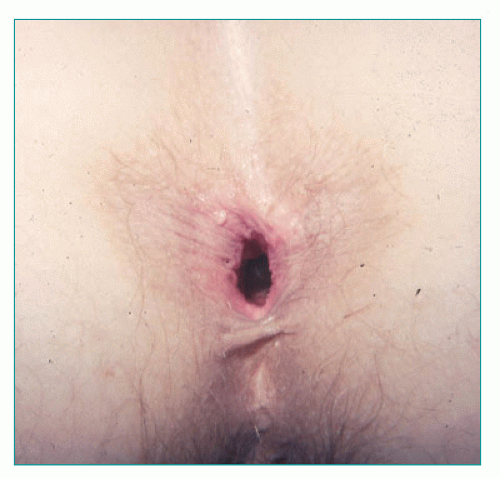
During delivery, the pelvic floor is at risk from trauma due to stretching by the fetal head on the perineum. This may cause a tear in the anterior part of the sphincter. Such an injury may involve only the sphincter ring or it may result in a cloacal deformity if a complete rupture of the anal canal opens into the introitus (
Figure 16-6). In recent years, more emphasis has been placed on this form of damage than on denervation injury. Both are, however, important and often occur simultaneously. Subclinical nerve damage during delivery may be a cause of incontinence years later as the natural process of neuromuscular degeneration leads to a situation where the sphincter is no longer competent. This may account for somewhat disappointing results following surgical repair.
Evidence of pudendal nerve damage from childbirth was first reported by Snooks and colleagues in 1984 who measured fiber density and PNTMLs in 79 women 2 months following delivery. Compared with controls, fiber density (1.37 vs. 1.67) and PNTML (1.9 vs. 2.1) were both abnormal in multiparous women, with recovery being evident in those who were primiparous.
418,419 Rieger and colleagues
375 found a fall in resting and squeeze pressures at 6 weeks after delivery among 53 primiparous women. Although a sphincter defect was found in 41%, this was not associated with lowered anal canal pressures. In a series of 259 women assessed at 6 weeks prior to and 8 weeks following delivery, a sphincter defect occurred in 16.7% and only in those undergoing a vaginal delivery. Multivariate analysis showed forceps delivery (OR = 12), perineal tear (OR = 16), episiotomy (OR = 6.6), and parity (OR = 8.8) to be risk factors for incontinence. Overall, 9% had symptoms of incontinence, but of these only 45% were found to have a defect.
It has become clear that incontinence after childbirth can occur without a sphincter defect.
6 When pudendal nerve function was measured in 128 unselected women before and at 6 to 8 weeks after delivery, there was a significant increase in PNTML determinations in both primipara and multiparous women but not in 7 patients who underwent elective cesarean delivery, although not in those having a section after a trial of labor. Twelve women with increased PNTML at 6 weeks were reexamined at 6 months; 8 had returned to normal values.
435 In incontinent patients, the PNTML was increased and related to perineal descent, indicating the presence of neurologic damage to the whole pelvic floor in some patients.
245 Persistent evidence of pudendal neuropathy was evident among 14 multiparous women who were followed for 5 years.
422 Physiologic studies on postpartum women have shown that multiparity, forceps delivery, increased duration of the second stage of labor, and high birth weight may lead to pudendal nerve damage and to sphincter atrophy.
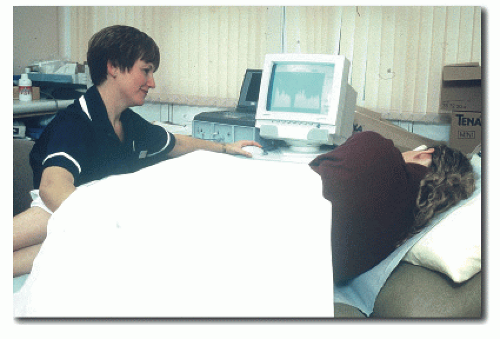
421Anal ultrasound has demonstrated a high incidence of subclinical sphincter damage following delivery (
Figure 16-7). In many cases, the presence of a defect on ultrasound has been interpreted as an indication for surgical repair. Many of these instances, however, are not associated with disruption of the sphincter ring, and repair offers, therefore, no benefit in this circumstance. Poor case selection may be another factor to explain some of the unsatisfactory results following repair.
Incidence
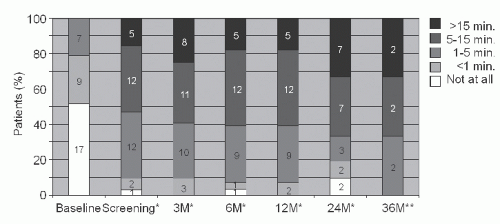
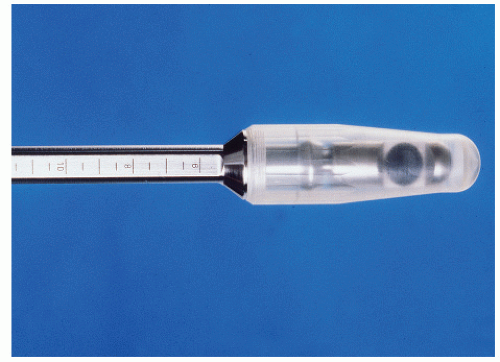
The use of ultrasound (
Figure 16-8) has enabled the incidence of sphincter injury during childbirth to be studied objectively. In a group of 202 women who had an anal ultrasound prior to delivery, a repeat examination was undertaken in 150 at 6 weeks and in 32 at 6 months after delivery. Symptoms of anal incontinence were present in 10/79 (13%)
of primiparous individuals and in 11/48 (23%) of those who were multiparous. A sphincter defect was found in 28/79 (35%) and 19/48 (40%) at 6 weeks and in 22/79 (28%) of primiparae at 6 months. None of the 23 patients who had a cesarean delivery were found to have a defect. Eight of 10 patients who had forceps assistance developed a defect compared with none who had vacuum extraction. There was a correlation between a sphincter defect and symptoms of incontinence, including urgency as well as soiling.
436A similar finding was reported by Pollack and colleagues from a questionnaire survey of 349 nulliparous women who then became pregnant.
366 Of these, 242 returned the questionnaire at 5 and 9 months and 5 years after delivery. At 5 years, incontinent symptoms were reported in 53% of women who had a sphincter tear and in 32% of those who did not. Age, sphincter tear, and subsequent childbirth were all risk factors for incontinent symptoms at 5 years. It is important to point out that in most of these patients “incontinence” was no more than occasional loss of flatus and that fecal incontinence was rare. de Leeuw and colleagues found that 12 (35%) of their 34 patients who suffered a sphincter injury at the time of delivery experienced difficulty with bowel control.
98 Sphincter defects were demonstrated in the majority. The protective effect of cesarean delivery was demonstrated in a study of 1,200 women, half of whom underwent assessment after delivery.
503 In those who had a vaginal delivery, there was a fall in anal canal resting pressure, although this did not occur after cesarean delivery. The first vaginal delivery appeared to cause a permanent lowering of resting anal pressure. Frudinger and colleagues found that anal continence deteriorated in 27.6% of women following delivery, 43.2% of whom had sonographic evidence of sphincter trauma.
144 Others have shown a high prevalence of anal sphincter defects on ultrasound (up to 62%) in incontinent, parous women without a prior history of anal surgery.
91,318In a study of 3,002 primiparous women who delivered between 1983 and 1986 recorded on the U.K. National Health Service database, 62% responded to a questionnaire sent two decades later. Of the 985 with adequate data, 54% recorded some form of pelvic floor symptom. About 5% had severe impairment of continence to solid stool. Cesarean delivery was protective for both urinary (OR = 0.47) and fecal (OR = 0.32) incontinence, but of 76 who had only a cesarean delivery, 9 (12%) had experienced some degree of fecal continence disturbance.
107In most patients, fecal incontinence when present resolves spontaneously within the first year. Thus, in a series of 86 primiparous women having vaginal delivery, 19 (25%) had flatus incontinence at 5 months, but this had fallen threefold by 12 months.
319 In some patients symptoms persist, with the rate estimated to be approximately 3%.
111 Macarthur and colleagues followed 4,214 women by mail questionnaire for 6 years.
270 The prevalence of fecal incontinence at 6 years was 3.6%. Interestingly, only 10% of patients had any symptom after the first delivery. Cesarean delivery was not related to the development of symptoms (OR = 1.04), but forcepsassisted delivery at any time was (OR = 1.48). Other risk factors included high maternal age, multiparity, and Asian ethnicity. There is other evidence indicating that African Americans have a lower incidence of pelvic floor trauma than other racial groups.
14,200 In their study of 128 unselected women, Sultan and associates found that a heavy baby and a prolonged second stage of labor were associated with abnormal pudendal function following delivery.
435Patients who have persisting symptoms of postpartum incontinence, or present with late onset fecal incontinence, have a high prevalence of sphincter injury. Thus, the presence of a sphincter defect among 335 patients with fecal incontinence was 65%, rising to 88% in those who had had a vaginal delivery and proctologic surgery. This compared with 43% of patients without symptoms of incontinence and with 22% in asymptomatic volunteers, the latter suggesting that the criteria for determining a sphincter defect may have been too liberal.
220 Not all reports have indicated obstetrical
injury is associated with incontinence. In another questionnaire survey, Fritel and coworkers received a response from 85% of 3,114 women aged 50 to 61 years.
141 Fecal incontinence within the prior 12 months was experienced by 250 (9.5%) and was related to depression (OR = 2.1), obesity (OR = 1.5), previous surgery for urinary incontinence (OR = 3.5), and anal surgery (OR = 1.7), but not to any obstetrical variable, such as parity, mode of delivery, birth weight, episiotomy, or third-degree perineal tear.
The symptoms and prognosis of incontinence may be related to the severity of the obstetrical injury. In a series of 52 women having a third- or fourth-degree tear treated by repair, 31 (61%) had persisting symptoms. The prevalence of a defect in each group was 39 (75%) and 10 (20%).
362 A mail survey by questionnaire was carried out in 180 women out of 5,123 who experienced a vaginal delivery in one Norwegian county between 1999 and 2000. Of these, 156 (87%) responded. At a median of 25 months, 88 (59%) experienced incontinence symptoms that were restricted to flatus in 53 (35%). Fourteen (9%) patients had urgency as the only symptom. It is noteworthy that only 3 of 29 women who regarded themselves to be severely disabled had sought medical help.
331 Others, however, have not found a correlation with the severity of the tear and symptoms. In a study of 330 patients with fecal incontinence, Voyvodic and colleagues found no correlation between the ultrasonic severity of external and internal sphincter defects and symptoms.
483 Resting tone was not related to whether or not there was a defect of the internal sphincter, although patients with a fragmented sphincter did have a low resting pressure. In contrast, however, Nichols and colleagues carried out a prospective study of 56 women who sustained a third- or fourth-degree tear of whom 39 were enrolled.
328 Those with a fourth-degree tear were more likely to have bowel symptoms (59% vs. 28%) and a persistent defect (48% vs. 8%).
In another study of 55 women having their first baby, ultrasound evidence of trauma was found in 13 (29%), but clinical significance was confined to the 5 patients with evidence of external sphincter damage.
490
Encopresis
Encopresis, or psychogenic soiling, is defined as the passage of formed or semiformed stool in a child’s underclothes (or other inappropriate places) that occurs regularly after the age of 4 years. It is essentially an involuntary evacuation of the bowel not caused by organic factors. Encopresis is at least four times more common in boys than in girls and is analogous to enuresis as it pertains to urinary incontinence.
The condition was first described by Weissenberg who recognized that this form of fecal incontinence was associated with emotional disturbance. Behavioral factors that may contribute to the problem include the following:
Excessive parental attention to toilet habits
Laxative use
Harsh or lax toilet training methods
Fear of the toilet or the loss of feces
Desire for attention
Family or personal stress
In time, the increasing retention of feces leads to attenuation of the rectal wall, lax sphincter contractility, progressive constipation, obstipation, and fecal impaction. Anal fissure and hemorrhoidal difficulties may develop. Loening-Baucke observed a common clinical history with children exhibiting chronic constipation and soiling, often many years of infrequent and abnormal stools, a dilated rectal ampulla, and the presence of an abdominal fecal mass.
Treatment is usually directed toward bowel management, stress reduction, and child and family psychological counseling. Laxatives, enemas, and dietary regimens are recommended, as well as encouraging the child to sit on the toilet for 10 minutes twice daily at the same time each day. The goal is to establish a practical time for defecation and, ultimately, a spontaneous bowel evacuation habit. Uridine-5-triphosphate has been suggested to have some limited success. Although the mechanism of action of this drug has not been ascertained, it is believed to stimulate the cortical substance of the brain to make the child more aware of the need to defecate.
Loening-Baucke used anorectal manometry to evaluate 20 healthy children, 12 with constipation, and 20 with chronic constipation and encopresis. Mean values for anal resting tone and anal pull-through pressure were lower in the constipated and the encopretic children than in the controls. The study was repeated up to 4 years after treatment for the condition; abnormal anorectal function was still apparent even years after cessation of treatment and apparent recovery. In a later study of 97 children, also by Loening-Baucke, the author reported that 57% had not recovered. Using a host of training techniques, Loening-Baucke noted that there was no difference in recovery rates for boys and girls, and that the likelihood of success or failure could not be predicted a priori.
Anal Surgery
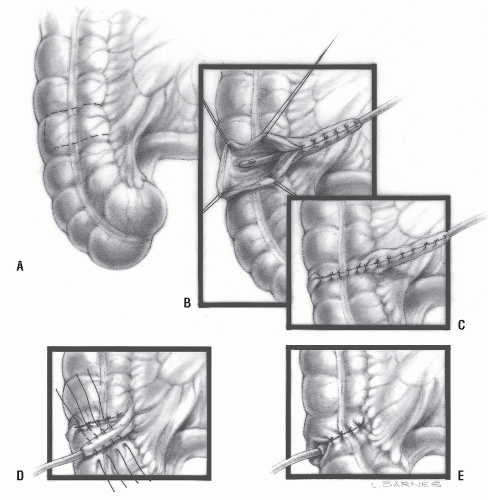
Fistula-in-Ano.
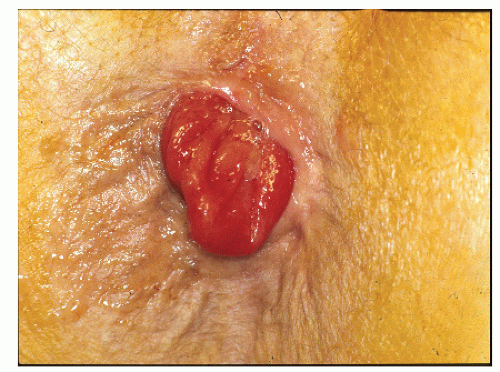
The adverse effect of fistula surgery on continence has been recognized for many years (
Figure 16-9).
34,36 Varying degrees of impairment for control are seen even after what is considered to be a limited division of the sphincter muscle. Complete incontinence (for formed stool) that follows anorectal surgery is usually the result of inappropriate division of the anorectal ring. This is most likely to occur when a high fistula is laid open or an artificial internal opening is created (see
Chapter 14).
Internal Anal Sphincterotomy.
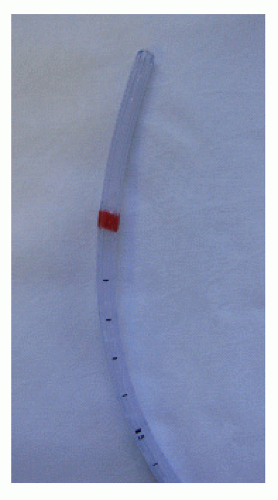
Internal anal sphincterotomy (
Figure 16-10) has been the preferred surgical treatment for anal fissure for many years (see
Chapter 12). It is still the most effective approach to the management of this condition when conservative treatment fails. Unfortunately, there is a small incidence of incontinence associated with this operation. The literature, however, confuses minor with major incontinence, and in many of the reports, preoperative continence has not been recorded. The results of medical and surgical treatment have been summarized by Nelson in two excellent Cochrane reviews,
321,322 with a commentary in an editorial by this author.
326 The incidence is probably well below 5% and the type of soiling is minor, with mostly small amounts of mucous discharge or flatus. It may be that a form of “tailored” sphincterotomy will avoid this possibility.
119,190 There is a more detailed discussion of this topic in
Chapter 12.
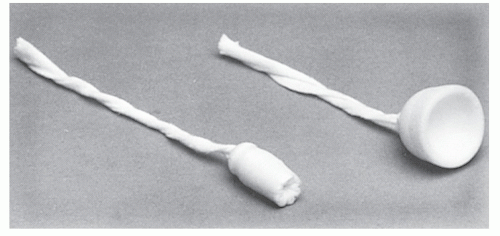
Anal Dilatation.
Sphincter stretch for anal fissure or manual dilatation as a treatment for hemorrhoids (Lord’s procedure) is also associated with fecal incontinence. This was first reported by Snooks and colleagues before anal ultrasound was available.
417 In a series of 10 patients who had undergone a Lord’s anal dilatation, they demonstrated impairment of both the external and internal sphincters. Subsequent reports of the ultrasonographic changes showed disintegration of both sphincters.
330,424 Damage caused in this manner results in a
destruction of the normal sphincter anatomy and is untreatable by conventional repair (
Figure 16-11). For this and other reasons, hemorrhoids are no longer treated by manual dilatation.
Other Anal Operations.
Partial incontinence may follow hemorrhoidectomy. This may further impair closure of the canal and allow continuous discharge of mucus (see
Chapter 11).
168
Accidental Trauma
Trauma to the perineum can injure the sphincter mechanism (
Figure 16-12). Impalement on a spike or pole as well as social injuries (e.g., fist fornication) may result in rupture of the sphincter and contamination of the extrarectal spaces.
53,89,265,343,494 Sepsis can supervene and lead to excessive scar formation with a resultant patulous anal canal and an incompetent sphincter (see also
Chapters 17 and
18).
Reduced Rectal Capacity
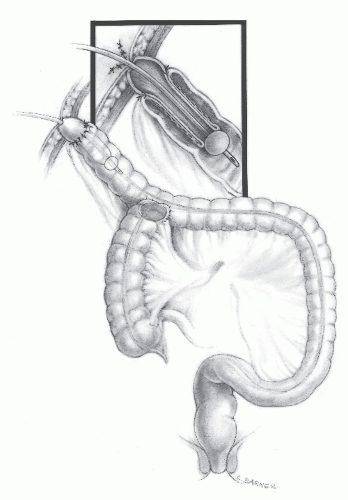
Anterior Resection
In low anterior resection, there are several factors that can impair continence. These include the loss of the rectal reservoir, damage to the anal sphincter mechanism, reduced sensation, and the effect of radiotherapy. This last factor may cause direct radiation damage to the sphincter if this is in the field of irradiation. If radiation is given postoperatively, it will reduce neorectal compliance (see later). Bowel resection designed to preserve the anal sphincter (e.g., low anterior resection, various pull-through procedures, coloanal anastomosis, abdominosacral resection) frequently results in discharge of mucus or incontinence for flatus and stool by the effect of anterior resection on the rectal capacitance, sphincter function, and neural regulation. Injury to the levator ani and external sphincter or to their innervation, and the decreased capacity of the neorectum, are contributing factors.
192,295,327Some degree of sphincter stretch occurs when a low coloanal or ileoanal anastomosis is carried out, either by transanal stapling or manually.
197 Even after a stapled ileoanal anastomosis, resting tone falls in 50% of patients.
68 This gradually improves with time (up to 2 years) but never fully recovers. In a prospective, randomized study of transanal-stapled anastomosis compared with the use of biofragmentable ring, 5 of 18 patients in the former group had ultrasound evidence of fragmentation of the internal sphincter that was associated with symptoms.
193Clinically, the patient will suffer from frequent smallvolume evacuations, often without warning and often associated with incontinence usually of the soiling type.
345,497
Pelvic Radiotherapy
Radiotherapy will cause direct injury to the anal sphincter if this is in the field of irradiation as is the case of patients having treatment for anal carcinoma.
425,473 Damage to the rectum can also occur following radiotherapy for prostatic carcinoma.
272,365,445 When used for the treatment of rectal cancer, radiotherapy doubles the risk of poor function because
it is superimposed on the anterior resection.
122 This is particularly true when given postoperatively.
269 The long-term effects of adjuvant radiotherapy that was employed in the Swedish trials, especially those involving five 25 Gy fractions, have been reviewed by Birgisson and colleagues.
33 Surgical options are limited, with every operative approach having a high complication and failure rate (see
Chapter 24). Most patients are, therefore, usually managed conservatively by antidiarrheal agents and a bowel management program or by fecal diversion.
179 Sacroneuromodulation has been used in four patients after anterior resection with chemoradiotherapy, of whom three appeared to benefit from permanent implantation.
372
Activation of the Anorectal Inhibitory Reflex
Patients with fecal impaction often are incontinent owing to the reflex development of internal sphincter relaxation. This results in passive leakage of stool associated with a physiologically patulous sphincter.