The approach to diagnosis and management of allograft dysfunction is best understood by the time period after transplantation. Although many of the causes of allograft dysfunction
may occur at virtually any time point after implantation (such as acute rejection, recurrent glomerular disease, and ureteral obstruction), there is enough difference in the distribution of diseases, and unique conditions occurring only at specific time points (hyperacute rejection, chronic allograft nephropathy), to make this the most informative way to understand the diagnosis and management of allograft dysfunction.
Following implantation of a living donor kidney, in the absence of technical difficulties with the donor nephrectomy or with implantation or hemodynamic compromise in the recipient, immediate allograft function is expected. Urine output should be brisk (>100 mL/hour) and the fall in serum creatinine rapid (>20% each day). For cadaveric kidneys, poor to no function immediately postimplantation is a relatively common event, occurring in 5% to 35% of patients. Most commonly, as will be discussed below, this is due to DGF (a form of ATN), which can be expected to recover without any specific therapy. However, DGF cannot be assumed to be the cause. The differential diagnosis of nonfunction in the immediate posttransplant period is broad— encompassing disastrous events such as hyperacute rejection, arterial or venous thrombosis, or generally reversible causes such as ureteral obstruction and urine extravasation, as well as DGF—and requires immediate diagnosis, and therapy when indicated (
Table 12.1).
Poor allograft function may be manifest as anuria or oliguria with little fall in serum creatinine. A modest diuresis (<1,000 cc/24 hours) with a slow fall in serum creatinine (10%-15%/day) without the need for dialysis-termed slow graft function—is a clinical scenario which should be evaluated with the same concern as oliguria with no fall in serum creatinine, as many of the same problems may manifest as this clinically milder form of posttransplant graft dysfunction (
89). In the absence of a brisk diuresis and a sustained, progressive fall in serum creatinine following implantation, immediate diagnostic efforts should be undertaken to investigate the cause. It is important to remember that patients who have maintained a relatively normal urine volume from their native kidneys just prior to transplantation can be expected to maintain a normal, or even elevated, urine volume following implantation. In this setting, urine volume or even a modest decline in serum creatinine may not reflect allograft function. Thus, the patient’s residual urine volume is an important element of the medical history to be considered when evaluating allograft function in the immediate postimplantation period.
Evaluation
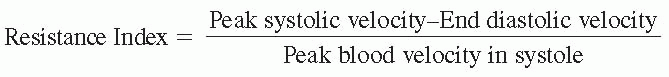
Doppler ultrasound imaging of the transplant is a simple noninvasive test that can easily be done immediately postoperative in the recovery room or intensive care unit, and is the first step in evaluating function immediately after transplantation. Ultrasound can evaluate transplant blood flow characteristics, assess patency of the transplant renal artery and vein, and determine if there is ureteral dilatation, or bladder distension suggesting obstruction to urine flow. In addition, the presence or absence, size, location, and characteristics of any perinephric collections can be determined. Similar although less detailed information may be obtained by radionuclide examination. Further diagnostic and/or therapeutic interventions will depend upon allograft function and the results of initial imaging studies. Analysis of the electrolyte content of wound drainage, if present, or of any perinephric collection may also be of value, particularly in diagnosing urinary extravasation.
Hyperacute Rejection
Hyperacute rejection (HAR) is caused by the presence of undetected antidonor HLA antibodies present in the recipient at the time of transplantation. Once circulation is reestablished to the newly implanted allograft, these antibodies immediately bind to HLA antigens expressed on donor endothelium resulting in endothelial damage and immediate graft thrombosis. This may be noticed by the transplant surgeon following revascularization of the graft by softening or flaccidity of the kidney, or cyanosis or mottling of the graft surface. It may also occur within several hours after implantation and not be evident in the operating room. Pathologically, this is evident as polymorphonuclear leukocyte accumulation in the glomerular and peritubular capillaries, endothelial damage, and diffuse microcirculatory thrombosis (
90). Anuria with complete absence of allograft function and absence of blood flow to the graft is invariably the result. No therapy has been found to be effective for hyperacute rejection, and immediate graft nephrectomy is generally indicated. Donor-specific antibody may be detected in a repeat crossmatch at that time or later. The inability to detect donor-specific antibodies should not deter the diagnosis of HAR, as at the time of HAR, donor-specific antibodies may be adsorbed onto the rejected allograft, and may not reappear in the circulation until weeks later. Additionally, non-HLA antigens, such as the endothelial monocyte antigen, may be the target of antidonor antibodies and lead to HAR (
91,
92,
93). These are highly unlikely to be detected by standard crossmatch techniques and need to be specifically looked for. There has been an entity called “delayed HAR,” coined to describe sudden severe graft dysfunction or thrombosis
24 to 48 hours after implantation. This poorly characterized syndrome, on occasion reversible, may result from the same mechanism with perhaps a very low titer or low affinity antidonor antibodies, often combined with a component of cellular rejection (
94).
Vascular Occlusion
Other causes of immediate nonfunction with absence of renal blood flow by ultrasonography or other imaging include renal vein or artery thrombosis. This is reported to occur in up to 2% to 6% of all renal transplants, with over 90% presenting in the first 7 days after transplantation (
95,
96). A higher incidence was noted with donors at both extremes of age, female donors, and with prolonged total ischemic time. Renal vein thrombosis is almost twice as frequent as renal artery thrombosis, and often presents with sudden pain and swelling of the allograft. Graft rupture may occur and represents a surgical emergency. Angiography, if immediately available, may be of use in distinguishing HAR from arterial thrombosis, since in the former condition, renal arterial patency is generally maintained, although secondary thrombosis of the renal artery or vein can occasionally be seen secondary to stasis of blood flow. The demonstration of thrombosis of the renal artery or vein should lead to immediate surgical reexploration of the patient, as the allograft may be salvaged if arterial or venous thrombosis is recognized shortly after its occurrence and renal circulation is successfully reestablished. However, the window of opportunity for recovery of function is small, as the nonperfused allograft at body temperature (warm ischemia) will suffer irreversible injury within a brief period of time. A delay of several hours to obtain further imaging of a kidney that has no flow by ultrasonography is rarely justified if salvage of renal function is anticipated. Transplant renal artery thrombosis may be due to one of several causes: endothelial damage, dissection of the artery, kinking due to a shift in position of the allograft, or, less likely, extrinsic compression due to hematoma or lymphocele. Transplant renal vein thrombosis may similarly be due to a variety of causes including damage to the vein during preservation or implantation, external compression, or kinking due to a shift in allograft position. A thrombophilic state in the recipient may also be a contributing factor in some cases (
97).
Pathologically, the characteristic microcirculatory thrombosis of HAR may extend into larger-sized arteries and veins, including the main renal vein and artery if there is renal infarction. The histology of primary renal vein thrombosis is characterized by hemorrhagic infarction of the allograft with thrombosis of the venous microcirculation, and may be distinguished from HAR by the absence of microthrombosis on the arteriolar side of the circulation. Primary thrombosis of the transplant renal artery usually results in bland renal infarction.
Another clinical entity that may present with poor allograft perfusion and function in the immediate postimplantation period is severe preservation injury. This uncommon entity occurs following complications of organ recovery, preservation, or implantation, and may result from excessive warm or cold ischemic times. Pathologically, there are findings of severe ATN, on occasion accompanied by evidence of endothelial injury and thrombotic changes in the glomerular microcirculation. There is a high primary nonfunction rate in these allografts, particularly if there has been vascular injury, and those that do recover function are most often significantly compromised. There is no defined treatment to prevent or minimize irreversible injury or to promote more rapid recovery.
Delayed Graft Function
DGF is defined as the need for dialysis during the first week after transplantation, while slow graft function describes patients who do not have an adequate decline in creatinine or urine output immediately after transplantation (i.e., <30% decline in serum creatinine within 48 hours or <1,000 mL urine output/day), but do not require dialysis. The pathogenesis of both these situations is thought to be similar, different only in degree, caused by ischemia/reperfusion injury resulting in tubular damage (
89). Pathologically, ATN is seen, postulated to be a result of tubular cell damage due to ischemia, free radical formation during reperfusion, activation of endothelial cells which increases expression of MHC class II and adhesion molecules, leukocyte diapedesis, increased cytokine expression, activation of mitochondrial apoptotic pathways, and damage due to cold storage (
98,
99,
100,
101,
102,
103). The reported incidence of DGF is quite variable, ranging from 5% to 40% for cadaveric transplants compared to 2% to 5% for living related donors (
104). Risk factors for DGF include increased cold ischemia time, use of an expanded criteria donor (ECD) kidney, elevated donor creatinine at time of organ harvesting, donor hypertension, kidney from a non-heartbeating donor, recipient panel of reactive antibodies (PRA) >50%, recipient race, perioperative blood pressure, degree of HLA mismatch, recipient of prior transplantation, and method of organ preservation (
104,
105,
106,
107,
108). The higher incidence of DGF in patients with high PRA suggests that immunologic factors also play an etiologic role in some cases (
105,
109,
110). Any evidence of clear-cut immune attack contributing to or masquerading as DGF should be treated aggressively (see below). The mean duration of DGF varies between studies, averaging 7 to 10 days (
111,
112). DGF is associated with worse long-term graft outcome, an effect that appears to be stronger the longer the duration of graft dysfunction (
104,
113,
114,
115). Results between studies have varied, but this effect is likely independent of acute rejection, leading to a graft half-life of 9.7 years compared to 14.2 years in those patients without DGF (
114,
116).
DGF blinds the clinician to what may be occurring immunologically in the kidney. Since there is oliguria and an elevated serum creatinine whose level in many patients is
determined by dialysis, clinically detecting a superimposed acute rejection becomes difficult without a biopsy. The incidence of acute rejection in patients with DGF that persists for 7 to 10 days is significant, varying from 18% to 48% (
117,
118,
119). The presence of acute rejection in biopsies of patients with DGF was associated with increased primary nonfunction and worse long-term graft survival (
117,
119). A transplant biopsy should be performed in patients with persistent DGF (>7days), since early detection and treatment of superimposed rejection is likely to improve graft function and survival, although this has not been formally studied. Repeat imaging of the allograft should also be performed at least once during the first week of DGF, and weekly during prolonged DGF to assure that graft thrombosis has not occurred, and that there is no obstruction to urine flow in the kidney recovering from DGF.
Strategies to limit DGF include improved organ preservation, shorter cold and warm ischemia times, and improved care of brain-dead donors. Intraoperative administration of a polyclonal antilymphocyte globulin (Thymoglobulin) may decrease the incidence of DGF. In one study, 58 patients were randomized to receive Thymoglobulin intraoperative or 6 hours after reperfusion (
120). The incidence of DGF was 14.8% in the intraoperative group compared to 35.5% in the postprocedure group (
P <0.05). Further, the intraoperative group had a decreased length of stay and lower serum creatinine at discharge. The long-term clinical benefit is unclear since renal function at 1 year was similar between groups. Studies to prevent DGF or to improve recovery from DGF using anti-ICAM1 antibodies have not shown any benefit, and the growth factor IGF-1 is still being studied (
121,
122).
There is no specific treatment for DGF to accelerate recovery of renal function. Management of immunosuppressive medications during DGF has been the subject of numerous investigations. However, no widely agreed upon strategy has been established. The goal is to balance adequate immunosuppression to prevent acute rejection against limited exposure to medications with a potential adverse impact on renal recovery. Most strategies have attempted to minimize exposure to calcineurin inhibitors (CIs) during DGF due to their nephrotoxic effects—renal vasoconstriction and direct tubular toxicity—while preventing rejection with the use of antilymphocyte antibody therapy (antithymocyte globulin, OKT3, or anti-IL2 receptor antibodies). In these treatment strategies, calcineurin inhibitor administration is often delayed until there is adequate recovery of renal function (often defined as serum creatinine <3 mg/dL). Other strategies have included antibody therapy with low-dose cyclosporine/tacrolimus, or sirolimus or mycophenolate mofetil (MMF) (or both) until renal function recovers (
123,
124,
125,
126,
127). Some advocate immediate administration of full-dose calcineurin inhibitors regardless of renal function (
128).
Early studies comparing antithymocyte globulin or OKT3 “prophylaxis” to immediate cyclosporine 10 mg/kg/day administration in patients with DGF suggested that cyclosporine use during DGF prolonged recovery (
127,
129,
130). However, low blood levels of cyclosporine immediately after transplantation are associated with an increased risk of acute rejection (
131). More recent studies have compared the time to recovery of renal function from DGF using two different immunosuppressant strategies: (a) administration of antithymocyte globulin while withholding calcineurin inhibitors and (b) immediate administration of CIs without antithymocyte globulin. The duration of DGF in patients treated immediately with CIs (cyclosporine 5 to 8 mg/kg/day or tacrolimus 0.15 to 0.3 mg/kg/day) compared to those treated initially with antithymocyte globulin was longer in one study but not in others (
125,
132,
133,
134). Sequential therapy using antithymocyte globulin or OKT3 until renal recovery followed by initiation of CI is safe and effective but may be associated with an increased risk of infection (
135). Anti-IL-2 receptor antibodies, in conjunction with cyclosporine and azathioprine or mycophenolate mofetil, have also been used successfully to decrease the incidence of acute rejection in patients with DGF (
136,
137).
Sirolimus is an attractive alternative to immediate CI use in patients with DGF: it is an effective immunosuppressive without vasoconstrictive effects or inherent nephrotoxicity. However, its potent antiproliferative activity may prolong recovery from DGF. In animal models, sirolimus use impairs resolution of ATN, and its use has been associated with prolongation of DGF (
111,
112,
138,
139). Prolonged recovery from DGF did not affect renal function at 1 year (
112).
Mycophenolate mofetil has not been associated with significant nephrotoxicity and does not inhibit the proliferation of renal tubule epithelial cells in vitro. It appears safe to administer it during episodes of DGF.
No single immunosuppressive strategy is clearly superior to another during DGF. Careful monitoring of allograft status is essential, with those patients who have not recovered function within 7 to 10 days undergoing allograft biopsy.
Urologic Complications
Urologic complications—ureteral obstruction and urine extravasation—are another cause of poor allograft function in the immediate postoperative period.
Transplant ureteral obstruction in the immediate postoperative period may represent a technical problem such as ureteral necrosis due to inadequate vascular supply, or poor surgical technique in creating the uretero-vesicular anastomosis. External factors such as compression of the ureter by a hematoma or kinking of the ureter due to poor positioning of the graft are also potential causes of obstruction to urine flow. If there is good initial function but ureteral obstruction, hydronephrosis will develop quickly. However, if DGF is present, a urologic abnormality may not be evident until recovery of function, as urine volumes recover. Periodic imaging of the transplanted kidney and ureter is essential to ensure that the allograft has not begun to recover function, but oliguria continues due to obstruction.
Damage to the transplanted ureter or faulty ureteroneocystostomy can also result in extravasation of urine out of the bladder or ureter. This urine will most commonly either collect in the perinephric area or drain via the fresh transplant incision. Less often, it may enter the peritoneal cavity or track into the scrotum or labia. Diagnosis of a urine leak can be made by analysis of fluid collected from wound drainage or aspirated from a collection. Simultaneous measurement of the sodium, potassium, and creatinine concentration should easily distinguish between urine leaking into the tissue and normal tissue fluid that might collect in a lymphocele or drain from the wound. Normal extracellular tissue fluid should have a creatinine, sodium, and potassium concentration nearly identical to plasma, whereas urinary potassium and creatinine concentrations will be much higher than that in the serum, and the sodium concentration lower. Radionuclide imaging may also be of value in the diagnosis of urinary extravasation. Radiotracer exiting the urinary system into the soft tissues strongly suggests a leak. This type of test may, however, be of limited value if allograft function is poor and background counts are high. Confirmation of the presence of and the site of a leak can be obtained by cystoscopy or following placement of a nephrostomy tube. A small volume of urine output per urethra does not exclude the diagnosis of ureteral obstruction or urinary leak. Urinary retention from bladder outlet obstruction may also lead to oliguria with no fall in serum creatinine. This occurs most commonly in men at risk from prostatic hypertrophy, or in diabetics with neurogenic bladder dysfunction.
The management of ureteral obstruction generally requires the placement of a ureteral stent to allow for decompression of the urinary system. If a stent bypassing the obstruction cannot be placed, a nephrostomy tube may be necessary. Alternatively, reoperation and reimplantation of the ureter may be indicated if the obstruction is due to obstruction at the ureteroneocystostomy site.
The management of urinary extravasation is directed toward improved drainage of urine into the bladder via a ureteral stent, or external drainage via nephrostomy tube placement. Either will reduce the hydrostatic pressure within the urinary system and encourage healing of the leak. If the ureter has completely dehisced from the bladder, reimplantation may be indicated. Mild urinary extravasation with a fundamentally sound ureteroneocystostomy may be managed with bladder drainage. More significant leaks usually require reoperation, either immediate or after controlling the leak with a nephrostomy/stent combination.
Catheter obstruction should always be considered in evaluating anuria or oliguria following transplantation. This should be readily evident if imaging reveals bladder outlet obstruction. The Foley catheter may be kinked or obstructed by a blood clot. Flushing the catheter with sterile saline should either relieve the obstruction or indicate the need to replace the catheter. Measures to relieve bladder outlet obstruction should be undertaken immediately to prevent disruption of the uretero-vesicular anastomosis due to elevated intraluminal pressure within the bladder.