Fig. 4.1
A normal high-resolution esophageal manometry (HREM) tracing, with time on the x-axis and esophageal distance on the y-axis
4.1.1 Motility Disorders Diagnosed by High-Resolution Esophageal Manometry
Motility disorders diagnosed by HREM include achalasia (Figs. 4.2, 4.3, and 4.4), scleroderma (Fig. 4.5), diffuse esophageal spasm (Fig. 4.6), nutcracker esophagus (Fig. 4.7), and ineffective esophageal motility (Fig. 4.8).
4.1.1.1 Achalasia
Three manometric subtypes can be diagnosed by HREM:
Treatment outcomes have been shown to differ among these subtypes. Type 2 achalasia is most responsive to treatment by pneumatic dilation or laparoscopic Heller myotomy. Type 1 is more refractory to treatment, and Type 3 is the least amenable to either treatment. Given the greater risks of surgery versus pneumatic dilation, one proposal suggests that Type 2 patients be treated with pneumatic dilation and Type 1 patients be treated with surgery, if unresponsive to medical therapy. Botox injection should be reserved for Type 3 patients or any Type 1 or Type 2 patient who is a poor candidate for pneumatic dilation or surgery because of medical comorbidities.
4.1.1.2 Scleroderma
HREM in patients with scleroderma (Fig. 4.5) shows evidence of low to absent LESP, accompanied by weak or absent lower esophageal body contraction amplitude. Striated muscle contraction in the upper esophagus may be normal.
4.1.1.3 Diffuse Esophageal Spasm
In this disease, more than 20 % of swallows studied with HREM (Fig. 4.6) feature simultaneous contractions, but peristalsis is present on other swallows, and the LES relaxes normally. Incomplete bolus transit is often present.
4.1.1.4 Nutcracker Esophagus
Here, esophageal body contraction amplitude is elevated above 180 mmHg (Fig. 4.7). There may be incomplete LES relaxation, but bolus transit is usually complete. Clinical correlation is important in these situations, as this finding can be detected in some normal patients. Symptoms of chest pain, rather than dysphagia, are more suggestive of actual pathology.
4.1.1.5 Ineffective Esophageal Motility
Findings in these patients do not meet criteria for other motility disorders. LES relaxation is complete, but there may be low-amplitude or nontransmitted contractions in the esophageal body (Fig. 4.8). Bolus transit may be complete or incomplete, and abnormal swallows may be seen alongside normal peristaltic contractions. This finding can accompany a diagnosis of GERD.
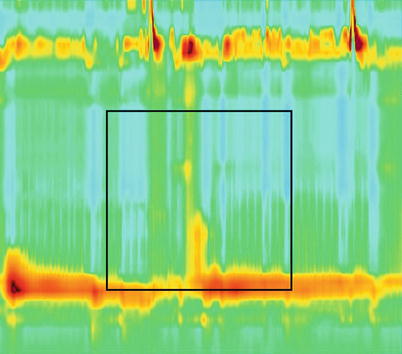
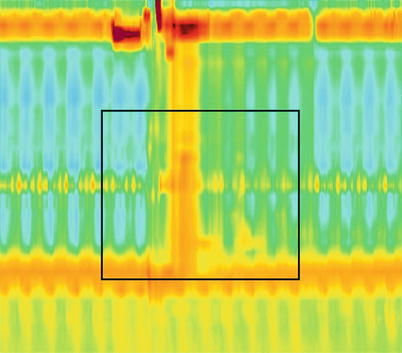
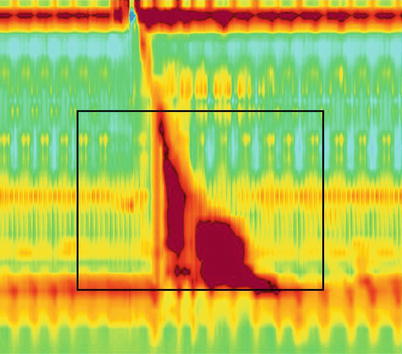
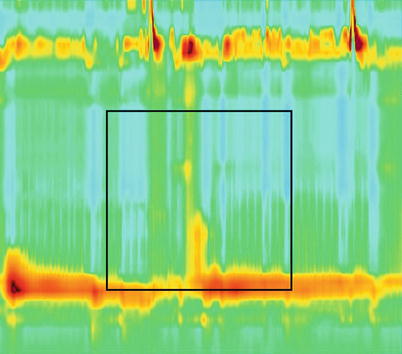
Fig. 4.2
Achalasia, type 1. This HREM tracing shows the swallow pattern of the classic subtype. Absent peristalsis is required for diagnosis. Esophageal pressurization is fully absent. Lower esophageal sphincter pressure (LESP) may be elevated, with poor LES relaxation
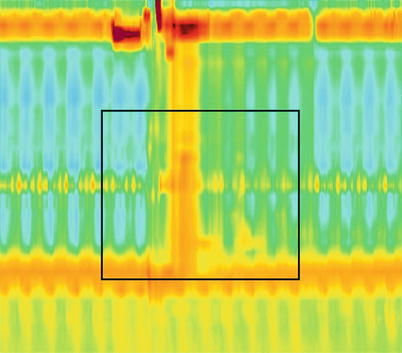
Fig. 4.3
Achalasia, type 2. This HREM tracing shows the swallow pattern of the esophageal compression subtype. This diagnosis requires absent peristalsis and panesophageal pressurization of the esophagus in more than 20 % of swallows. LESP may be elevated, with poor LES relaxation
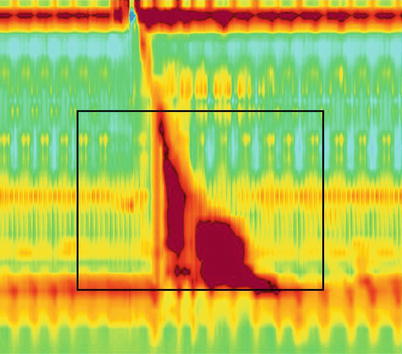
Fig. 4.4




Achalasia, type 3. This HREM tracing shows the swallow pattern of the spastic subtype. This diagnosis requires high-amplitude spastic contractions of the esophagus in more than 20 % of swallows, with or without preservation of distal peristalsis. LESP may be elevated, with poor LES relaxation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








