In recent years, endoscopic ultrasonography (EUS) has emerged as an important tool for the diagnosis and management of pancreaticobiliary disease. The close proximity of the echoendoscope to the biliary system allows detailed imaging of the gallbladder and adjacent structures. EUS is useful for the detection of occult cholelithiasis and biliary sludge and in the evaluation of suspected choledocholithiasis. It can be used to classify and predict neoplasia in polypoid lesions of the gallbladder and also to diagnose and stage gallbladder carcinoma. This article reviews the use of EUS in these diseases of the gallbladder.
Endoscopic ultrasonography (EUS) was introduced in 1980 and has developed considerably in the past 30 years. Primarily useful for the detection and staging of gastrointestinal cancers, EUS is now established as an important diagnostic modality that is necessary for the optimal management of gastrointestinal disease. EUS and magnetic resonance cholangiopancreatography (MRCP) have been largely responsible for the diminishing role of diagnostic endoscopic retrograde cholangiopancreatography (ERCP). EUS has become an essential tool for the complete pancreaticobiliary endoscopist.
EUS is an accurate modality for imaging gallbladder structures because of the close proximity of the duodenum to the gallbladder and extrahepatic biliary tree ( Fig. 1 ). EUS is considered superior to transabdominal ultrasonography (US) for imaging the biliary system, using higher ultrasound frequencies (5–12 MHz vs 2–5 MHz). EUS can differentiate the double-layered structure of the gallbladder wall and provide higher resolution for imaging small polypoid lesions. Both types of echoendoscopes, radial and linear (transverse and longitudinal imaging, respectively), can be used to image the biliary tree. In addition to imaging, EUS-guided needle puncture using the linear instrument enables transluminal aspiration of tissue for diagnosis and provides direct access to the biliary tree for therapeutic interventions. The development of intraductal ultrasonography (IDUS) miniprobes has further advanced the study of pancreaticobiliary tree disorders.

Clinical situations in which EUS can be used for evaluation of gallbladder disease include investigation of suspected cholelithiasis or biliary sludge, evaluation of suspected choledocholithiasis, imaging of polypoid lesions of the gallbladder, and diagnosis and staging of gallbladder cancer. This article reviews the use of EUS in these settings.
EUS instruments
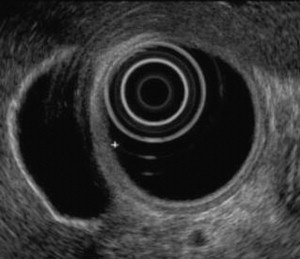
The currently available instruments for biliary imaging with EUS include radial and linear echoendoscopes and catheter-based IDUS probes. There are 2 types of echoendoscopes, denoted radial or linear based on the piezoelectric crystals that generate the EUS image. In EUS, ultrasound pulses are generated by a transducer containing a piezoelectric crystal that converts an electronic pulse into an acoustic wave that propagates into the tissue. The same transducer then detects returning acoustic waves that contain information about the tissue through which the waves have propagated. In a radial echoendoscope, the crystals are arranged in a band around the shaft of the endoscope, perpendicular to the long axis of the instrument, generating a cross-sectional image ( Fig. 2 ). Radial scanning instruments provide detailed circumferential images, making them useful for orientation, and electronic radial instruments with Doppler capabilities help distinguish small vessels from ducts and improve vascular staging. In a linear echoendoscope, the crystals are arranged along one side of the endoscope’s tip, generating a longitudinal image parallel to the long axis of the instrument. Only the linear echoendoscope can be used to guide fine-needle puncture. The ability of the linear echoendoscope to provide scanning in the same plane as the instrument’s shaft allows the endoscopist to trace the path of a needle as it is inserted out of the working channel of the echoendoscope ( Fig. 3 ). Hence, a linear echoendoscope can be used for diagnostic evaluation and to facilitate interventional EUS, such as EUS-guided fine-needle aspiration, EUS-guided injection therapies, and EUS-guided drainage procedures. The availability of high-frequency catheter ultrasound probes allows imaging from within the biliary tree. IDUS probes are placed during ERCP, most often over a guide wire, and can be advanced into the common bile duct, hilar region, intrahepatic ducts, gallbladder, and across biliary strictures.


EUS technique
Endoscopic expertise using a duodenoscope (radial and linear echoendoscopes are primarily oblique viewing) and a detailed understanding of the regional cross-sectional anatomy are essential to obtain and interpret EUS images of the biliary tree. The optimal position for imaging the gallbladder is variable. The gallbladder is most commonly and easily imaged from the duodenal bulb but may also be imaged from the antrum or descending duodenum. EUS imaging is usually commenced in the duodenal bulb with the echoendoscope in the long position, with the endoscope advanced to the superior angle of the duodenal bulb and the tip deflected downward. To image the body, fundus, and neck of the gallbladder, the transducer is moved slowly along the course of the gallbladder using torque and tip deflection as needed. The normal gallbladder appears as a large fluid-filled (anechoic) structure with a thin, layered wall ( Fig. 4 ). With the echoendoscope in the same position, the common bile duct and common hepatic duct are seen in their long axis alongside and superficial to the portal vein ( Fig. 5 ). When it is dilated, the bile duct is often readily recognized. If Doppler is available, it can be used to confirm bile duct identification and distinguish the duct from vessels such as the portal vein or gastroduodenal artery. Imaging is then continued with the echoendoscope in the short position at the level of the papilla, similar to the endoscope position when performing ERCP. In this position, the bile duct is identified at the periampullary portion of the pancreas and followed proximally to the level of the bifurcation and gallbladder.

EUS technique
Endoscopic expertise using a duodenoscope (radial and linear echoendoscopes are primarily oblique viewing) and a detailed understanding of the regional cross-sectional anatomy are essential to obtain and interpret EUS images of the biliary tree. The optimal position for imaging the gallbladder is variable. The gallbladder is most commonly and easily imaged from the duodenal bulb but may also be imaged from the antrum or descending duodenum. EUS imaging is usually commenced in the duodenal bulb with the echoendoscope in the long position, with the endoscope advanced to the superior angle of the duodenal bulb and the tip deflected downward. To image the body, fundus, and neck of the gallbladder, the transducer is moved slowly along the course of the gallbladder using torque and tip deflection as needed. The normal gallbladder appears as a large fluid-filled (anechoic) structure with a thin, layered wall ( Fig. 4 ). With the echoendoscope in the same position, the common bile duct and common hepatic duct are seen in their long axis alongside and superficial to the portal vein ( Fig. 5 ). When it is dilated, the bile duct is often readily recognized. If Doppler is available, it can be used to confirm bile duct identification and distinguish the duct from vessels such as the portal vein or gastroduodenal artery. Imaging is then continued with the echoendoscope in the short position at the level of the papilla, similar to the endoscope position when performing ERCP. In this position, the bile duct is identified at the periampullary portion of the pancreas and followed proximally to the level of the bifurcation and gallbladder.
EUS and occult cholecystolithiasis or microlithiasis
Gallstone disease is common in the United States, with a prevalence of approximately 10% to 15% among adults. The gold standard for evaluation for gallbladder stones is transabdominal US, which has been shown to have a sensitivity of 98% for the detection of cholecystolithiasis. However, US may miss gallstones in some patients, particularly those with small gallstones, and a high clinical suspicion for cholelithiasis may make additional studies warranted. Given its higher-frequency resolution and the closer proximity of the echoendoscope to the biliary system compared with US, EUS can be used to evaluate for occult cholecystolithiasis among patients in whom gallbladder stones are suspected but cannot be confirmed after US ( Fig. 6 ).
The performance of EUS in the diagnosis of occult cholelithiasis was evaluated by Dahan and colleagues. They prospectively studied 45 patients with acute idiopathic pancreatitis (n = 25) or transient biliary-type pain associated with fever, jaundice, and increased liver enzymes (n = 20). All patients previously had at least 2 normal transabdominal US scans. EUS showed gallbladder stones or sludge in 26 of the 45 patients, with the diagnosis of macrolithiasis or microlithiasis confirmed at cholecystectomy in 23 of the 26. Among the 19 patients in whom EUS did not suggest cholelithiasis, 7 underwent cholecystectomy for other reasons, and the others were followed clinically; only 1 patient was subsequently diagnosed with cholelithiasis. EUS therefore had a sensitivity of 96% for detection of occult cholelithiasis (94% for macroscopically visible stones) and a specificity of 86%. This result compared with a sensitivity of 67% for the microscopic examination of duodenal bile from the same patients ( P <.03).
Liu and colleagues performed EUS in 18 patients with acute pancreatitis in whom no cause was identified after history, laboratory evaluation, and conventional abdominal imaging. Of these patients, all had undergone at least 1 US, 9 had multiple US, and 6 had also been evaluated with computed tomography (CT); each of these imaging studies had failed to detect biliary calculi. EUS revealed small gallstones in 14 of the 18 patients (78%); 10 of these 14 also had gallbladder sludge ( Fig. 7 ), and 3 had concomitant choledocholithiasis. The diagnosis of cholelithiasis was confirmed at cholecystectomy in all 14 patients. The 4 patients without cholelithiasis by EUS remained free of gallstone disease as determined by laboratory, clinical, and US follow-up for a median of 22 months. Similar results were obtained by Thorbøll and colleagues, who evaluated 35 consecutive patients with biliary colic who had undergone at least 1 (mean = 2.1) normal US. EUS showed cholecystolithiasis in 18 of the 35 (52%). Seventeen of these patients underwent cholecystectomy, which confirmed the presence of stones in the gallbladder in 15 of 17 (88%).
EUS and choledocholithiasis
Choledocholithiasis is a frequent complication of gallstone disease, occurring in 15% to 20% of patients with symptomatic cholelithiasis. Historically, ERCP has been considered the gold standard for the diagnosis of common bile duct stones. However, ERCP is an invasive procedure that is associated with a small, but not insignificant, risk of serious complications such as pancreatitis, cholangitis, perforation, and hemorrhage, and thus should ideally be reserved for patients with proven common bile duct stones who require endoscopic therapy. It is therefore important to use initial safe, noninvasive diagnostic modalities for choledocholithiasis to select appropriate patients for ERCP.
In recent years, EUS has emerged as a minimally invasive procedure that is useful for the diagnosis of common bile duct stones ( Fig. 8 ). Several studies have been performed to compare the performance of EUS with those of conventional imaging techniques such as US and CT, as well as a newer modality, MRCP. The performance of EUS has also been compared with ERCP. In addition, several groups have recently proposed and studied an EUS-guided ERCP approach for diagnosis of choledocholithiasis among patients with intermediate probability of common duct stones.
Transabdominal US is routinely used for the diagnosis of cholelithiasis, but it is not sensitive in the detection of common bile duct stones. In a prospective series of 155 patients with suspected choledocholithiasis, 51 of whom had common duct stones at ERCP that were later confirmed by sphincterotomy or surgery, Sugiyama and Atomi found that EUS had a higher sensitivity (96%) than US (63%) for detection of choledocholithiasis ( P <.001). The specificity and accuracy of EUS (100% and 99%, respectively) for common duct stones were also significantly higher than those of US (95% and 83%). The extrahepatic bile duct was wholly displayed in 96% of patients by EUS but in only 60% by US ( P <.0001). Amouyal and colleagues obtained similar results when they evaluated 62 consecutive patients with suspected common bile duct stones. They found that EUS was more sensitive (97%) than US (25%, P <.0001) and had a significantly higher negative predictive value (97% vs 56%; P <.0001). Specificity and positive predictive value of the 2 modalities were not significantly different.
The sensitivity of CT for common duct stones, although higher than that of US, is lower than the sensitivity of EUS. Earlier studies performed before helical CT scanning was widely available, found that CT had a sensitivity for detection of common bile duct stones ranging from 71% to 75%. More recent investigations have found improved test performance using helical CT, albeit not equal to that of EUS. In a prospective study of 52 inpatients referred for ERCP for suspected choledocholithiasis, Polkowski and colleagues compared the performance of EUS with helical CT. Thirty-four of the 50 patients (68%) who underwent successful ERCP (which was considered the gold standard) were shown to have bile duct stones. The sensitivity, specificity, and accuracy of EUS (91%, 100%, and 94%, respectively) were higher than those of CT (85%, 88%, and 86%), but these differences were not statistically significant. Likewise, Kondo and colleagues evaluated the performance of EUS versus helical CT in 28 patients considered likely to have common bile duct stones. Twenty-four of the 28 patients (85.7%) were found to have choledocholithiasis using a combination of ERCP and intraductal US, which was considered the gold standard. The sensitivity of EUS (100%) was higher than that of helical CT (88%). Among patients with small (1–4 mm) common duct stones, sensitivity of EUS remained 100%, whereas sensitivity of CT fell to 67%. The investigators concluded that, when immediate diagnosis and treatment are required, EUS should be the first-choice study because of its improved sensitivity for small stones.
MRCP, as a noninvasive and increasingly available study, has been advocated as an alternative to EUS for the evaluation of choledocholithiasis, particularly among patients with low to intermediate probability of common bile duct stones. Schmidt and colleagues prospectively evaluated 57 patients with suspected choledocholithiasis using MRCP and EUS. If either study detected choledocholithiasis or unexplained common bile duct dilation, ERCP or intraoperative cholangiography was considered the gold standard for final diagnosis. Among patients with negative EUS and MRCP, the gold standard was clinical follow-up. Common bile duct stones were found in 18 of the 57 patients (31.6%) and confirmed by ERCP in 17 patients and by intraoperative cholangiography in 1 patient. Sensitivity, specificity, and accuracy for MRCP were 94.8%, 94.4%, and 94.7%, respectively. Corresponding values for EUS, which were not statistically different, were 97.4%, 94.4%, and 96.5%. A systematic review of 5 prospective studies comparing EUS and MRCP, with a pooled data set of 301 patients, yielded similar results. The aggregated sensitivities of EUS and MRCP for the detection of choledocholithiasis were 93% and 85%, respectively, and their aggregated specificities were 96% and 93%. The aggregated positive predictive values were 93% and 87%, with negative predictive values of 96% and 92%. The systematic review showed no statistically significant differences between EUS and MRCP for the detection of choledocholithiasis.
Several studies have compared the performance of EUS with ERCP in the detection of common duct stones, and most have failed to find a significant difference in test performance between the 2 procedures. Palazzo and colleagues retrospectively evaluated 219 patients who had undergone EUS and ERCP for evaluation of suspected choledocholithiasis. Common bile duct stones were detected by ERCP in 77 patients, and, in all of these cases, stones were also diagnosed by EUS. In 19 patients, choledocholithiasis was diagnosed by EUS but not confirmed by ERCP, and EUS and ERCP failed to diagnose common duct stones in 1 patient later found to have choledocholithiasis during surgical exploration. EUS and ERCP findings were therefore concordant in 91.3% of cases. In a prospective study, Prat and colleagues evaluated 119 patients strongly suspected of choledocholithiasis, and performed EUS and ERCP. Endoscopic sphincterotomy with basket and balloon exploration of the common bile duct was considered the gold standard for diagnosis of choledocholithiasis and was performed in all but 1 case; 78 (66%) of the patients were found to have common bile duct stones at sphincterotomy. The findings at ERCP and EUS were concordant in 95% of cases. The sensitivity, specificity, positive predictive value, and negative predictive value of EUS were 93%, 97%, 98%, and 88%, respectively. These values were not significantly different than those for ERCP (89%, 100%, 100%, and 83%).
Given the comparable test performances of EUS and ERCP, and the risk of morbidity associated with ERCP, a strategy has been proposed in which EUS is used as the initial diagnostic test before ERCP, particularly for patients with intermediate or lower probability of common bile duct stones. Several recent randomized controlled trials have evaluated this approach. Karakan and colleagues randomized 120 patients with an intermediate risk for choledocholithiasis (baseline probability of bile duct stones no more than 67%) in a 1:1 fashion to EUS or ERCP as their initial study. Those who underwent EUS first (the EUS-guided ERCP group) proceeded to ERCP only if choledocholithiasis was detected on EUS, and sphincterotomy and stone extraction were performed if either procedure showed common duct stones. Among patients in the ERCP group, sphincterotomy and stone extraction were performed if the cholangiogram revealed choledocholithiasis. There was a trend for an increased number of endoscopic procedures in the ERCP group (mean 1.63 procedures per patient) compared with the EUS-guided ERCP group (mean 1.38 procedures per patient), although this difference was not statistically significant. There was also a trend for an increased rate of complications in the ERCP group (10%) compared with the EUS-guided ERCP group (1.7%; P = .06), and Kaplan-Meier analysis showed a significantly higher rate of negative outcomes in the ERCP group ( P = .049). Polkowski and colleagues, in a study of similar design, randomized 100 patients with intermediate probability of common bile duct stones to EUS or ERCP first. They found no significant difference in the number of procedures performed in the EUS-guided ERCP versus ERCP groups (1.42 and 1.31 procedures per patient, respectively), but more patients in the ERCP group (40%) than the EUS-guided ERCP group (10%; P <.001) experienced a negative outcome. A recent systematic review that included 423 patients from the Polkowski and Karakan studies as well as 2 other randomized controlled trials, showed that the EUS-guided ERCP approach avoided ERCP in 67% of patients when EUS did not show choledocholithiasis. The risk of undergoing an additional endoscopic procedure was higher in the EUS-guided ERCP group (risk ratio [RR] 2.46, P = .004). The EUS-guided ERCP approach was also associated with a significantly lower risk of overall complications (complication rate 6.6% vs 19%; RR 0.35; P <.001) and post-ERCP pancreatitis (RR 0.21, P = .03).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




