The technique of robotic partial nephrectomy continues to evolve, but the goals remain the same. Achievement of pentafecta outcomes is difficult to obtain; however, surgeons should continue to strive for this standard of excellence. The future continues to be bright for patients and surgeons alike in continuing to perform robot-assisted partial nephrectomy.
Key points
- •
Robotic partial nephrectomy is no longer an emerging field but has been widely accepted as a safe and appropriate management technique for small renal masses.
- •
Future directions for robotic partial nephrectomy include identifying patient-specific outcomes to measure improvement. The pentafecta assessing both early and late outcomes may provide this road map for comparison.
- •
The usage of technologic advances, patient selection, and pathway creation will provide further implementation of this technology and continue to improve surgical results.
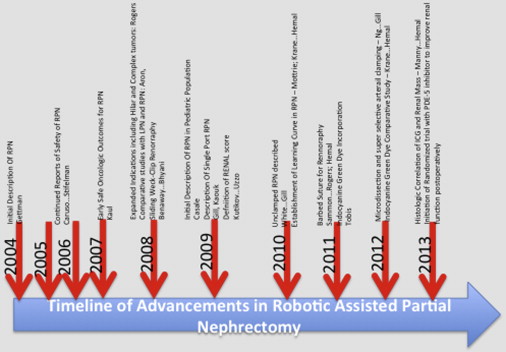
Robotic partial nephrectomy (RPN) has been widely adopted for the management of renal masses amenable to extirpative surgery. Its role in providing the advantages of a minimally invasive procedure while still safely sparing nephrons has led to increased adoption. As this technology has been adapted in many high-volume institutions, several techniques and technologies have been implemented to provide improved outcomes; the nomenclature to ensure obtaining these goals is also evolving. Fig. 1 demonstrates a timeline of advances that have occurred throughout the development of RPN.
The trifecta is an established gambling term for describing prediction of the exact order of the first 3 horses finishing a race. This terminology has been adapted to describe outcomes of patients undergoing RPN. As described from the University of Southern California Group, the trifecta in RPN includes negative margins, no urologic complications, and a minimal decrease in renal function postoperatively. They found a trend toward an increased rate of trifecta with their most recent patients; however, the range of patients achieving this outcome was between 44% and 68%. Early reports of trifecta outcomes demonstrate that using the robotic platform seems to improve the likelihood of obtaining these. Khalifeh and colleagues note that RPN is much more likely to produce trifecta outcomes than a strict laparoscopic approach with an increase from 32% to 59% of patients.
Although the achievement of a trifecta may provide early indicators of surgical success, patients inevitably requires further follow-up to assess the success of these elements. Negative cancer margins do not necessarily correlate with long-term oncologic control. Although minimizing urologic complications is a goal, patients who experience any complication may not feel as if they have received a trifecta-worthy procedure. The authors, therefore, think the goal of performing RPN should be a pentafecta, which encompasses not only the trifecta but also includes long-term maintenance of preoperative renal function and freedom from cancer recurrence. In addition, avoidance of all complications is required not just pertaining to the urologic subset. In order to achieve a pentafecta outcome, there are several necessary components: a technically sound procedure, an appropriate patient selection, care pathway–guided perioperative management, and long-term continuity of care and follow-up. This review highlights these emerging techniques and their role in improving patient outcomes for RPN, particularly in establishing outcomes leading to a pentafecta.
Patient selection and immediate perioperative management for prevention of complications
With only 80% of small renal masses identified on computerized tomography being malignant lesions, identifying the appropriate patients to undergo surgical procedures would minimize undue morbidity. Although it was initially reported that there was a poor concordance between renal mass biopsy and final pathology, recent reports have demonstrated improved diagnostic accuracy of the renal biopsy in establishing a pathologic diagnosis. An agreement between biopsy and final pathology was 92% in a recent publication by Halverson and colleagues, and this was associated with 100% positive predictive values for a treatment algorithm based on the biopsy.
In optimizing outcomes, the perioperative patient management also plays a significant role in ensuring safe and reliable care. Several groups have established care pathways, creating standardization in perioperative management and smooth transitions for patients between the hospital and their return home. Abaza and Shah described a pathway including the minimization of narcotics, cessation of drain usage, immediate postoperative ambulation, early induction of a clear-liquid diet, and urethral catheter removal on postoperative day 1 following RPN. Through the use of the pathway, 97% of patients could be discharged from the hospital on postoperative day 1, with only a 2.7% readmission rate. The implementation of the pathway and date of surgery, as noted in the series from Patel and colleagues, was the only predictor of early discharge. In these patients, once again, a low readmission rate was documented.
Complication rates following RPN are in the 15% to 25% range based on the definition of complication used, whether this is a strict deviation from the clinical course or if this is only a complication requiring further management. Pentafecta achievement requires a smooth perioperative course by minimizing deviation from the established clinical course and understanding the potential complications before their development.
Patient selection and immediate perioperative management for prevention of complications
With only 80% of small renal masses identified on computerized tomography being malignant lesions, identifying the appropriate patients to undergo surgical procedures would minimize undue morbidity. Although it was initially reported that there was a poor concordance between renal mass biopsy and final pathology, recent reports have demonstrated improved diagnostic accuracy of the renal biopsy in establishing a pathologic diagnosis. An agreement between biopsy and final pathology was 92% in a recent publication by Halverson and colleagues, and this was associated with 100% positive predictive values for a treatment algorithm based on the biopsy.
In optimizing outcomes, the perioperative patient management also plays a significant role in ensuring safe and reliable care. Several groups have established care pathways, creating standardization in perioperative management and smooth transitions for patients between the hospital and their return home. Abaza and Shah described a pathway including the minimization of narcotics, cessation of drain usage, immediate postoperative ambulation, early induction of a clear-liquid diet, and urethral catheter removal on postoperative day 1 following RPN. Through the use of the pathway, 97% of patients could be discharged from the hospital on postoperative day 1, with only a 2.7% readmission rate. The implementation of the pathway and date of surgery, as noted in the series from Patel and colleagues, was the only predictor of early discharge. In these patients, once again, a low readmission rate was documented.
Complication rates following RPN are in the 15% to 25% range based on the definition of complication used, whether this is a strict deviation from the clinical course or if this is only a complication requiring further management. Pentafecta achievement requires a smooth perioperative course by minimizing deviation from the established clinical course and understanding the potential complications before their development.
Minimizing warm ischemia time
The role of minimizing ischemic time during tumor excision has been an evolving process. Historically, a maximum of 30 minutes of warm ischemia time was the goal, although data supporting this time point are poorly substantiated. Clinical evidence in a porcine model demonstrates safety up to 90 minutes with selective clamping ; in humans, outcomes with 55 minutes of ischemia seem to have minimal long-term functional loss.
In the authors’ experience, they noted 5 Qs responsible for the maintenance of renal function: (1) quality of residual tissue, (2) quantity of residual nephron mass, (3) quickness in resection, (4) quality noncompressing renal reconstruction, and (5) qualitative use in clamping techniques. These Qs are highlighted to ensure adequate long-term renal functional outcomes and are of particular concern in solitary kidneys or in patients with preexisting chronic kidney disease. Smith et al. reported zero ischemia or unclamped procedures in open partial nephrectomy. Gill and colleagues pioneered these techniques in minimally invasive surgery, although this initially required a complicated coordinated effort with the anesthesiologists involving pulmonary artery monitoring and transesophageal echocardiography with which they were able to create hypotension that corresponded to resection of the deepest part of the tumor. In this early cohort of patients, they found no change in serum creatinine or estimated glomerular filtration rate (eGFR) at the time of discharge. Subsequent descriptions of zero ischemia did not include the invasive monitoring or temporal hypotension. Rizkala and colleagues have used a preplaced suture that is used during an unclamped procedure when bleeding is encountered. Novak and colleagues have noted that, in 22 patients without hilar clamping, there was only one transfusion and most patients were stable for discharge on postoperative day 1. Krane and colleagues performed an unclamped RPN and compared outcomes with clamped procedures and did not note any increase in perioperative morbidity.
Techniques for surgical excision with selective versus global ischemia have also been described. Using the high 10 × magnification of the daVinci surgical system, there is an ability to perform tumor-specific devascularization without global ischemia to the kidney. In a recent multi-institutional analysis, Desai et al note that in patients undergoing selective devascularization, the percentage decrease in the estimated decrease in glomerular filtration rate was 17% for the global ischemia group versus 11% in the selective devascularization. They did find a increase in transfusion rate (24% vs 6%) and operative duration (71 minutes) for the super selective clamping, and also noted similar renal parenchymal preservation between the two groups.
An initial multi-institutional analysis of selective ischemia also found that this could improve early renal functional outcomes. Hsi and colleagues also reported that, in the immediate postoperative period, the renal functional was better preserved in the selective ischemia group; however, at a median of 6.6 months of follow-up, there was no statistical difference between global and selective ischemia.
Whether or not short-duration ischemia truly impacts renal function postoperatively has been the subject of intense debate. Recent publications have highlighted that the most important determinant of long-term renal function is volume preservation. The authors’ group assessed unclamped partial nephrectomies in a nonrandomized fashion. They did not find a statistically significant difference in the long-term follow-up for unclamped versus clamped (either with artery and vein or simply the artery) procedures. No randomized trials have been created to assess the long-term renal functional data or oncologic outcomes in order to assess the overall superiority or inferiority of an unclamped or selective devascularization procedure compared with the clamping technique.
To improve perioperative renal function, other adjuncts have been used. Rogers and colleagues have described intraoperative cold ischemia. Using a gel-port, they were successful in placing ice slush directly on the kidney during hilar clamping and tumor excision. An added benefit of this technique is the ability to remove the tumor very quickly through this port, allowing for immediate pathologic analysis with margin assessment. Olweny and colleagues have adopted the use of hyperspectral light imaging to assess renal oxygenation during RPN. They found that baseline renal hemoglobin oxygenation was inversely associated with preoperative eGFR and eGFR at the most recent follow-up, opening the door for more exploratory studies with this technology. The authors’ group is currently investigating pharmacologic treatment to minimize the deleterious effects of warm ischemia. They are in the midst of assessing the role of immediate preoperative oral sildenafil in a randomized placebo-controlled trial with a primary end point of the difference between groups in terms of the 3-month change in eGFR. The role of statins in the prevention of early and long-term renal functional outcomes has also been described.
Indocyanine green dye and near-infrared fluorescence for identification of renal vasculature, minimizing ischemia, and decreasing margin rate
Indocyanine green (ICG) dye is a well-described adjunct to surgical procedures, having been used in hepatic and ophthalmologic surgeries extensively. The incorporation of a near-infrared fluorescent camera on the daVinci Si robotic platform has allowed this technology to be introduced into minimally invasive urologic oncology. ICG is a water-soluble dye, which is highly protein bound following intravascular injection. When bound to protein, it is almost completely restricted to the intravascular space. Additionally, ICG is hepatically cleared; it poses no threat to renal functional outcomes and it is not restricted in patients with renal insufficiency.
The intravascular distribution of the ICG makes it an ideal molecule for selective arterial clamping. Following injection of the dye, within seconds, the kidney is hyperfluorescent with intravascular ICG. Therefore, injection following selective or superselective clamping of the tertiary or quaternary arteries demonstrates perfusion to the remainder of the kidney but not the areas supplied by the clamped artery. This practice ensures only regional rather than global ischemia. Borofsky and colleagues performed a multi-institutional retrospective analysis of this procedure and described the feasibility of this. In addition, they noted that in match-paired analysis comparing ICG with selective clamping to patients with global ischemia, there were significantly improved short-term renal functional outcomes with a decrease of −1.8% of GFR with ICG versus −14.9% without ICG and selective clamping. Harke and colleagues have performed a similar matched-pair analysis with 22 patients undergoing selective arterial clamping and, once again, found a short-term decrease in eGFR to be statistically significantly less following ICG injection and selective clamping.
Bilitranslocase is a transporter molecule located on the proximal tubule, and it has been reported to be downregulated in small renal masses. Following injection of the ICG, these masses appear hypofluorescent when compared with the normal renal parenchyma. An image of a clear cell renal carcinoma before and after ICG administration is seen in Fig. 2 . The reliability of this downregulation and the ability for ICG to routinely identify malignancy has been called into question. In their retrospective analysis of 100 consecutive cases with ICG administration, Manny and colleagues found that, in hypofluorescent masses, the sensitivity was only 84% and the specificity was just 57%. For clear cell renal carcinoma, there was 96% concordance noted with hypofluorescence; this was also seen from another institution.
ICG has proven to be a useful surgical adjunct to the RPN, but the true utility in terms of patient outcomes is still debated. In 94 patients, Krane and colleagues performed the largest comparative study of ICG in a nonrandomized retrospective analysis. There was a statistically significant improvement in warm ischemia time from 17 to 15 minutes, but the clinical utility of this is debatable as the margin rate and complications were similar in both cohorts. ICG is clearly an emerging technology in RPN, but how this technology will fit into improving specific patient outcomes has not been fully identified.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





