Robot-assisted radical prostatectomy (RARP) offers excellent and lasting oncologic control. Technical refinements in apical dissection, such as the retroapical approach of synchronous urethral transection, and adoption of real-time frozen section analysis of the excised prostate during RARP have substantially reduced positive surgical margin rates, particularly in high-risk disease patients. Furthermore, precision offered by the robotic platform and technical evolution of radical prostatectomy, including enhanced nerve sparing (veil), have led to improved potency and continence outcomes as well as better safety profile in patients undergoing surgical therapy for prostate cancer.
Key points
- •
Surgical management of clinically localized prostate cancer leads to superior survival when compared with observation or radiotherapy.
- •
Robot-assisted radical prostatectomy (RARP) has become the modality of choice for surgical management of prostate cancer and has evolved dramatically since its inception in the early 2000s.
- •
RARP offers excellent and lasting oncologic control.
- •
Technical refinements in apical dissection, such as the retroapical approach of synchronous urethral transection, and adoption of real-time frozen section analysis of the excised prostate during RARP, have substantially reduced positive surgical margin rates, particularly in high-risk disease patients.
- •
Precision offered by the robotic platform and technical evolution of radical prostatectomy, including enhanced nerve sparing (veil and superveil), have led to improved potency and continence outcomes as well as better safety profile in patients undergoing surgical therapy for prostate cancer.
Introduction
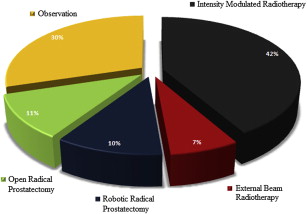
Prostate cancer (PCa) remains the most common internal organ malignancy and the second leading cause of cancer-related death in men in the United States. Most cases of PCa are clinically localized at the time of diagnosis and potentially curable by an array of therapeutic modalities, with the major options being ( Fig. 1 ) :
- 1.
Observation (active surveillance and watchful waiting)
- 2.
Radiotherapy (intensity-modulated radiation therapy and external beam radiotherapy)
- 3.
Surgery (radical prostatectomy [RP])
Each modality has its benefits and limitations, although current evidence suggests RP to be the most effective of these modalities. RP leads to better overall and cancer-specific survival when compared with observation or radiotherapy alone across all PCa risk groups (D’Amico), with patients with high-risk disease benefitting the most.
RP can be performed via an open approach or a laparoscopic approach with or without robotic assistance. In recent years, there has been a remarkable increase in the use of robot-assisted RP (RARP). In 2001, less than 0.3% of all RPs were performed robotically; however, by 2011, 61% to 80% of all RPs in the United States were being performed with robotic assistance. Recent population-based reports and meta-analyses, constituting level 2a evidence, have shown that RARP compares favorably with open RP (ORP) in terms of perioperative outcomes, perioperative complications, and functional (continence and potency) results. In terms of oncologic outcomes, whereas the few large retrospective series of RARP have reported equivalent outcomes, there is a paucity of long-term definitive data.
In this review, the various technical advances are discussed that have been made in RARP since its inception, leading to increasingly better oncologic, functional, and safety outcomes in patients undergoing RARP for management of PCa.
Historical perspective
Minimally invasive surgery (MIS) began in 1987 with laparoscopic cholecystectomy. Laparoscopic RP (LRP) was first performed by Schuessler and colleagues in 1991, and further developed and pioneered by Guillonneau and Vallancien, subsequently. The strengths and weaknesses of the MIS approach became apparent quickly. The strengths included smaller incision, less surgical site infection, blood loss, and postoperative pain, shorter hospital stay and convalescence period, and better cosmesis. On the other hand, the weaknesses included loss of haptic feedback, natural hand-eye coordination, and dexterity. These limitations made delicate dissections and anastomoses difficult, if not impossible. Robotic surgery was developed to overcome these limitations of minimally invasive laparoscopic surgery and to enhance the capabilities of surgeons performing open surgery.
RARP was first reported by Abbou and colleagues in 2000. RARP has since been refined and popularized by Menon and colleagues as a minimally invasive technique, with vastly improved ergonomics, superior outcomes, and shorter learning curve relative to LRP. Robotics has since permeated and found its application in many oncologic, nononcologic, and pediatric urologic procedures, and, more recently, in kidney transplantation.
Introduction
Prostate cancer (PCa) remains the most common internal organ malignancy and the second leading cause of cancer-related death in men in the United States. Most cases of PCa are clinically localized at the time of diagnosis and potentially curable by an array of therapeutic modalities, with the major options being ( Fig. 1 ) :
- 1.
Observation (active surveillance and watchful waiting)
- 2.
Radiotherapy (intensity-modulated radiation therapy and external beam radiotherapy)
- 3.
Surgery (radical prostatectomy [RP])
Each modality has its benefits and limitations, although current evidence suggests RP to be the most effective of these modalities. RP leads to better overall and cancer-specific survival when compared with observation or radiotherapy alone across all PCa risk groups (D’Amico), with patients with high-risk disease benefitting the most.
RP can be performed via an open approach or a laparoscopic approach with or without robotic assistance. In recent years, there has been a remarkable increase in the use of robot-assisted RP (RARP). In 2001, less than 0.3% of all RPs were performed robotically; however, by 2011, 61% to 80% of all RPs in the United States were being performed with robotic assistance. Recent population-based reports and meta-analyses, constituting level 2a evidence, have shown that RARP compares favorably with open RP (ORP) in terms of perioperative outcomes, perioperative complications, and functional (continence and potency) results. In terms of oncologic outcomes, whereas the few large retrospective series of RARP have reported equivalent outcomes, there is a paucity of long-term definitive data.
In this review, the various technical advances are discussed that have been made in RARP since its inception, leading to increasingly better oncologic, functional, and safety outcomes in patients undergoing RARP for management of PCa.
Historical perspective
Minimally invasive surgery (MIS) began in 1987 with laparoscopic cholecystectomy. Laparoscopic RP (LRP) was first performed by Schuessler and colleagues in 1991, and further developed and pioneered by Guillonneau and Vallancien, subsequently. The strengths and weaknesses of the MIS approach became apparent quickly. The strengths included smaller incision, less surgical site infection, blood loss, and postoperative pain, shorter hospital stay and convalescence period, and better cosmesis. On the other hand, the weaknesses included loss of haptic feedback, natural hand-eye coordination, and dexterity. These limitations made delicate dissections and anastomoses difficult, if not impossible. Robotic surgery was developed to overcome these limitations of minimally invasive laparoscopic surgery and to enhance the capabilities of surgeons performing open surgery.
RARP was first reported by Abbou and colleagues in 2000. RARP has since been refined and popularized by Menon and colleagues as a minimally invasive technique, with vastly improved ergonomics, superior outcomes, and shorter learning curve relative to LRP. Robotics has since permeated and found its application in many oncologic, nononcologic, and pediatric urologic procedures, and, more recently, in kidney transplantation.
Indications and contraindications
Indications are same as those for ORP. Patients with locally advanced disease (T3–T4 disease) with or without nodal metastasis (N1) may be considered as part of a multimodal/multidisciplinary management strategy and constitute a highly selected group. Relative contraindications include chronic obstructive pulmonary disease and abnormalities of cardiac function caused by difficulties in ventilation, which may occur in patients undergoing RARP as a result of exposure to pneumoperitoneum and steep Trendelenberg position. Previous abdominal/pelvic surgery may also present difficulties but is not a contraindication; a careful laparoscopic review and adhesiolysis at the time of port placement are helpful in avoiding delays and complications later during the procedure. Patient factors, such as morbid obesity, narrow pelvis, large prostate, large median lobe, or surgery in the salvage setting, increase the complexity of RARP, and hence, should be reserved for experienced surgeons.
Technical advancements in cancer control
The most important outcome to assess in patients undergoing RP is cancer control. Survival statistics and biochemical recurrence rates are the critical indicators of oncologic control, but all of these require long-term follow-up to assess and can be subject to significant reporting and interpretational biases. Positive surgical margin (PSM) rate thus remains an early oncologic outcome measure of importance when evaluating surgical therapy.
In mature RARP series, overall PSM rates have ranged between 9% and 19%, depending on the patient and surgeon characteristics. In our patients, undergoing the Vattikuti Institute Prostatectomy (VIP) technique of RARP, we have previously shown a PSM rate of 13% and 35% in patients with pT2 and pT3 disease, respectively. The most common locations for PSMs during RARP are posterolateral and apical, but location and number do not seem to affect survival. However, an extensive PSM does seem to affect the prognosis adversely. Various technical modifications and tailoring the nerve sparing according to the disease severity have been shown to improve cancer control during RARP. The major technical modifications are listed in Fig. 2 and are discussed later.
Apical Dissection
Meticulous dissection of the prostatic apex is one of the most challenging steps of RP, for multiple reasons. First, the apex is in a relatively inaccessible location, deep beneath the pubic arch and surrounded with vital structures such as the dorsal venous complex (DVC), converging erectile neurovascular bundles, rectum, and urethral sphincter. Second, the apex lacks the distinct prostatic capsule and periprostatic tissue that surrounds the posterolateral prostate, making the accurate planes of dissection in this area difficult to find. Third, the anatomy of the apex is highly variable from individual to individual, with some glands harboring a distal beak of apical tissue protruding posterior to the urethra (also known as a posterior apical notch). This hidden posterior extension might be violated during surgery, especially if the dissection is carried out in a plane perpendicular to the longitudinal axis of the urethra.
Therefore, to optimize the cancer control (as well as urinary and potency outcomes), surgeons have sought ways to optimally dissect the apical tissue. For example, to prevent the DVC or puboprostatic ligaments from obstructing the view, Tewari and colleagues used a 30° upward-looking lens combined with cephalad retraction of the prostate (by an assistant) to approach the transition of the apex into the membranous urethra from the posterior undersurface of the prostate rather than the conventional anterior approach. This novel retroapical technique decreased the investigators’ PSM rates from 4.4% to 1.4%. Other proposed modifications include upfront cold transection of the DVC facilitated by increased pneumoperitoneum and its subsequent ligation.
Degree of Nerve Sparing Versus Cancer Control
Before deciding how wide to dissect the neurovascular bundles, the surgeon must take into consideration the clinical patient data, including prostate biopsy findings, prostate-specific antigen levels, digital rectal examination findings, patient age, preoperative sexual function, and patient expectations, because different levels of nerve sparing can be considered based on these factors, and accordingly, different planes of dissection can be entered. Nerve sparing is not an all or none phenomenon, as it was believed to be.
Tewari and colleagues suggested using the periprostatic veins as an anatomic landmark to differentiate among the various fascial compartments. Depending on the preoperative clinical characteristics and how the extent of the tumor at base is appreciated, the surgeon may choose to carry out the dissection in 1 of the 3 periprostatic anatomic planes: in an intrafascial plane (complete nerve sparing as ascertained by the view of glistening prostate), an interfascial plane (partial nerve sparing confirmed by a whitish coloration of the prostate), or an extrafascial plane (non–nerve sparing determined by fatty tissue seen on the prostate). These investigators showed a decline in PSM rate from 2.1% to 1% by adoption of these visual cues, despite an increase in risk categorization of the patients operated.
Intraoperative Frozen Section Analysis
Techniques for extracting prostate intraoperatively during RARP have recently been described by our group and Beyer and colleagues These techniques are aimed at increasing the certainty of adequate excision of the tumor by allowing performance of real-time bimanual examination and frozen section histopathology of the excised prostate specimen, especially in patients with aggressive high-risk disease.
In our technique a GelPOINT device (Applied Medical, Rancho Santa Margarita, CA) is used, which allows for rapid specimen extraction without compromising the pneumoperitoneum. The GelPOINT access port is inserted in the periumbilical region through a 4-cm to 5-cm vertical incision. The GelSeal cap, prepared with a 12-mm camera port and a 10-mm assistant port preplaced through it, is secured on top of the access port. Cruciate stab incisions around the 10-mm port on the GelSeal cap are made to facilitate the retrieval of the specimen. Other ports are placed and the patient is put in a 30° Trendelenberg, as previously described. After excision of the prostate, the specimen is retrieved through the stab incision in the GelSeal cap without dedocking the robot, and a bimanual examination is performed on table by the surgeon. Frozen section biopsies are obtained from areas suspicious for PSM and after being carefully marked for anatomic orientation are sent for pathology. Biopsies positive or suspicious for cancer result in more tissue being removed from the corresponding pelvic bed region, which is labeled and sent for permanent sections. Beyer and colleagues, developing on their technique of NeuroSAFE for ORP, also recently described a similar technique for RARP. In contrast with our technique, in the NeuroSAFE technique, the prostate is systematically sectioned in a circumferential manner (rather than targeted biopsies as we do) and the sections are sent for frozen section analysis. Both these studies showed a dramatic reduction in PSMs by performing intraoperative frozen biopsies, without an increase in the operative time or blood loss. Beyer and colleagues found that the overall PSM rate decreased from 24% to 16% ( P = .003) by adopting the NeuroSAFE technique, and we found that the PSM rates (in patients with pT3 disease) decreased from 43% to 17% ( P = .05). Beyer and colleagues also showed that in addition to decreasing the PSM rates, the NeuroSAFE technique also improved the nerve sparing rates in the setting of both organ-confined and locally advanced disease.
Technical advancements in urinary continence
Oncologic outcomes achieved with RARP and ORP have been excellent and equivalent, and hence, the focus of innovation has increasingly been on the preservation of quality of life (QOL). Urinary control after RP has the greatest impact on a patient’s QOL and accordingly, maintaining optimal urinary function after RP takes precedence among outcomes, given ideal control of cancer. As a result, several surgical modifications in technique have been attempted to achieve early return and improve overall continence rates.
Fig. 3 summarizes the various technical modifications and advances that have been made in this regard, and their impact on continence outcomes. Many of these modifications were developed in the ORP model, but because the surgical principles underlying continence preservation are consistent irrespective of the approach, these modifications were readily adapted for robotic surgery. These modifications are detailed later.
Bladder Neck Preservation
As understanding of the continence anatomy and mechanism evolved, the usefulness of bladder neck preservation was shown. Gaker and Steel and Deliveliotis and colleagues both reported that precise dissection of the prostatovesical junction and preservation of the circular muscle fibers of the bladder neck lead to early return of continence, although overall continence rates remained unchanged. Similar results have been reported by other groups as well.
Periurethral Suspension
Many investigators have shown the usefulness of periurethral suspension after DVC ligation. Different approaches have been described. Patel and colleagues, using their technique of DVC suspension, showed earlier return of continence as well as higher continence rates at 3 months. Similarly, Campenni and colleagues, using their technique of pubourethral suspension, Noguchi and colleagues, using their approach of vesicourethral anastomosis suspension, and Jorion, using their technique of fascial sling suspension, also reported significantly improvement in continence outcomes. However, the latter modification also increased the risk of urinary retention. We do not perform this step routinely, because we have noted no additional improvement in urinary control by performing periurethral suspension in addition to our routine nerve sparing VIP technique.
Puboprostatic Ligament Sparing
It has been hypothesized that preservation of the puboprostatic fibromuscular tissue would provide anterior support to the urethra, leading to better urinary control. Studies by Poore and colleagues and Avant and colleagues reported that preservation of pupoprostatic ligaments facilitated an earlier median return to continence when compared with standard ORP. On the contrary, Deliveliotis and colleagues showed that there was no short-term continence benefit in adding pupoprostatic ligaments preservation to bladder neck sparing. This concept has been translated into Retzius-sparing RARP by Galfano and colleagues and Rha and colleagues Conventional RARP technique for bladder neck dissection, nerve sparing, and apical dissection use an anterior approach, but these investigators have suggested a posterior approach without the need for dropping down the bladder. Galfano and colleagues claimed that this technique showed better outcomes in early continence rate, compared with the published data. However, this technique is still in its infancy, and there is lack of high-level evidence to support the superiority of this technique over the conventional approaches.
Periurethral Reconstruction Techniques
Great interest has been paid to periurethral reconstructive techniques: both posterior musculofascial plate and anterior puboprostatic collar repair. The posterior repair technique, using a 2-stitch posterior rhabdosphincter reconstruction before urethrovesical anastomosis, was first proposed by Klein and Rocco and colleagues and reported dramatic success in improving early continence in both ORP and LRP settings. Continence rates at 1 month improved from 30% to 79% for ORP and from 32% to 84% for LRP. These results have been replicated in the setting of RARP by Nguyen and colleagues, who showed that the continence rates improved from 17% to 56% at 6 weeks. Coelho and colleagues also reported early return of continence in patients undergoing posterior reconstruction during RARP (42.7% vs 51.6% at 4 weeks), but no difference in continence rates was observed at 3 and 6 months. Tewari and colleagues developed a technique for preservation of the anterior puboprostatic collar, with 1-week and 6-week continence rates of 29% and 62%, respectively; subsequently, a complete vesicourethral repair technique was developed, yielding 1-week and 6-week continence rates of 38% and 83%. Our own experience, in a randomized control trial setting, showed that reconstruction of periprostatic tissue (both anterior and posterior) provided no added benefit in early return to continence (80% vs 74% at 30 days; P >.1). The lack of improvement noted in the patients undergoing complete periurethral repair was probably because of the excellent continence outcomes already achieved by the patients in the control group secondary to precise nerve sparing, urethral length preservation, and bladder neck sparing. Despite this finding, we do continue to perform a posterior musculofascial repair before ultraviolet anastomosis.
Preservation of Urethral Length
Multiple studies have reported the importance of preserving membranous urethral length for optimal urinary continence. Coakley and colleagues and Nguyen and colleagues, using preoperative magnetic resonance imaging, reported that the membranous urethral length was directly related with continence outcomes after RP. However, the challenge lies in precisely identifying the junction between the prostatic apex and the proximal membranous urethra. The improved visualization of the robotic interface is implicitly beneficial in pursuit of this goal. van Randenborgh and colleagues suggested a technique of craniodorsal retraction of prostate for maximal preservation of urethral length. They reported significant improvement in continence (89% vs 76%; P <.05).
Creating a Watertight Anastomosis
Urine extravasation secondary to poor vesicourethral anastomosis has been shown to lead to local inflammation followed by fibrosis and scarring of the vesicourethral junction. Van Velthoven described a simple, running, laparoscopic technique for accomplishing a watertight vesicourethral anastomosis. This technique is easily transferrable and reproducible in the robotic environment and has been described by our group in detail previously.
Locoregional Pelvic Hypothermia
Controlled hypothermia is a well-established technique that has been used to limit the inflammatory cascade common to all surgical procedures. Finley and colleagues were the first to use, and show the benefits of, regional cooling during RARP. These investigators used an endorectal cooling balloon system, which was continuously irrigated with ice-cold saline at 4°C to maintain effective regional hypothermia throughout the procedure. With this technical modification, the investigators noted a significant decrease in the time to continence (median 39 days vs median 59 days; P = .002) as well as improved overall continence rates at 3 months (86.8% vs 68.6%). This technique might aid in improving the potency outcomes as well, because the underlying physiologic principles used are consistent with the athermal technique of cavernosal nerve sparing (see later discussion).
Barbed Suture
Sammon and colleagues performed a randomized control trial showing the usefulness of barbed sutures in decreasing the time for urethrovesical anastomosis (26.8% reduction) and posterior reconstruction (23.3% reduction). V-Loc (Covidien, Mansfield, MA, USA) barbed sutures were used, and knots were not required because of the autolocking properties of the suture. These investigators found no difference in leaks, bladder neck contractures, patient symptoms, or other outcome measures. Subsequently, it has been shown to be a cost-effective approach as well.
Suprapubic Catheter
Traditionally with ORP, the bladder had been drained via urethral catheter for a finite period (2–3 weeks) to maintain urethral patency. Despite this precaution, bladder neck contracture rates ranged from 5% to 32%. With the advent of running anastomosis and the improved visualization of mucosal suturing offered by the robotic platform, postoperative bladder neck contracture rates were reduced to 0% to 3%, questioning the role of urethral catheter in urethral patency after RARP. Further, the desire by both patient and surgeon for early catheter removal, or perhaps to obviate urethral stenting altogether, led us to introduce the suprapubic catheter as an alternative to the urethral catheter. We found that the continence and stricture rates were similar between this group and historical controls, with significant reduction in catheter-related discomfort postoperatively. Results from other groups have been mixed, with some mirroring our results, whereas others have reported no benefit. In a subsequent study, we showed that the use of a suprapubic catheter (instead of the urethral catheter) was also associated with an early return of urinary continence. Tewari and colleagues looked at a custom suprapubic catheter with a small bladder neck anastomotic splint, which could be retracted. This pilot study also reported earlier return of continence and decreased patient discomfort.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





