Effects of Surgery and Therapeutic Procedures
Endoscopic Thermal Injury
Endoscopic resection of colorectal polyps is currently a standard practice. In general, the resection margin passes through the submucosa. Less than 1% of patients perforate following the procedure (615). Perforations could result from the surgical resection of the colonic wall or from thermal injury. The postendoscopic resection sites show a range of mucosal changes including ulceration. Submucosal changes include inflammation, granulation tissue, fibrosis, and vascular proliferations. If changes are present in the muscularis propria, they may have a “skip” appearance. These consist of patchy muscular depletion or necrosis in the inner muscular layer with or without accompanying fibrosis. Ink may also be seen (615).
Diversion Colitis
The term diversion colitis refers to the inflammation that occurs in the defunctionalized intestinal segment following diversion of the fecal stream. The changes may remain asymptomatic or give rise to rectal bleeding or discharge (616,617). Its importance lies in the inability to differentiate it from other types of proctitis, such as ulcerative colitis. The lesion completely resolves following restoration of the continuity of the fecal stream.
The pathophysiology of the changes are thought to relate to a decrease in mucosal nutrition since short-chain fatty acids that derive from the bacterial fermentation of starch and proteins are the main metabolic fuels for colonocytes, especially distally (618). A change in the bacterial flora in the defunctionalized segment may also lead to the inflammation.
Patients with diversion colitis present with continuing GI symptoms, including constipation or diarrhea with mucoid or bloody discharge and crampy abdominal pain. Endoscopically, the bowel may show erythema; petechial hemorrhages; mucosal friability; mucosal nodularity, sometimes surrounded by aphthous ulcers; nonspecific colitis; and inspissated mucus (619). Patients may also present with the underlying disorder for which the original colonic surgery and diversion were performed, such as IBD.
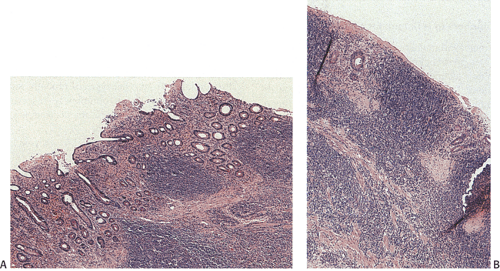
Inflammation develops in up to 72% of patients (Fig. 13.177). Biopsies taken from the distal diverted intestine show relatively nonspecific changes, including aphthous ulcers, focal crypt abscesses, surface exudates, surface epithelial cell degeneration, and prominent follicular hyperplasia. It is the lymphoid hyperplasia that produces the fine mucosal nodularity. Many of the mucosal lymphoid follicles have overlying small, punctate erosions forming classic aphthous ulcers. With time, the mucosal inflammation becomes more extensive, leading to the development of ulcers and inflammatory pseudopolyps. Inflammation occurs diffusely throughout the lamina propria and is mainly chronic in nature, but it may include some neutrophils with consequent cryptitis and crypt abscess formation. Subsequently, muciphages may become prominent in the lower half of the lamina propria.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree