Dynamic Graciloplasty
Cornelius Baeten
S. Breukink
Introduction
Continence is a subtle coordinated action of several factors including peristalsis, stool consistency, rectal capacity, anorectal sensibility, pelvic floor muscles, central neural intactness, and an intact sphincter. After the sphincter is damaged the quality of the other factors will determine patients’ continence. In the presence of fecal incontinence, it is mandatory to investigate all these variables. The best methods to evaluate the sphincter function are endosonography and anal manometry in order to obtain insight into the anatomy and contractility of the internal and external sphincter. One of the last resorts for incontinent patients is the dynamic graciloplasty. Graciloplasty is the transposition of the gracilis muscle from the upper leg to encircle the anus (1). This muscle transposition seems an ideal solution as the anus is reinforced with a fresh muscle. This muscle seems to have no other function in the human body but auxiliary to endorotation and adduction of the leg, and can be harvested without affecting performance in the lower limb.
The procedure is termed dynamic graciloplasty as the muscle is stimulated and therefore able to contract longer without any fatigue. A normal skeletal muscle is not capable for long-term contraction; the muscle will fatigue and within a few minutes it is not capable to recontract. This means that a normal transposition can never give a functional replacement of the original anal sphincters.
Anatomy and Physiology
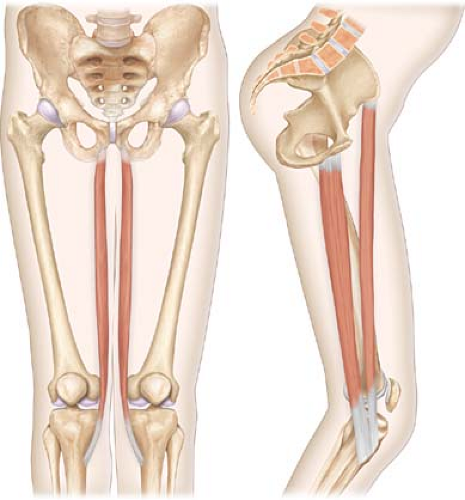
The gracilis muscle is the most superficial muscle in the medial aspect of the upper leg (Fig. 12.1). Its vascular supply consists of several arteries. The main artery, the vein, and the gracilis nerve enter the muscle at 8 cm from the origin of the gracilis very reliably. The main artery derives from the arteria femoris profunda. The number of peripheral arteries vary among people ranging from zero to five, and even shows variability in the same patient between sides. To harvest and rotate the muscles all of
the peripheral arteries must be divided. In over 95% of patients the vascular bed inside the muscle will supply even the most distal part of the gracilis muscle (2).
the peripheral arteries must be divided. In over 95% of patients the vascular bed inside the muscle will supply even the most distal part of the gracilis muscle (2).
The veins always accompany the arteries. The obturator nerve supplies the gracilis nerve. The origin of the muscle is the wide attachment at the pubic bone. The distal tendon of the gracilis muscle joins with the tendons of the sartorius and semitendinosus to form the “pes anserinus” (goose’s foot). The part of the gracilis distally from the neurovascular bundle is available for transposition around the anus. At the top the gracilis is wider, and while running downward it tapers to the distal tendon. The form and location of the gracilis provide the most ideal muscle to construct a sphincter.
Microscopically the fiber pattern of most skeletal muscles is very similar to the muscle fibers of the gracilis. The majority of the fibers consist of type II fibers which are forceful, but fatigue-prone, capable of a short-term contraction hence unsuitable for sphincter function.
The first dynamic graciloplasty was described in 1988 (3). The muscle was stimulated with electrical pulses, inducing a change in fiber pattern of the muscle. Type 1 fibers were gradually replaced by type 2 fibers, which are less force-full but not loosely fatigable. The dynamic graciloplasty was capable of long-term contraction of the gracilis muscle (4,5), and it resembled the fiber pattern of the original anal sphincter (6). Contracting the gracilis muscle voluntarily was no longer necessary as the implanted stimulator forced the muscle to a continuous contraction. By switching off the stimulator, we allow muscle relaxation followed by evacuation.
The dynamic graciloplasty should only be utilized after most other therapies have proven to be unsuitable or have failed. It can be the last step before a consideration of permanent colostomy.
The patient has to be informed about all pros and cons of the operation. The choice for a left or a right graciloplasty depends on the condition of the muscles, innervations, vascularization, or surgeon’s preference. Patient hand dominance has no influence on choice of side.
The patient is positioned with the legs in stirrups to have good access to the upper leg, the perineum, and the lower abdomen. The skin is prepared and the patient receives systemic antibiotics.
Dynamic graciloplasty is always performed under general anesthesia. Spinal or epidural anesthesia is possible but can be psychologically demanding on the awake patient.
The operation starts with an incision in the median aspect of the upper leg. The subcutis is divided and the first muscle visible is the gracilis muscle. The gracilis is not encapsulated by the Fascia Lata. The dorsal side provides a safe entrance to free the gracilis muscle. With index finger the gracilis can now be encircled and drawn from its bed. In doing this, several peripheral arteries are stretched (Fig. 12.2).
The small arteries are divided by ligation of both ends or by coagulation. The gracilis should be freed first about halfway the upper leg. The sartorius muscle partially covers the gracilis and should not be mistaken for the gracilis muscle. The gracilis is now freed up to its distal tendon. The gracilis tendon can be divided some centimeters proximal from its insertion. The gracilis now lies free in the upper leg and can be drawn to medial with a clamp on the distal tendon. The proximal part of the muscle can now be freed up to the neurovascular bundle that invariably can be found at the lateral side, 8 cm from the origo. The neurovascular bundle must be preserved. Damaging the nerve, the artery and the vein will necrotize the muscle. The medial aspect of the proximal part of the gracilis can be freed from the subcutaneous tissue. The only structure that can be found here are the small arteries to the dermis, which can be coagulated. The gracilis muscle is now distally free (only attached to its origin and its neurovascular bundle); while preparing for the next part of the operation, it can be protected by tucking it in the perianal subcutaneous pocket.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree