Superficial position in the medial aspect of the upper thigh
Main neurovascular bundle in the upper part of the muscle which can allow to free its body for all the entire length as far as the insertion of its tendon to the tibial plate
Proximal attachment to the pubic bone far from the insertion of the main neurovascular bundle
No functional problem after detachment from the leg being an auxiliary muscle for adduction, flexion, and extrarotation of the hip and knee
16.2 Current Indications for DGP
In the treatment of selected cases of end-stage fecal incontinence, DGP can be offered as an option to those patients in whom a major defect of the external sphincter is the main reason of the problem. Usually these lesions are of traumatic or iatrogenic origin, and sphincter’s defect involves half or more of its circumference preventing the possibility of a direct muscular and anal repair. ABS is not indicated in the presence of a massive tissue defect (Fig. 16.1). Patients with anorectal agenesis submitted to pull-through procedure in whom electromyographic mapping or perineal sonography demonstrates the absence of anal sphincters are also possible candidates to DGP. In patients strongly determinate to avoid a terminal abdominal stoma after APE, the so-called total anorectal reconstruction (TAR) can be an option. The operation consists in performing, after an APE, a perineal colostomy and encircling it with a neosphincter represented by a stimulated gracilis muscle. In end-stage fecal incontinence, a complete workup of the anorectal function of the patient to rule out the extent and type of damage should have been primarily done to evaluate possible conservative or alternative surgical treatments like sphincteroplasty, SNS, and ABS (Table 16.2). Contraindications to DGP are reported in Table 16.3. As regards TAR, the almost unique indication derives from the desire of the patients to avoid a terminal abdominal stoma. Advances in surgical techniques and increasing adoption of neoadjuvant treatment have determined in the last years a steep increase of sphincter-sparing procedures with subsequent decreasing number of patients with permanent abdominal colostomy [30]. Therefore, the indications for offering a TAR procedure are nowadays quite limited (Table 16.4). As regards the approach to patients with rectal cancer, some authors [31, 32] sustain that it is correct to offer the option of TAR only after an adequate period of follow-up (at least 2 years) to minimize the risk of a recurrence and to allow selection of patients really determine to avoid an abdominal stoma. Indeed, in most of the reported series, TAR was performed as primary reconstruction. Deferred reconstruction is feasible but with high morbidity [33]. The operation should be reserved to patients with long life expectancy. Patients with advanced age, with metastatic disease, or very advanced rectal cancer; those who do not respond to preoperative chemoradiation; and those with no curative resection should not be considered for TAR. Patients must have complete information of the operation with the possible complications and rate of failure. Functional results are not always good. They must be advised that a fairly acceptable outcome in the long term can be obtained in 50 % of the cases and that defecation will not be the same as before the surgery. Quite often they will experience defecatory difficulties requiring enemas to empty the neorectum. The surgeon must evaluate the manual dexterity of the patients to use the magnet or handheld telemetry equipment which controls the stimulator. Of high relevance is the meeting with one or more patients of similar age and sex who had undergone the procedure especially TAR.
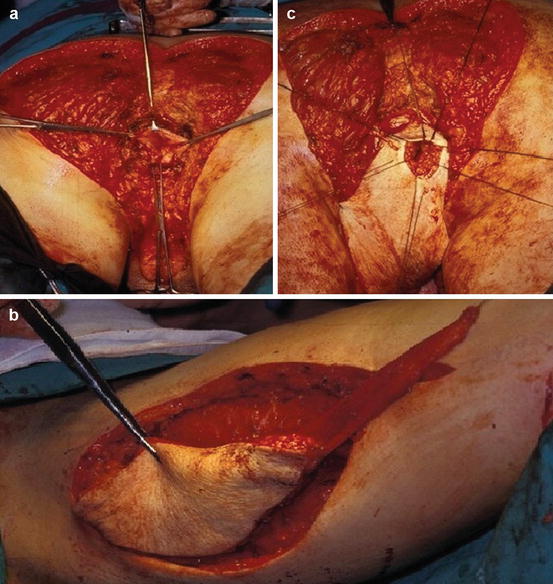
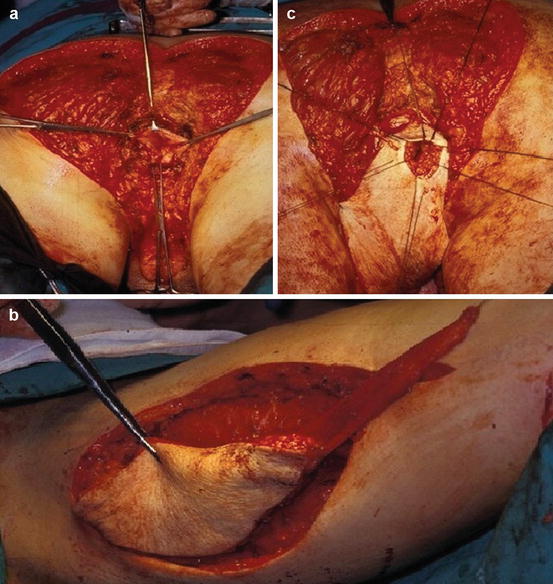
Fig. 16.1
(a) Wide perineal and anal sphincter excision for destructive Verneuil disease. (b) Preparation of myocutaneous gracilis flap. (c) Transposition of the flap to the perineum with the gracilis muscle encircling in γ fashion the neoanus; anastomosis between the rectum and the skin of the flap. Dynamization of the muscle was performed after 6 months
Table 16.2
Examinations for evaluation of fecal incontinence
Colonoscopy/proctoscopy | Anorectal sensitivity tests |
Endoanal sonography | Anal reflexes examination |
Anal manometry | Electromyography of the anal sphincter with PNTML (pudendal nerve terminal motor latency) |
Defecography |
Table 16.3
Contraindications to DGP
Intussusception | Enterocele |
Rectocele | Rectal prolapse |
Constipation | Perianal sepsis or Crohn’s disease |
Causes of potentially damaged gracilis muscle (sclerosis, myopathic diseases) | Cardiac pacemaker (relative) |
Table 16.4
Possible indications for APE + TAR
T2–T3 very low rectal cancer (2–3 cm from a.m.) not suitable for an intersphincteric excision and coloanal anastomosis (history of episodes of fecal incontinence and/or partial response to preoperative chemoradiation) |
Anal cancer partially responsive to chemoradiotherapy |
Extensive damage of anal structures for advanced fibrosis and stenosis after radiochemotherapy for anal cancer |
Complete traumatic or infective destruction of anorectal structures (car accident, gun wounds, sex abuse, Verneuil disease, etc.) |
16.3 Technique of Dynamic Graciloplasty: General Aspects
As regards isolation of the gracilis muscle, the technique has been well standardized after the works of Pickrell, and it is the same either in the presence of intact rectum or in the case of TAR after APE [4]. Conversely, other technical aspects related to timing of graciloplasty after APE as well as the timing and method of electrical stimulation have been and in part are still controversial issues. The different surgical approaches are summarized in Table 16.5.
Table 16.5
Reported surgical approaches to DGP
Graciloplasty for fecal incontinence with intact rectum | Synchronous vs. deferred insertion of stimulating electrodes | With or without protective stoma |
Immediate vs. deferred stimulation | ||
Neuronal vs. muscular stimulation | ||
APE with synchronous perineal colostomy | Synchronous mono- or bilateral graciloplasty | With or without protective stoma |
Synchronous or deferred insertion of the electrodes | ||
Neuronal vs. muscular stimulation | ||
Immediate vs. deferred stimulation | ||
Deferred perineal colostomy after late refusal of terminal abdominal stoma | Synchronous or deferred mono- or bilateral graciloplasty | With or without protective stoma |
Synchronous or deferred insertion of electrodes | ||
Neuronal vs. muscular stimulation | ||
Immediate vs. deferred stimulation |
16.4 Dynamic Graciloplasty in Fecal Incontinence
The patient is placed on the operating table in the modified Lloyd-Davis position with the interested leg abducted and extended. This leg will be, if necessary, adducted during the operation to favor the encirclement of the anorectum or neorectum by the gracilis. A single longitudinal incision is made on the medial aspect of the thigh following a line going from the medial femoral condyle to the inferior pubic ramus. Alternative access to the muscle can be obtained through a series of small incisions following the same line. Taking care not to damage the main saphenous vein, the muscle is easily identified being the most superficial muscle in that area, sharply dissected and gently encircled with a finger (Fig. 16.2a). Small feeding vessels are identified, tied, and cut to reach the tendon in its distal part, remembering that, at this level, the sartorius muscle covers the tendon and it must be separated. The tendon is followed as far as its insertion in the tibial tuberosity and cut 4–5 cm distal to the muscular body. The gracilis is proximally isolated as far as its main neurovascular bundle containing arteries arising from the profunda femoris and nerve from the obturator nerve. The main vascular pedicle and nerve enters in the lateral aspect of the muscle at the junction of the proximal with the distal two thirds of it at about 7–8 cm from the origin of the muscle at the pubic bone and emerging under the abductor longus muscle. The pedicle can be checked with the help of a disposable nerve stimulator (Fig. 16.2b). Some authors have suggested to clear the vascular pedicle from areolar tissue with careful dissection and mobilize the muscle as far as its origin in the pubis [18]. This maneuver would help in obtaining a complete encirclement of the anal canal by the body of the muscle and in identifying the main nerve of the gracilis proximal to the main vascular bundle. This can also allow the positioning of the stimulating electrode directly on the nerve that lies on the abductor magnus muscle. Since preservation of the main neurovascular bundle is the mandatory step of the operation, most of the authors do not isolate the main nerve to the gracilis muscle for the risk of damaging it, preferring to place the electrodes distally to the nerve entrance (Fig. 16.2c) [34]. The muscle with intact neurovascular bundle is repositioned in the thigh.
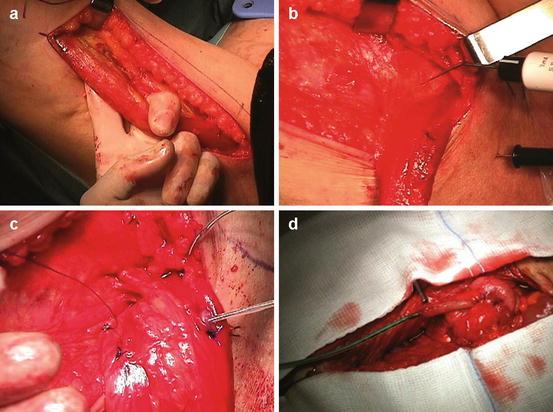
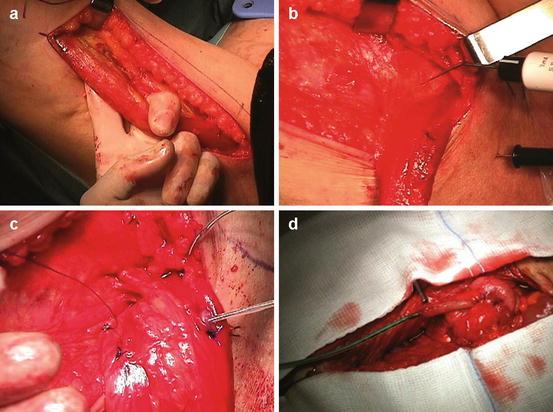
Fig. 16.2
(a) Isolation of the gracilis muscle. (b) Identification of the neurovascular bundle with electronic stimulator. (c) Final position of the electrodes for neuromuscular stimulation. (d) Preparation of Malone-type appendicostomy for antegrade continence enema
16.4.1 Preparation of Native Anorectum in Fecal Incontinence
Two curvilinear incisions 3–4 cm long are made lateral or anterior/posterior to the anus. A subcutaneous tunnel around the anal canal, external to the sphincters, is created. It must allow at least the passage of two to three fingers for easy accommodation of the gracilis muscle to avoid its entrapment when transposed. A communication is created between the perineum and the wound in the thigh with sharp dissection dividing the strong Scarpa’s fascia. Also this tunnel must allow the passage of, at least, three fingers.
16.5 Graciloplasty and TAR
Graciloplasty, as part of immediate TAR, is done much the same as for fecal incontinence. It is done under general anesthesia being carried out after TME abdominoperineal resection with perineal colostomy. Sometimes two gracilis muscles have been transposed [33, 35]; however, in most experiences, only one gracilis has been isolated and transposed [31, 36]. The operation is made in the classic Lloyd-Davis position as for APE with access to both thighs. The abdominal operation can be performed laparoscopically and it is slightly different from a standard APE. In fact to allow the descending colon to reach the perineum, it is necessary to mobilize the splenic flexure. A temporary loop ileostomy is prepared in the lower right abdominal quadrant. In the perineal phase, after excision of the anorectum and having encountered the abdominal dissection, the anorectum and sigmoid colon are delivered outside the perineal wound as in a pull-through maneuver. The descending colon is transected with a stapler in a well-vascularized area a few cm outside the perineum and the specimen removed. Some long stitches are positioned in the proximal stump to avoid its sliding in the pelvic cavity. Alternatively, a longer proximal stump 10–15 cm is left to protrude outside the perineum. The preparation of the gracilis is performed in the same manner as described above. A subcutaneous tunnel is created between the incision of the thigh and perineal wound.
16.6 Positioning of the Gracilis Muscle and Dynamization
Using a long strong clamp passed from the perineal wound to the incision in the thigh, the free tendon is grasped and the muscle is transposed in the perineum taking care not to twist it. Different configurations of looping the anus with the muscle can be adopted to use as much as possible muscular tissue rather than tendon (Fig. 16.3). Gamma or epsilon loop is created when the muscular part is long. Alpha loop is preferred in case of short muscular part or in double transposition. Rosen suggested a split technique in which the tendon is brought through the muscle belly itself to shorten the way around the anal canal [36]. After deciding the configuration of the loop, the muscle is repositioned in the thigh to allow easier placements of the electrodes and to pass the fixing stitches in the periosteum of the homolateral or contralateral pubic bone (ischium). During this maneuver, if patients are under general anesthesia, no muscle relaxant must be used. Electrodes (Platinum-Iridium, mod.435045/mod.435055, Medtronic Inc., USA) must be placed to allow maximum contact with muscular fibers and nerves. The first electrode (anode), with a special designed needle, is passed through the body of the muscle orthogonal to its main axis a few cm distal to the nerve entrance. The other electrode (cathode) is positioned close to the entry of the nerve in the muscle with the help of an auxiliary electrode connected to the needle used for insertion. Stimulating this electrode and the needle, it will be easy to find out the best place for insertion that is where the muscle contracts at the lowest voltage. Both electrodes are fixed to the epimysium. In the case of double graciloplasty, the electrodes (cathodes) are positioned close to the nerve entrance of both muscles. The dynamized muscle(s) is/are now repositioned around the anus according to the best configuration, while the tendon(s) is/are anchored by the stitches placed in the periosteum of the ischial tuberosity(ies). The electrodes are passed subcutaneously from the thigh(s) to a pocket prepared in the lower abdomen and connected to a pulse generator (InterStim mod.3023, Medtronic Inc., 710 Medtronic Parkway N.E. Minneapolis – MN 55432 – USA) placed and fixed to the muscular fascia. The wounds are closed. Some authors create a temporary loop ileostomy in the lower right abdominal quadrant also in the procedure for fecal incontinence [23]. In TAR the colonic stump (neoanus) is opened and sutured to the perineal skin. When a longer stump has been left protruding from the perineum, this can be left in situ for 1 week as far as it has adhered to the perineal skin. At that moment, the excess of the colon will be resected and the coloperineal anastomosis performed.