CHAPTER 23 Diverticula of the Pharynx, Esophagus, Stomach, and Small Intestine
ZENKER’S DIVERTICULUM
Cause and Pathogenesis
Zenker’s diverticula are acquired. They develop when abnormally high pressures occurring during swallowing lead to protrusion of mucosa through an area of anatomic weakness in the pharynx known as Killian’s triangle. High pressures are generated when the opening of the upper esophageal sphincter (UES) is impaired. In patients with Zenker’s diverticula, several pathophysiologic changes have been documented in the cricopharyngeus. These changes lead to a reduction in compliance and to decreased opening of the UES.1 Killian’s triangle is located where the transverse fibers of the cricopharyngeal sphincter intersect with the oblique fibers of the inferior pharyngeal constrictor muscle. The size of this area of weakness varies among individuals. Relatively large defects may predispose to the development of Zenker’s diverticula.2
Diverticula similar in appearance to Zenker’s diverticula have been reported as a complication of anterior cervical spine surgery.3,4
Clinical Features and Diagnosis
The prevalence of Zenker’s diverticula has been estimated to be between 0.1% and 0.01%. Patients generally present in the seventh or eighth decade of life. Twice as many men as women develop Zenker’s diverticula.1,5 Common presenting symptoms are listed in Table 23-1. Patients with small diverticula may be asymptomatic.
Table 23-1 Presenting Symptoms in Patients with a Zenker’s Diverticulum
Squamous cell cancer may develop in Zenker’s diverticula. The incidence has been estimated to be from 0.4% to 1.5%.1,6,7 If myotomy without diverticulectomy is planned, it is prudent to inspect the lining of the diverticulum carefully for any evidence of cancer.
Bleeding may occur from ulcerated Zenker’s diverticula. Aspiration of retained food contents may complicate induction of anesthesia.8 Medications may become lodged in Zenker’s diverticula. Corrosive medications may cause ulceration. Unpredictable absorption of tablets or capsules may also lead to clinical problems.9 Accumulation of radioactive iodine tracer in a Zenker’s diverticulum has been reported to lead to an erroneous diagnosis of metastatic thyroid cancer.10 Videocapsules may also become lodged in Zenker’s diverticula and should be delivered into the stomach with a fiberoptic endoscope when such studies are required.11,12
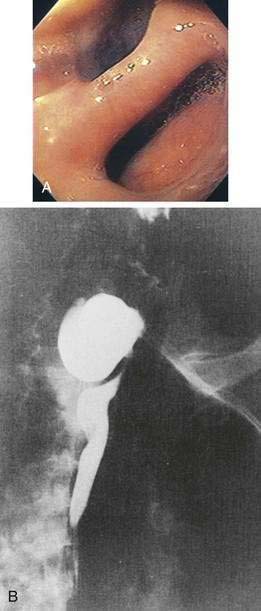
Intubation of the trachea or the esophagus may be complicated by the presence of a Zenker’s diverticulum. A large diverticulum displaces the lumen of the esophagus. The tip of the intubation instrument is directed preferentially into the diverticulum. At endoscopy, it may be difficult to distinguish the lumen of the diverticulum from the true lumen of the esophagus (Fig. 23-1A). Endotracheal intubation, placement of a nasogastric tube, and intubation of the esophagus for upper endoscopy, endoscopic retrograde cholangiopancreatography, or transesophageal echocardiography may be difficult. Perforation can occur. Intubation in patients with Zenker’s diverticula should be done under direct vision. When a large Zenker’s diverticulum causes marked anatomic distortion or when intubation with a side-viewing endoscope is required, direct intubation is not prudent. In such cases, a forward-viewing endoscope can be used to pass a soft-tipped guidewire into the esophageal lumen. The guidewire is then back-loaded into the endoscope and the endoscope is advanced into the esophagus over the guidewire. An alternative technique consists of passing a forward-viewing endoscope loaded with an overtube. Once the endoscope has been passed into the esophagus, the overtube is advanced, the forward-viewing endoscope is withdrawn, and the side-viewing or ultrasound endoscope is passed through the overtube.13
Zenker’s diverticulum can be suspected from a careful history (see Table 23-1). Barium swallow is the most useful diagnostic study. The radiologist should be alerted in advance, so that proper views are taken (see Fig. 23-1B). Small diverticula may be seen only transiently. Barium swallow in the lateral view using video fluoroscopy is helpful for detecting small diverticula. The opening of a large Zenker’s diverticulum often becomes aligned with the axis of the esophagus. Oral contrast will preferentially fill the diverticulum and will empty slowly. Large diverticula are therefore often obvious, even on delayed images. During endoscopy, Zenker’s diverticulum should be suspected if, on entering the pharynx, the upper esophageal sphincter cannot be located. In such cases, the endoscopy should be stopped and the patient should be sent for a barium study.
Treatment and Prognosis
Patients with small asymptomatic or minimally symptomatic diverticula can be followed, because progressive enlargement is uncommon.2 Patients with large and symptomatic Zenker’s diverticula should be offered treatment.
Zenker’s diverticula may be treated by open surgical procedures or by transoral endoscopic techniques with rigid or flexible fiberoptic instruments. Open surgery for Zenker’s diverticula can be performed as an outpatient procedure.14 An open surgical approach is the safest alternative for patients with large (>5 cm) diverticula that extend into the thorax.15 Damage to mediastinal structures is best avoided by optimal exposure. Large diverticula can be resected, inverted, or suspended (diverticulopexy). Resection of small diverticula is not required. UES myotomy should always be part of the procedure. If diverticula are resected without myotomy, there is an increased risk of postoperative leaks and an increased frequency of recurrence.16,17 Complications of open surgery include leaks with mediastinitis, esophagocutaneous fistula, and vocal cord paralysis from recurrent laryngeal nerve injury.
Endoscopic treatment has become the predominant technique for the management of Zenker’s diverticula since the introduction of stapling for myotomy in 1993. Compared with open surgical approaches, endoscopic approaches are associated with lower complication rates, shorter anesthesia times, and shorter hospital stays.7
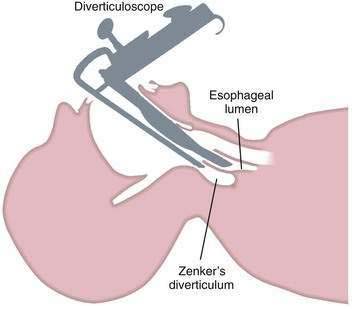
Endoscopic techniques are suitable for patients with medium-sized diverticula (2 to 5 cm). Specially designed rigid diverticuloscopes (e.g., Weerda, van Overbeek) and conventional flexible fiberoptic endoscopes have been used. The diverticuloscope is used to provide optimal visualization of the lumen of the esophagus and diverticulum and the septum between them (Fig. 23-2). This septum is comprised of the posterior wall of the esophagus and the anterior wall of the diverticulum, and includes the UES. The muscular layers of this septum are incised, resulting in ablation of the UES and restoration of a single lumen. The incision can be performed by a number of techniques. With a rigid diverticuloscope, CO2 laser and surgical staplers have been used. Stapling has become the predominant technique since it was reported to be safer and more effective than CO2 laser.7,18 With CO2 laser, fusion of the cut edges of the incision is relied on to prevent leaks. With endoscopic stapler-assisted myotomy, a double row of staples is placed along the cut edges, reducing the risk of perforation and bleeding. Stapling may not be technically feasible if the diverticulum is short (<3 cm), because not enough of the stapler will fit into the diverticulum. Modifications of the stapler and other techniques may improve results in short diverticula.19 Conversion from an endoscopic to an open approach may be necessary in about 10% of patients. Overall, 90% of patients have long-term satisfactory results after endoscopic stapling.17 Complications of endoscopic procedures include bleeding, perforation, and leaks, but these are uncommon if a stapler-assisted technique is used.
Flexible fiberoptic endoscopic techniques also have a role in the treatment of Zenker’s diverticula. Rigid diverticuloscopes cannot be used in patients who have limited neck extension or limited ability to open their mouth.15 Flexible fiberoptic techniques do not require general anesthesia. To improve exposure and stabilize the diverticulum, a transparent cap may be attached to the tip of the endoscope.20–22 Another device developed for this purpose is a soft diverticuloscope used as an overtube.23,24 A variety of techniques are used to perform the endoscopic myotomy, including needle knife, argon plasma coagulation, and monopolar forceps. Several sessions may be required to achieve an adequate myotomy. Complications of fiberoptic flexible techniques include cervical and mediastinal air dissection, which are common, as well as perforation and mediastinitis. Persistent or recurrent symptoms have been reported in 10% to 15% of cases.
DIVERTICULA OF THE ESOPHAGEAL BODY
Cause and Pathogenesis
Diverticula of the esophageal body are most commonly located in the middle or lower third of the esophagus (Fig. 23-3). Diverticula located near the diaphragmatic hiatus are called epiphrenic diverticula (Fig. 23-4). Congenital bronchopulmonary-foregut malformations can communicate with the esophagus and present as esophageal diverticula.25 Traction diverticula are often related to mediastinal inflammation associated with tuberculosis and histoplasmosis. Enlarged mediastinal lymph nodes from lung malignancies can also lead to traction diverticula. Epiphrenic diverticula are acquired. About 80% are associated with motility disorders, such as achalasia, diffuse esophageal spasm, hypertensive lower esophageal sphincter, and nonspecific motility disorders.26–28 Epiphrenic diverticula have been reported as a complication of obesity surgery.29
Clinical Features and Diagnosis
Congenital and traction diverticula are usually asymptomatic. Bronchopulmonary fistulae can develop, leading to cough, pneumonia, and recurrent bronchopulmonary infections.30 Midbody and distal esophageal diverticula are also usually asymptomatic. If symptoms are not present at diagnosis, they rarely occur during follow-up. When symptoms occur, the most common are dysphagia, food regurgitation, reflux, weight loss, and chest discomfort.31 Dysphagia may be caused by an underlying motility disorder or by extrinsic compression of the esophagus by a large diverticulum, with preferential filling.32,33
An epiphrenic diverticulum may be mistaken for a diaphragmatic hernia or duplication cyst on chest radiography. Diagnosis is best made by barium swallow, which serves to visualize the diverticulum and localizes it more precisely than endoscopy (see Fig. 23-4).
Squamous cell carcinoma has been reported in epiphrenic diverticula.34 As with Zenker’s diverticula, accumulation of radioactive iodine tracer in esophageal diverticula has been mistaken for metastatic thyroid cancer.35
Treatment and Prognosis
Asymptomatic diverticula of the esophagus need no treatment. Only those patients with symptoms clearly related to their diverticula should be treated. Preoperative endoscopy and manometry are advisable. It can be difficult to pass a manometry catheter beyond the diverticulum and into the stomach, but documentation of achalasia or diffuse esophageal spasm is helpful for guiding treatment.36 Large diverticula may be inverted or resected. Given the high prevalence of associated motility disorders, esophageal myotomy is performed in most if not all cases.27,28,37 Small diverticula can be treated by myotomy without resection. To prevent gastroesophageal reflux, a nonobstructing fundoplication is usually done.
Surgery for esophageal diverticula may be done by open, laparoscopic, or laparoscopic combined with thoracoscopic techniques.27,28,37,38 Epiphrenic diverticula are often amenable to a laparoscopic approach, which has the advantages of a short hospital stay and a quick return to normal activities.
ESOPHAGEAL INTRAMURAL PSEUDODIVERTICULA
Only about 200 cases have been reported, but EIP are more common than the small number of published case reports would imply. EIP have been demonstrated in about 1% of barium swallow studies.39 In autopsy studies, the incidence has been reported to be as high as 55%.40,41
Cause and Pathogenesis
EIP are abnormally dilated ducts of submucosal glands. They are thought to be acquired, and are often associated with conditions that cause chronic esophageal inflammation. The ducts may become dilated because of periductal inflammation or fibrosis.40,42 Gastroesophageal reflux, chronic candidiasis, previous caustic ingestion, esophageal cancer, and a single case of eosinophilic esophagitis have all been associated with EIP.39,43–45 Esophageal strictures are also commonly associated with EIP.41,46 Marked thickening of the esophageal wall has been noted in some cases by CT or endoscopic ultrasound.47
Clinical Features and Diagnosis
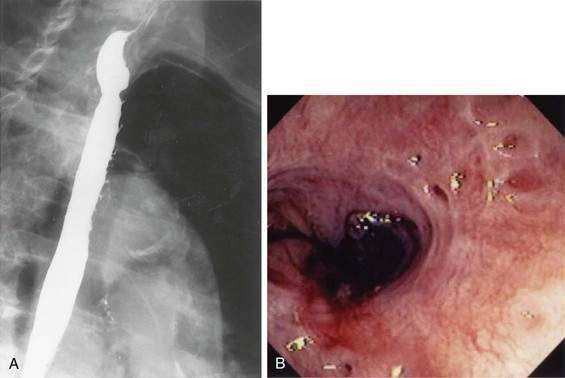
Patients are found to have EIP most commonly in their sixth or seventh decades. The condition is slightly more common in men than in women.41 EIP are discovered most commonly on a barium swallow done for dysphagia or heartburn (Fig. 23-5A). EIP may also be an incidental finding in patients without related symptoms. EIP are usually segmental in distribution, but may be diffuse. Stricture is noted in most cases.41 Tracking or communication between adjacent pseudodiverticula is not uncommon if it is looked for carefully.48 The differential diagnosis on barium swallow examination includes esophageal ulceration. Cancer must be excluded by upper endoscopy if a stricture is present. Although the endoscopic appearance of EIP is characteristic (see Fig. 23-5B), the openings of EIP are small and are often missed. EIP located within an area of stricture are particularly difficult to see at endoscopy. Symptoms, when present, are generally related to the associated condition, such as stricture, cancer, acid reflux, or candidiasis, rather than to the EIP. There have been case reports of perforation of EIP leading to mediastinitis.49
GASTRIC DIVERTICULA
Gastric diverticula are found in less than 1% of upper gastrointestinal x-rays or autopsies.51 Juxtacardiac diverticula make up 75% of all gastric diverticula. These are most often located near the gastroesophageal junction, on the posterior aspect of the lesser curvature.52 They are most commonly found in middle-aged patients, although cases have been reported in children and adolescents.53–55 They range in size from 1 to 3 cm in diameter (Fig. 23-6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree