Fig. 1 a–c
a A 3D view of the ascending colon showing a smooth filling defect at the convergence of folds (white arrow). b Corresponding 2D view showing the filling defect with a soft tissue density (white arrow). c Coronal reformat showing a cecum recurvatum internum with acute flexure, causing compression of the pericolic fat and vascular structures at the inner side (white arrow)
Troubleshooting the flexural pseudotumor:
Smoothly thickened fold located at flexures.
Presence of fat, convergence of folds.
Compare both acquisitions — 3D and 2D.
Anorectal Region
The rectum is particularly difficult to inspect. Special attention is needed for the anal margin. This is done by turning the virtual camera backward toward the anal margin. Good visualization of this segment may be hampered by the rectal catheter and its small insufflated balloon, which prevents dislocation from the rectum. To obtain a good view of the region, it is mandatory to deflate the balloon before the second acquisition. Besides a true polyp or tumor, several tumor-like conditions are possible at and around the anal margin [8–10].
Rectal Folds
The rectum presents with a longitudinal fold arising from the anal margin (rectal bar). This fold is located anteriorly to the rectal catheter (at 12 o’clock). In 2D, it may mimic a polyp; 3D shows its exact nature. Sometimes, more than one fold is present.
Hypertrophied Anal Papilla
The hypertrophied anal papilla is a benign polypoid protrusion arising on the dentate line. It is not possible to differentiate this lesion from a true polyp. Therefore, whenever the lesion is ⩾6 mm, rectoscopy is necessary (Fig. 2).
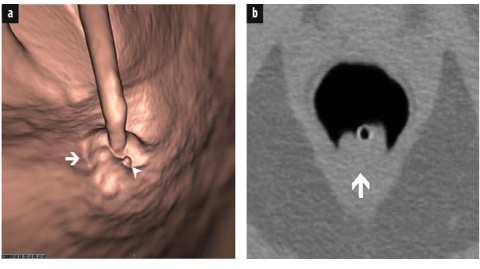
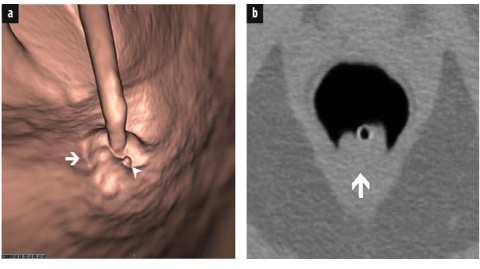
Fig. 2 a, b
a Typical 3D image of internal hemorrhoids surrounding the rectal catheter at the level of the anal margin (white arrow). Additional tiny polypoid defect <5 mm near the hemorrhoids (white arrowhead): most probably a tiny hypertrophied anal papilla. No further investigation is necessary, as this lesion is clearly <5 mm. b Corresponding 2D image shows internal hemorrhoids with soft issue attenuation surrounding the rectal catheter (white arrow)
Internal Hemorrhoids
Internal hemorrhoids are varicose dilatations and arise from the superior hemorrhoidal plexus, superior to the dentate line. They typically appear as smooth filling defects surrounding the rectal catheter, with thin folds converging toward the catheter. They frequently change in appearance on both acquisitions (Fig. 2). In their atypical appearance, they appear as a polypoid lesion, which makes them look like a true polyp. Under this condition, rectoscopy is again necessary whenever the defect is ⩾6mm (Fig. 3).
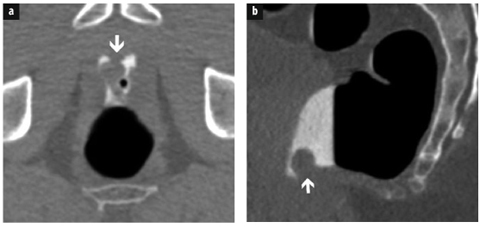
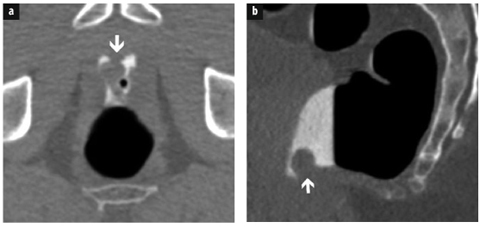
Fig. 3 a, b
a Large filling defect close to the rectal catheter and anal margin (white arrow). Because of this location and the fluid, this lesion is difficult to detect. b Sagittal reformat showing a large polypoid defect highly suspicious of a large polyp (white arrow). Rectoscopy revealed a large, atypical hemorrhoid. This lesion was only visible after deflation of the balloon
Rectal Varix
A rectal varix is a dilated submucosal vein causing a long, serpiginous filling defect. It frequently is less prominent, with better distension of the rectum in the prone position. The varix may appear elsewhere in the colon. It must be noted that, exceptionally, a polyp may also present as a serpiginous filling defect.
Venous Bleb
A venous bleb is a small, venous malformation that may mimic a true polyp.
Troubleshooting the anorectal region:
Take special care to inspect the anal margin.
Know the several possible benign conditions.
Deflate the balloon before the second acquisition.
Be strict: in case of inconclusive diagnosis, perform OC whenever a lesion is ⩾6mm.
Cecum
First identify both ileocecal (IC) valve and appendix when examining the cecum.
As with the rectum, the cecum is challenging to examine. It is a blind-ending segment, with a lumen wider than the other colonic segments. Furthermore, special attention is needed to assess the IC valve and appendix [11].
Ileocecal Valve
The normal IC valve consists of two folds (upper and lower lip) converging at both sides in a prominent fold, the frenulum. These characteristics make it an anatomical landmark of the cecum, which must be identified invariably. The IC valve may have several benign appearances, which must be differentiated from malignant disease.
Lipomatous Transformation
In case of lipomatous transformation, both lips of the IC valve are infiltrated with fatty tissue. On 3D, the IC valve is moderately to excessively enlarged but still shows its normal lip structure. Diagnosis is readily confirmed on 2D, with the IC valve showing typical fat attenuation (0/−100 HU).
Papillary Transformation
In case of papillary transformation, diagnosis is not always straightforward. This entity is caused by protrusion of the terminal ileum into the IC valve and is considered a normal functional status, with the IC valve preventing fluid reflux from the colon into the ileum. The normal lip-like structure becomes distorted and may appear as a bulky mass, with difficult distinction of the two lips. In 3D, a central depression is sometimes present, corresponding to the terminal ileum. Mostly, this condition still shows smooth delineation of the IC valve with some fatty infiltration on 2D imaging. The appearance frequently is different when comparing both acquisitions (Fig. 4). Sometimes a tumor is mimicked, making OC necessary.
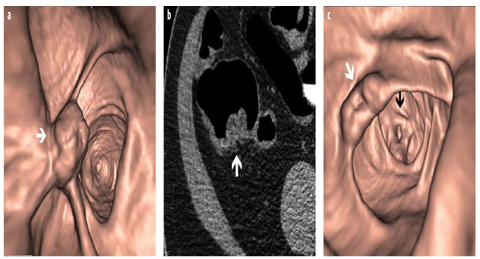
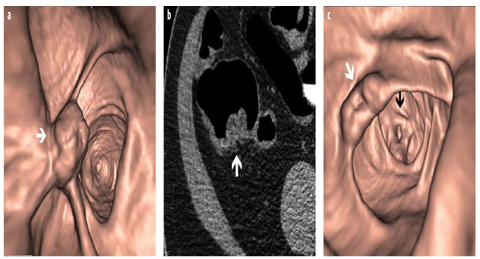
Fig. 4 a–c
a A 3D view of an enlarged ileocecal (IC) valve with distorted aspect in supine acquisition (white arrow). b Corresponding 2D view shows the enlarged IC valve with slightly inhomogeneous soft tissue density (white arrow). c Prone acquisition shows a normal IC valve (white arrow). On the background, a spasm with typical contraction of the taeniae gives a triangular appearance to the lumen of the ascending colon (black arrow)
Troubleshooting the IC valve:
Check the IC valve in 3D and 2D on both acquisitions.
Identify the morphology.
Check the attenuation.
Appendix
The appendix is another landmark in the cecum and appears as a small orifice or depression frequently located in the vicinity of a small fold. It is obvious that we need to inspect the entire appendix in 2D. Therefore, it is mandatory to know whether the patient underwent previous appendectomy. Normally, the appendix presents as a thinwalled, tubular structure, which may be filled with air or contrast. Any global or focal wall thickening should prompt further investigation to rule out malignancy (= appendectomy). Tumoral conditions of the appendix are rare and frequently asymptomatic [12].
Mucocele of the Appendix
An appendiceal mucocele corresponds to a mucus-dilated appendix. It typically is contiguous with the appendix and may present with a mural calcification. When close to the cecum, it frequently produces an extrinsic impression. This entity may correspond to a benign cyst or an obstructed appendix. A malignant cause must always be excluded. Therefore, surgery (appendectomy/right hemicolectomy) is necessary.
Intussusception of the Appendix
Intussusception of the appendix is mostly partial and asymptomatic. It produces a polypoid appearance in 3D and 2D, frequently reducing on one of both acquisitions. If not, and if the luminal defect situated at the appendiceal orifice is ⩾6mm, a true tumoral lesion must be excluded with OC.
Inverted Appendiceal Stump
Following inversion-ligation appendectomy, an older appendectomy technique, the appendiceal stump may cause a pseudopolypoid appearance. This entity cannot be differentiated from a true tumoral lesion, and once again, whenever the lesion is ⩾6 mm, OC is necessary. Furthermore, on rare occasions, a polyp or malignancy may develop in the stump [13].
Troubleshooting the appendix:
Suspicion of significant appendicular pathology should prompt further investigation.
Lesions ⩾6 mm at the appendicular orifice, with soft tissue attenuation, need colonoscopy.
Tumors may develop in an appendicular stump.
Diverticular Disease
Myochosis causes restricted distension of the sigmoid.
Diverticular disease creates many prominent folds with blind spots.
Polyp detection becomes more challenging.
Diverticular disease is frequent in the Western population, with a frequency of ∼30% at age 50 years and >50% at age 60 years. It is mostly located in the sigmoid. Diverticulosis is a challenge for every CTC-reader. In its early stage, the disease is characterized by myochosis: a triad of muscular thickening, taeniae shortening, and luminal narrowing. This causes restricted colonic distension, with prominent, semilunar folds and deep haustrations, making CTC interpretation more challenging. In 3D, there is restricted visualization behind the folds (blind spots), with the deep haustrations increasing these blind spots and requiring dedicated 3D inspection by turning the virtual camera around the folds. To improve colonic distension, the use of Buscopan is justified. Distension can also be improved with an additional acquisition of the affected segment with the patient in the right or left lateral decubitus position.
With myochosis progression, diverticula appear, and semilunar folds become more prominent. In 2D, diverticula are characterized by gas-filled outpouchings on the colonic wall. In 3D, they appear as a complete dark ring, which is in contrast to a polyp, which mostly presents as an incomplete or vague dark ring when viewed en face. Sometimes, this may be confusing. However, comparing 3D with 2D imaging makes differentiation straightforward.
Diverticular disease gives rise to pseudopolypoid lesions [14].
Troubleshooting diverticular disease:
Combine 3D with 2D imaging to inspect diverticular segments.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








