Chapter 33 Diseases of the bile ducts
1 Diseases of the bile ducts (BDs) usually manifest with symptoms and signs related to BD obstruction, including pain, jaundice, pruritus, fever, and elevated serum levels of liver biochemical tests
2 Choledocholithiasis, the most common benign disorder of the biliary tree, may manifest in patients with an intact gallbladder, who usually harbor gallbladder stones, or in patients who have had a cholecystectomy. Predictors of BD stones in patients with a compatible history include elevated liver biochemical test levels, duct dilatation, stones visualized in the duct on imaging studies, and an initial presentation with cholangitis.
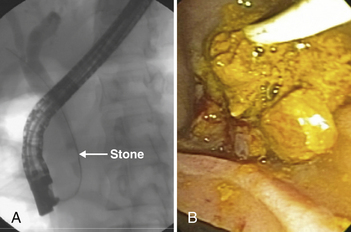
3 In the diagnosis and management of BD stones before laparoscopic cholecystectomy, endoscopic retrograde cholangiopancreatography (ERCP) should be restricted to patients in whom BD stones are strongly suspected and in whom therapeutic intervention is likely. Magnetic resonance cholangiopancreatography (MRCP) is used commonly for noninvasive diagnosis. Endoscopic ultrasonography is also highly sensitive and specific.
4 Endoscopic sphincterotomy is the most common technique used for removal of BD stones, either before or after cholecystectomy. Laparoscopic extraction of BD stones during cholecystectomy is an alternative approach when intraoperative cholangiography results are positive and surgical expertise is available.
5 Endoscopic intervention plays an important role in the diagnosis and treatment of complications of cholecystectomy, such as biliary leaks and strictures.
Bile Duct Stones
Composition
2. Black pigment stones are formed in the gallbladder and are associated with hemolytic disorders such as sickle cell disease. They are also common in persons with cirrhosis.
Clinical features
3. Features of cholangitis include the following:
 Charcot’s triad, consisting of abdominal pain, fever, and jaundice: Each feature may not be present in all patients with cholangitis.
Charcot’s triad, consisting of abdominal pain, fever, and jaundice: Each feature may not be present in all patients with cholangitis.
 Charcot’s triad, consisting of abdominal pain, fever, and jaundice: Each feature may not be present in all patients with cholangitis.
Charcot’s triad, consisting of abdominal pain, fever, and jaundice: Each feature may not be present in all patients with cholangitis.Laboratory features
1. Elevations in serum liver biochemical test levels include alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase, gamma glutamyltranspeptidase (GGTP), and bilirubin.
 Marked elevations in serum ALT and AST levels may occur, even levels higher than 1000 U/L transiently, especially with cholangitis.
Marked elevations in serum ALT and AST levels may occur, even levels higher than 1000 U/L transiently, especially with cholangitis.
 Marked elevations in serum ALT and AST levels may occur, even levels higher than 1000 U/L transiently, especially with cholangitis.
Marked elevations in serum ALT and AST levels may occur, even levels higher than 1000 U/L transiently, especially with cholangitis.Imaging studies
6. Percutaneous transhepatic cholangiography (THC)
 Seldom used for evaluation or treatment of BD stones, except with acute cholangitis when ERCP is unavailable or fails or is anatomically impossible because of prior surgery
Seldom used for evaluation or treatment of BD stones, except with acute cholangitis when ERCP is unavailable or fails or is anatomically impossible because of prior surgery
 Seldom used for evaluation or treatment of BD stones, except with acute cholangitis when ERCP is unavailable or fails or is anatomically impossible because of prior surgery
Seldom used for evaluation or treatment of BD stones, except with acute cholangitis when ERCP is unavailable or fails or is anatomically impossible because of prior surgeryTreatment
1. ERCP and endoscopic sphincterotomy: treatment of choice at most centers
 Most common treatment of BD stones when laparoscopic cholecystectomy is planned and BD stones are documented or strongly suspected
Most common treatment of BD stones when laparoscopic cholecystectomy is planned and BD stones are documented or strongly suspected
 Most common treatment of BD stones when laparoscopic cholecystectomy is planned and BD stones are documented or strongly suspected
Most common treatment of BD stones when laparoscopic cholecystectomy is planned and BD stones are documented or strongly suspected3. Laparoscopic cholecystectomy plus extraction of BD stones
 High success rates (80% to 90%) are reported by expert surgeons when IOC results are positive for BD stones.
High success rates (80% to 90%) are reported by expert surgeons when IOC results are positive for BD stones.
 High success rates (80% to 90%) are reported by expert surgeons when IOC results are positive for BD stones.
High success rates (80% to 90%) are reported by expert surgeons when IOC results are positive for BD stones.4. Open choledochotomy
 This was standard care before ERCP in the 1970s; it is seldom performed currently except for large retained stones not extractable by other methods.
This was standard care before ERCP in the 1970s; it is seldom performed currently except for large retained stones not extractable by other methods.
 It is performed either at the time of cholecystectomy or after a patient presents with symptomatic choledocholithiasis.
It is performed either at the time of cholecystectomy or after a patient presents with symptomatic choledocholithiasis.
 This was standard care before ERCP in the 1970s; it is seldom performed currently except for large retained stones not extractable by other methods.
This was standard care before ERCP in the 1970s; it is seldom performed currently except for large retained stones not extractable by other methods. It is performed either at the time of cholecystectomy or after a patient presents with symptomatic choledocholithiasis.
It is performed either at the time of cholecystectomy or after a patient presents with symptomatic choledocholithiasis.5. ERCP techniques for the treatment of choledocholithiasis
 Guidewire cannulation of BD using a sphincterotome is a common technique; the sphincterotome is advanced over a guidewire into the BD.
Guidewire cannulation of BD using a sphincterotome is a common technique; the sphincterotome is advanced over a guidewire into the BD.
 Guidewire cannulation of BD using a sphincterotome is a common technique; the sphincterotome is advanced over a guidewire into the BD.
Guidewire cannulation of BD using a sphincterotome is a common technique; the sphincterotome is advanced over a guidewire into the BD.6. Large stones: may require more advanced ERCP techniques
 Laser lithotripsy through choledochoscopy: “baby scope” inserted into the BD through the channel of a side-viewing endoscope
Laser lithotripsy through choledochoscopy: “baby scope” inserted into the BD through the channel of a side-viewing endoscope
 Laser lithotripsy through choledochoscopy: “baby scope” inserted into the BD through the channel of a side-viewing endoscope
Laser lithotripsy through choledochoscopy: “baby scope” inserted into the BD through the channel of a side-viewing endoscope7. Complications of ERCP and sphincterotomy
a. Pancreatitis occurs in 5% of patients. It may result either from the diagnostic portion of the procedure or from cautery-induced injury to the pancreatic duct orifice.
 Pancreatitis is more common in patients with a difficult cannulation, suspected or proven sphincter of Oddi dysfunction (SOD), or a needle-knife precut sphincterotomy.
Pancreatitis is more common in patients with a difficult cannulation, suspected or proven sphincter of Oddi dysfunction (SOD), or a needle-knife precut sphincterotomy.
 Pancreatitis is more common in patients with a difficult cannulation, suspected or proven sphincter of Oddi dysfunction (SOD), or a needle-knife precut sphincterotomy.
Pancreatitis is more common in patients with a difficult cannulation, suspected or proven sphincter of Oddi dysfunction (SOD), or a needle-knife precut sphincterotomy.