2 Difficulty swallowing and pain on swallowing
Case
A 28-year-old male presents with a 10 year history of intermittent (roughly 2 monthly), non-progressive dysphagia for solids, but not liquids. He perceives bolus holdup in the neck. Sips of water help resolve minor dysphagia episodes. He has had two visits to the Accident and Emergency Department in 10 years for endoscopic disimpaction of meat boluses, but the endoscopist reported the oesophagus appeared entirely normal and the bolus had passed spontaneously on both occasions. He has had two barium radiographs performed in this time; both were normal. He denies heartburn, chest pain, regurgitation or weight loss. He suffered from asthma as a child. He takes no medications and has no prior medical history. He denies deglutitive cough and post-nasal regurgitation, and has no need for multiple swallows to clear liquid from the pharynx.
Pain on Swallowing (Odynophagia)
Odynophagia is the symptom of pain on swallowing, generally arising from irritation of an inflamed or ulcerated mucosa by the swallowed bolus during its passage through the oesophagus. Mucosal injury causing odynophagia can be caused by infective (viral or fungal) oesophagitis or by mucosal ulceration secondary to corrosive agents (e.g. tablets or reflux oesophagitis) (Box 2.1). The symptom of odynophagia almost invariably warrants endoscopy to elucidate the cause, which may need biopsy confirmation.
Gastro-oesophageal reflux disease
Reflux oesophagitis can cause odynophagia. The patient typically describes a sensation of pain or discomfort coincident with passage of the bolus through the oesophagus, sometimes combined with a sense of transient bolus hold-up. The sense of bolus arrest can dominate the symptom complex if the oesophagitis has progressed to stricture formation, but is not infrequently perceived even in the absence of a stricture. For a detailed account of investigation and management of reflux disease, refer to Chapter 1.
Dysphagia
Causes of dysphagia
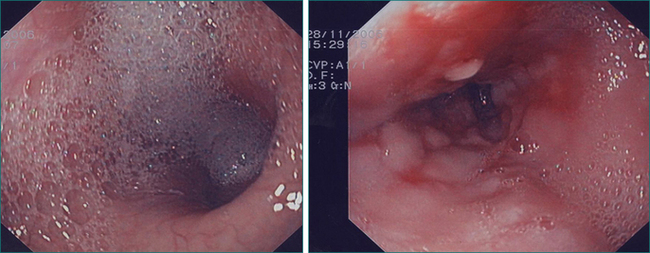
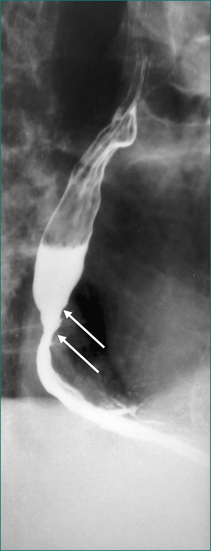
Oral-pharyngeal dysphagia is most commonly related to neuromuscular dysfunction, most commonly stroke (Box 2.2). Head and neck surgery and radiotherapy, for malignant disease, are also very commonly associated with oral-pharyngeal dysphagia. Other structural disorders causing oral-pharyngeal dysphagia include strictures, mucosal webs (Fig 2.1) and pharyngeal diverticulum.
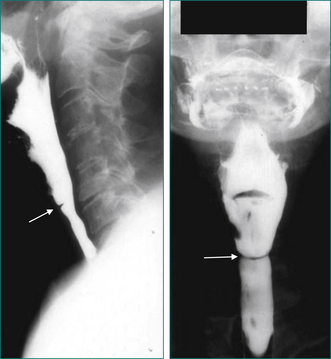
Figure 2.1 Mucosal web in the cervical oesophagus seen in lateral view (left) and anteroposterior view (right).
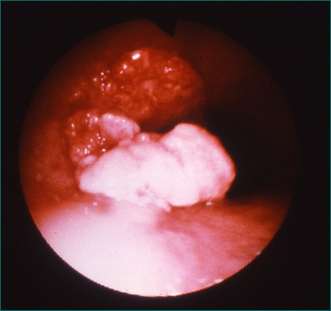
Because gastro-oesophageal reflux disease is prevalent, peptic oesophageal strictures are a very common cause of oesophageal dysphagia (Figs 2.2 and 2.3, Box 2.3). In these cases, there is frequently a prior history of reflux symptoms. Mucosal rings, such as the Schatzki ring at the cardio-oesophageal junction, are a common cause of intermittent oesophageal dysphagia. Malignant oesophageal obstruction is usually evident on history by virtue of a short history of rapidly progressive dysphagia and significant weight loss (Fig 2.4).
Box 2.3 Causes of oesophageal dysphagia
Structural disorders
Stricture (peptic, caustic, pill-induced, radiation-induced)
Extrinsic compression (e.g. aberrant R subclavian artery, mediastinal or bronchial tumour)