Circulating agents cause intestinal secretion or changes in motility with decreased intestinal transit time, resulting in secretory-type diarrhea. Secretory diarrhea as opposed to osmotic diarrhea is characterized by large-volume, watery stools, often more than 1 L per day; by persistence of diarrhea when patients fast; and by the fact that on analysis of stool-water, measured osmolarity is identical to that calculated from the electrolytes present. Although sodium plays the main role in water and electrolyte absorption, chloride is the major ion involved in secretion.
- •
Circulating agents reach intestinal epithelial cells and change water and electrolyte absorption to secretion.
- •
In Verner-Morrison syndrome (also known as pancreatic cholera or watery diarrhea, hypokalemia, hypochlorhydria [WDHH] syndrome), vasoactive intestinal polypeptide (VIP) released from a neuroendocrine tumor causes secretory diarrhea. The syndrome can be mimicked by intravenous VIP infusion in healthy subjects.
- •
In malignant carcinoid syndrome, secretory diarrhea is accompanied by flushing, right-sided endocardial fibrosis and sometimes bronchospasm.
- •
In Zollinger-Ellison syndrome (ZES), high levels of circulating gastrin lead to many liters of gastric secretions per day, a volume that overwhelms the absorptive capacity of the intestine and results in diarrhea.
- •
In many of the endocrine diarrhea syndromes, a somatostatin analog is capable of reducing diarrhea by decreasing the release of hormones and other tumor products from the neoplasms.
Introduction
In the syndromes to be described, circulating agents cause intestinal secretion or changes in motility with decreased intestinal transit time, resulting in secretory-type diarrhea. Secretory diarrhea as opposed to osmotic diarrhea is characterized by large-volume, watery stools, often more than 1 L per day; by persistence of diarrhea when patients fast; and by the fact that on analysis of stool-water, measured osmolarity is identical to that calculated from the electrolytes present. This calculation is done by analyzing the sodium and potassium concentrations, multiplying their sum by 2 to account for the anions, and comparing this number to the measured osmolarity.
Although sodium plays the main role in water and electrolyte absorption, chloride is the major ion involved in secretion. Several intracellular steps result in exit of chloride ions from epithelial cells through a chloride-specific channel in the apical membrane. This process can be initiated from the luminal side, for instance, by cholera toxin or from the serosal side by circulating agents, such as serotonin or VIP. Both cholera toxin and VIP trigger increases in intracellular cyclic adenosine monophosphate (cAMP), which causes active chloride secretion. A list of agents that cause secretion in vitro (applied from the serosal side of intestinal mucosa) or in vivo (as circulating agents) is given in Table 1 .
| Hormones | Gastrin, secretin, cholecystokinin, glucagon, enteroglucagon, gastric inhibitory polypeptide, calcitonin |
| Neuroendocrine substances | Acetylcholine, VIP, peptide histidine methionine, helodermin, substance P, bombesin, neurotensin, serotonin, galanin-1, adenosine triphosphate |
| Other substances | Histamine, bradykinin, prostaglandins |
The classic endocrine diarrheal syndrome: Verner-Morrison syndrome or VIPoma syndrome
Other names for Verner-Morrison syndrome or VIPoma syndrome are pancreatic cholera syndrome and watery diarrhea hypokalemia hypochlorhydria (WDHH) syndrome. VIP is produced by a pancreatic tumor. VIP under normal circumstances serves as a neurotransmitter in the peripheral and central nervous system, particularly in the enteric nervous system and in the urogenital tract. The normally seen low levels of serum VIP are viewed as a neuronal overflow phenomenon. Only in the presence of a VIP-producing tumor are the serum concentrations elevated. These tumors occur with a frequency of 1 case per 10 million population per year.
Verner and Morrison of Duke University first called attention to this syndrome in association with an islet cell tumor. Before the discovery of VIP (see below) it was the hypochlorhydria that differentiated this syndrome from the Zollinger-Ellison syndrome (ZES) described 3 years previously. The name, pancreatic cholera syndrome , was first used by Matsumoto and coworkers. Pancreatic cholera syndrome is an appropriate name because the diarrhea results from cAMP-mediated intestinal secretion, as in Asiatic cholera. The only shortcoming of this term is that some tumors are outside the pancreas (eg, ganglioneuroblastomas or other neural crest tumors). Bloom and colleagues first found elevated levels of VIP in plasma and in tumor tissue of such patients.
VIP was discovered and isolated by Said and Mutt between 1968 and 1972. It is a 28–amino acid polypeptide with a molecular weight of 3326. Initially discovered as a vasoactive substance, VIP was once viewed as a gastrointestinal hormone by Morton Grossman before it became clear that its major role is that of a neurotransmitter.
VIP is an intestinal secretagogue and causes active chloride and bicarbonate secretion by intestinal epithelia. In intestinal perfusion experiments in dogs and in humans, the authors have shown active chloride secretion (against a chemical and electrical gradient) in response to VIP. A smaller effect can also be seen in the colon. In healthy volunteers, VIP infusion over 10 hours to reach plasma levels similar to those seen in patients with pancreatic cholera can mimic the syndrome (an average of 2.4 L of stool in 10 hours).
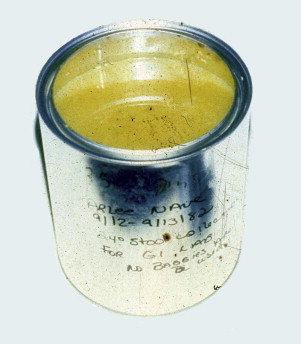
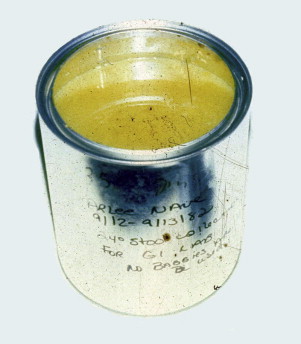
The large fluid loss in such patients (the authors have observed diarrhea volumes up to 10 L per day) and the loss of bicarbonate in stool water lead to metabolic acidosis and hypokalemia (the colon preserves sodium but loses potassium in exchange). Untreated patients die of renal failure due to hypovolemia. The authors have measured an average stool volume of 4.5 L per day in 9 such patients who were eating a regular diet (1.8 L while fasting). A typical stool collection is shown in Fig. 1 . Resection of the tumor is the therapy of choice; however, more than 50% of the patients have liver metastases at the time of diagnosis.
Treatment with somatostatin analog has been effective and chemotherapy with streptozotocin and 5-fluorouracil (5-FU) is also beneficial. A large armamentarium of other therapeutic options is now available, includeing targeted therapy with everolimus, radioligand therapy, and chemoembolization. In rare cases, when after resection of the primary tumor the remaining metastases are limited to the liver, partial hepatectomy or liver transplantation can be performed. In some of the tumors, other peptides are cosecreted, such as peptide histidine methionine, calcitonin, and helodermin. All these agents are capable of changing absorption to secretion in the intestine, but the main mediator of intestinal secretion and thus of diarrhea, is VIP. There is also a troublesome syndrome referred to as pseudopancreatic cholera in which no tumor or circulating secretagogue can be found in the presence of long-lasting secretory diarrhea.
The classic endocrine diarrheal syndrome: Verner-Morrison syndrome or VIPoma syndrome
Other names for Verner-Morrison syndrome or VIPoma syndrome are pancreatic cholera syndrome and watery diarrhea hypokalemia hypochlorhydria (WDHH) syndrome. VIP is produced by a pancreatic tumor. VIP under normal circumstances serves as a neurotransmitter in the peripheral and central nervous system, particularly in the enteric nervous system and in the urogenital tract. The normally seen low levels of serum VIP are viewed as a neuronal overflow phenomenon. Only in the presence of a VIP-producing tumor are the serum concentrations elevated. These tumors occur with a frequency of 1 case per 10 million population per year.
Verner and Morrison of Duke University first called attention to this syndrome in association with an islet cell tumor. Before the discovery of VIP (see below) it was the hypochlorhydria that differentiated this syndrome from the Zollinger-Ellison syndrome (ZES) described 3 years previously. The name, pancreatic cholera syndrome , was first used by Matsumoto and coworkers. Pancreatic cholera syndrome is an appropriate name because the diarrhea results from cAMP-mediated intestinal secretion, as in Asiatic cholera. The only shortcoming of this term is that some tumors are outside the pancreas (eg, ganglioneuroblastomas or other neural crest tumors). Bloom and colleagues first found elevated levels of VIP in plasma and in tumor tissue of such patients.
VIP was discovered and isolated by Said and Mutt between 1968 and 1972. It is a 28–amino acid polypeptide with a molecular weight of 3326. Initially discovered as a vasoactive substance, VIP was once viewed as a gastrointestinal hormone by Morton Grossman before it became clear that its major role is that of a neurotransmitter.
VIP is an intestinal secretagogue and causes active chloride and bicarbonate secretion by intestinal epithelia. In intestinal perfusion experiments in dogs and in humans, the authors have shown active chloride secretion (against a chemical and electrical gradient) in response to VIP. A smaller effect can also be seen in the colon. In healthy volunteers, VIP infusion over 10 hours to reach plasma levels similar to those seen in patients with pancreatic cholera can mimic the syndrome (an average of 2.4 L of stool in 10 hours).
The large fluid loss in such patients (the authors have observed diarrhea volumes up to 10 L per day) and the loss of bicarbonate in stool water lead to metabolic acidosis and hypokalemia (the colon preserves sodium but loses potassium in exchange). Untreated patients die of renal failure due to hypovolemia. The authors have measured an average stool volume of 4.5 L per day in 9 such patients who were eating a regular diet (1.8 L while fasting). A typical stool collection is shown in Fig. 1 . Resection of the tumor is the therapy of choice; however, more than 50% of the patients have liver metastases at the time of diagnosis.
Treatment with somatostatin analog has been effective and chemotherapy with streptozotocin and 5-fluorouracil (5-FU) is also beneficial. A large armamentarium of other therapeutic options is now available, includeing targeted therapy with everolimus, radioligand therapy, and chemoembolization. In rare cases, when after resection of the primary tumor the remaining metastases are limited to the liver, partial hepatectomy or liver transplantation can be performed. In some of the tumors, other peptides are cosecreted, such as peptide histidine methionine, calcitonin, and helodermin. All these agents are capable of changing absorption to secretion in the intestine, but the main mediator of intestinal secretion and thus of diarrhea, is VIP. There is also a troublesome syndrome referred to as pseudopancreatic cholera in which no tumor or circulating secretagogue can be found in the presence of long-lasting secretory diarrhea.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





