Fig. 3.1
Los Angeles (LA) classification of erosive esophagitis. Grade A: One (or more) mucosal break no longer than 5 mm that does not extend between the tops of two mucosal folds. Grade B: One (or more) mucosal breaks more than 5 mm long that does not extend between the tops or two mucosal folds. Grade C: One (or more) mucosal break that is continuous between the tops of two or more mucosal folds but which involved less than 75 % of the circumference. Grade D: One (or more) mucosal break which involves at least 75 % of the esophageal circumference [21]
However, similar to the use of radiographic studies for the diagnosis of GERD, sensitivity remains low. In a population-based study from northern Sweden using a validated questionnaire for gastroesophageal reflux symptoms, the prevalence of symptoms was 33.6 %. Endoscopy was performed on a random subset of the responders demonstrating mucosal breaks and erosive esophagitis in a total of 15.5 % of the sample population. Among those with gastroesophageal reflux symptoms as the reference standard, only 24.5 % had evidence of erosive esophagitis [22]. Therefore, with the recognition that 70–85 % of patients with symptoms of GERD have nonerosive reflux disease (NERD) , the role of endoscopy for the detection of erosive esophagitis as the basis for the diagnosis of GERD is limited and not cost-effective [8, 23–25]. Furthermore, initial empiric diagnostic and treatment strategies for GERD limit the utility of endoscopy in the diagnosis of GERD as independent predictors for the demonstration of NERD include PPI use prior to endoscopy, the absence of nocturnal symptoms, age ≥ 60, and the absence of a hiatal hernia [26] .
Although endoscopy has limited sensitivity in the diagnosis of GERD, endoscopy allows for a detailed evaluation to rule out alternative diagnoses such as eosinophilic esophagitis, infection, or pill-induced injury, as well as for sampling of rings and strictures and for screening of Barrett’s esophagus [2, 6] . While screening for Barrett’s remains controversial, a number of studies highlight similar risk factors associated with the presence of Barrett’s esophagus to include male sex, older age (> 40 years), and prolonged duration of symptoms (> 13 years) [27–29]. Barrett’s esophagus is suspected endoscopically when the pale pink squamous mucosa of the distal esophagus is replaced to various lengths with salmon-pink columnar mucosa (Fig. 3.2). In Barrett’s esophagus , the SCJ is displaced proximal to the gastroesophageal junction (GEJ or Z line; defined by the proximal margin of the gastric folds), and the diagnosis is confirmed with a biopsy finding of intestinal metaplasia, which is different from normal esophageal mucosa lined by stratified squamous mucosa. Intestinal metaplasia is characterized by mucin-containing goblet cells, which can be detected by routine hematoxylin and eosin stain or accentuated with an alcian blue stain. Barrett’s esophagus may be divided into short-segment Barrett’s esophagus (SSBE) and long-segment Barrett’s esophagus (LSBE) types according to whether the metaplasia is longer or shorter than 3 cm. It is more common to find dysplasia and cancer in a patient with LSBE, but patients with SSBE are also at increased risk.
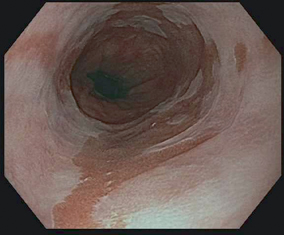
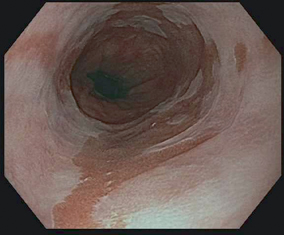
Fig. 3.2
Endoscopic appearance of long-segment Barrett’s metaplasia extending proximally from the gastroesophageal junction (salmon-pink columnar mucosa)
Advanced endoscopic imaging techniques have been evaluated as a method of improving the sensitivity of endoscopy in the diagnosis of GERD. Narrow-band imaging (NBI) utilizes a blue/green wavelength of light to illuminate the mucosa and preferentially enhance the superficial tissue structures emphasizing features such as capillary and mucosal patterns without the use of dyes. The use of NBI has been used to improve the visualization of the SCJ and thus improving the ability to assess for erosive disease. In a prospective study of 80 patients (50 with GERD as defined by validated questionnaire, of which 30 had endoscopically erosive esophagitis) , the use of NBI magnified images demonstrated that an increased number and presence of dilated intrapapillary capillary loops were the best predictors for a diagnosis of GERD with a 92 % sensitivity and 100 % specificity (when combined with the presence of microerosions). In addition, an increased number and presence of dilated intrapapillary capillary loops were able to differentiate patients with NERD compared to a control group [30]. A second study assessing the role of NBI in examination of the SCJ included 107 subjects (36 with NERD, 41 with erosive esophagitis, and 30 controls). A combination of increased vascular pattern and absence of round pit pattern was able to distinguish NERD from controls with a sensitivity of 86.1 % and specificity of 83.3 % [31]. Therefore, advanced imaging techniques may provide endoscopy with an improved sensitivity for the diagnosis of GERD.
Esophageal Biopsy
The addition of esophageal biopsies to endoscopy allows for histologic assessment in order to assess for microscopic mucosal injury, rule out alternative diagnoses such as eosinophlic esophagitis, and assess for disease complications such as the development of Barrett’s esophagus or neoplasia. Early histologic studies in asymptomatic patients and in whom no reflux was demonstrated by pH studies detailed the normal histologic appearance of the esophageal mucosa characterized by dermal papillae that extended less than halfway to the free luminal margin and a basal cell layer occupying less than 15 % of the total thickness of the epithelium. Polymorphonuclear leukocytes were never found in the lamina propria, and eosinophils were uncommon. However, in those with symptomatic reflux and positive pH studies, the dermal papillae extended more than 50 % of the distance to the epithelial surface and the basal cell layer accounted for more than 15 % of the epithelial thickness. Polymorphonuclear cells and eosinophils were seen in the lamina propria in severe cases of esophagitis [14]. In the initial study by Ismail-Beigi, 28 of 33 patients with reflux had at least one abnormal biopsy (85 % sensitivity) while 19 of 21 control subjects had normal biopsies (90 % specificity) [32]. However, a subsequent study defining GERD patients based on 24-h ambulatory pH monitoring was unable to replicate the sensitivity of basal zone thickness or papillary length for the diagnosis of GERD [33].
Outside of the use of light microscopy for a diagnosis of GERD, transmission electron microscopy has been used to evaluate the dilated intercellular space (DIS) diameter. In a study of 11 patients with heartburn (6 with erosive esophagitis) and 13 controls, 8 of the 11 with heartburn and no controls demonstrated an intercellular space diameter of ≥ 2.4 µm, demonstrating a 73 % sensitivity and 100 % specificity as a histologic discriminator for GERD [34].
In a more recent analysis of 258 subjects with GERD diagnosed based on the presence of reflux esophagitis , abnormal distal pH monitoring or ≥ 95 % symptom association probability (SAP), the presence of eosinophils, total epithelial thickness, and papillary length were significant predictors of GERD. Total epithelial thickness measured 0.5 cm above the Z line demonstrated a sensitivity of 77 % and specificity of 52 % for the diagnosis of GERD [24]. Furthermore, combining histologic features has the ability to improve the test characteristics of esophageal biopsy for the diagnosis of GERD as demonstrated in a study of 119 patients with GERD symptoms and 20 control patients with normal 24-h ambulatory pH monitoring in which biopsies were obtained at the Z line, 4 cm from the Z line, and 2 cm from the Z line. A combination of histologic assessment was performed for basal cell layer, length of papillae, and DIS, which were semiquantitatively scored 0–2 and combined with the presence of intraepithelial eosinophils, neutrophils, and necrosis/erosions resulting in a final histologic “reflux score.” ROCs demonstrated that for a score of > 2, the “reflux score” had 84 % sensitivity and 85 % specificity for the diagnosis of GERD [35].
The optimal use of histologic parameters in the diagnosis of GERD remains in the ability to rule out alternative diagnoses as the use of esophageal biopsy for the diagnosis of GERD is limited by interobserver variability in identifying and grading relevant features [24]. In a review of five studies, regardless of histologic criteria, esophageal biopsy for a diagnosis of GERD had an overall sensitivity of 77 % and specificity of 91 % [14]. Given the insensitive test characteristics of histology in the diagnosis of GERD, the routine use of biopsy of the esophagus cannot be recommended in a patient with heartburn and normal endoscopy and therefore should only be taken when other causes of esophagitis are suspected [2, 6].
Manometry
Esophageal manometry is a diagnostic test that measures intraluminal pressures and coordination of the pressure activities of the three functional regions of the esophagus: LES, esophageal body, and upper esophageal sphincter (UES). Manometry is performed with the use of either a water-infusion catheter or a solid-state catheter system. Solid-state catheters contain embedded microtransducers that directly measure the esophageal contractions. Water-perfused catheters contain several small-caliber lumens that are perfused with water from a low-compliance perfusion device. When a catheter port is occluded by an esophageal contraction, water pressure builds within the catheter, exerting a force that is conveyed to an external transducer. With either catheter system, the electrical signals from the transducers are transmitted to a computer, which produces a graphic record.
Manometry is commonly used in the assessment of patients with symptoms suggestive of esophageal motor dysfunction, such as dysphagia and noncardiac chest pain. The role of manometry in the evaluation of GERD is limited to the accurate placement of catheter-based ambulatory 24-h esophageal pH monitoring and evaluation of esophageal peristalsis prior to antireflux surgery. Patients with achalasia can present with heartburn and regurgitation mimicking a diagnosis of GERD, and achalasia is a manometric contraindication to antireflux surgery [36, 37]. Manometry may also be helpful in patients with a primary symptom of regurgitation as it can help differentiate rumination syndrome from GERD [6].
Ambulatory Reflux Monitoring
Ambulatory 24-h esophageal pH monitoring is an important tool in the diagnosis and management of GERD. Esophageal pH monitoring can detect and quantify gastroesophageal reflux and correlate symptoms temporally with reflux. The primary indications for ambulatory 24-h esophageal pH monitoring are (1) to document excessive acid reflux in patients with suspected GERD but without endoscopic esophagitis, (2) to assess reflux frequency, and (3) to assess symptom association .
Standard ambulatory 24-h esophageal pH monitoring measures distal esophageal acid exposure by using a single pH electrode catheter that is passed through the nose and positioned 5 cm above the superior margin of the manometrically determined LES. Although other techniques for electrode placement exist, such as pH step-up (rise in pH from stomach to esophagus) and endoscopic and fluoroscopic placement, they are less accurate and not standardized [38, 39]. After catheter placement, the patient is encouraged to conduct a typical day without dietary or activity limitations. Because ingestion of foods or liquids with a pH < 4.0 can mimic reflux events and produce false-positive results, acidic foods or drinks should be excluded from the analysis period or accurately noted in the pH diary [40, 41]. In using a catheter-based system, the pH is recorded every 4–6 s, and the data are transmitted to an ambulatory data logger. Faster sampling frequencies up to 1 Hz can lead to the detection of a greater number of reflux events but do not change the overall acid exposure values [42].
Typical ambulatory esophageal pH monitoring units have an event marker that can be activated by the patient during the study to indicate the timing of symptoms, meals, and recumbent positioning. The patient also records these events on a diary card so that specific symptoms can later be correlated with the esophageal acid exposure as recorded by the pH probe. At the end of the study, data are downloaded to a computer, which generates a pH tracing and a data summary. The typical duration for clinical esophageal pH monitoring catheter-based systems is 24 h. Shorter study periods ranging from 3 to 16 h have been studied as a result of poor patient tolerance to the pH catheters; however, shorter study durations have resulted in decreased sensitivity compared to 24-h monitoring [41, 43–45] .
When performing study interpretation, a reflux episode is defined when the esophageal pH drops below 4.0. This value is chosen on the basis of the proteolytic activity of pepsin, which is most active at and below this pH. Additionally, a pH value less than 4.0 best distinguishes between symptomatic patients and asymptomatic controls [46–49]. Although many scoring systems and parameters have been evaluated, the percentage of time that the pH is less than 4 is the single most important parameter to measure and is calculated in most software programs used in the analysis of pH monitoring. Results are generally considered abnormal when the total time that the pH is less than 4 exceeds 4.2 % of the study period [50,51]. Stratification by supine time and upright time is also reported by all software programs.
Although the pH software automatically calculates the total, upright, and supine reflux times, manual review of the pH tracing to exclude artifact is essential for precise interpretation. A typical reflux event involves an abrupt drop in pH. This must be distinguished from a slowly drifting pH value, which may be secondary to the probe’s losing contact with the esophageal mucosa and drying out. Probe dysfunction or disconnection can result in a reading that drops to zero. In addition, some patients may sip on acidic carbonated or citrus beverages, causing prolonged periods during which pH is less than 4. These artifacts should be identified, and their corresponding time excluded from the calculation of acid exposure times .
Multiple-probe catheters have additional pH electrodes located more proximally in the esophagus or the hypopharynx. These electrodes allow for the detection of proximal esophageal and pharyngeal acid reflux events, which may be useful in the evaluation of extraesophageal GERD symptoms, particularly laryngitis, chronic cough, and asthma. The conventional location of the proximal esophageal pH probe is 15–20 cm above the LES, with a normal value for total time with pH below 4.0 being less than 1 % [52, 53]. The hypopharyngeal probe is usually placed 2 cm above the manometrically determined UES. Although normal values are not clearly defined, more than two or three episodes of hypopharyngeal reflux are considered abnormal. It is again critical to review the pH tracings to be sure that proximal esophageal or hypopharyngeal reflux events are accompanied by distal esophageal reflux and are not secondary to artifact.
Given limitations in patient tolerance to ambulatory catheter-based esophageal pH monitoring systems and difficulties with prolonged measurement periods, an ambulatory wireless capsule-based pH monitoring system has been developed (Fig. 3.3). Upon placement, a standard upper gastrointestinal endoscopy is performed to locate the GEJ. The endoscope is removed, and an introducer with an attached pH capsule probe is inserted. The introducer is advanced, and the capsule probe is placed 6 cm above the GEJ. Recording data are then transmitted to a device worn on the patients’ waist. The wireless system has the advantage of recording 48–96 h of pH data. The capsule pH probe falls off after several days and is passed in the stool .


Fig. 3.3
Endoscopic appearance of the Bravo wireless pH capsule (Given Imaging, Yoqneam, Israel) attached to the esophageal mucosa after deployment
The wireless capsule-based pH monitoring system may be better tolerated, causing less interference with daily activities, and has a higher overall satisfaction rate for patients with GERD. In a randomized study of 50 patients receiving catheter-based or wireless pH monitoring, wireless capsule-based pH monitoring was associated with less nose pain, runny nose, throat pain, throat discomfort, and headache as compared with those with the traditional pH probe, whereas the wireless capsule-based pH monitoring was associated with more chest pain [54]. An additional advantage of wireless pH testing is its greater sensitivity for detecting reflux events due to (1) prolonged monitoring, (2) improved patient compliance, (3) reduced impairment of patients’ daily activity, and (4) decreased likelihood of catheter movement during the study [55]. However, disadvantages of the wireless pH testing system exist including the risk of early capsule detachment. A report from two centers described early detachment in 3/85 patients at 24 h and poor data reception in 3/85 patients at 48 h, where erroneous interpretation of acid exposure time could result due to intragastric pH monitoring [55].
A number of comparison studies have been performed assessing the simultaneous capture of acid reflux using the wireless pH system and catheter-based pH monitoring [56–58]. While strong correlations were observed between acid exposure recorded, a significant offset was noted in the pH values reported by the two systems with the wireless capsule-based pH monitoring system under recording reflux events compared to the catheter-based system [56, 58, 59]. When using a reference standard of swallowed orange juice measured ex vivo, differences in calibration of the catheter-based system due to a thermal calibration correction factor error in the software (which has since been corrected) accounted for differences in offset of pH values and reflux events [59]. Although the number of reflux events could only be partly explained by differences in the thermal correction factor, increased numbers of short reflux events were detected by the catheter-based system likely secondary to the lower sampling rate of the wireless capsule-based pH monitoring system [58] .
The standard duration of recording for esophageal pH monitoring catheter-based systems is 24 h; however, with the introduction of wireless capsule-based pH monitoring, recording times can occur from 48 to 96 h [60]. The routine 48-h data acquired by wireless pH systems can be interpreted using an average of the 48-h collection or using only the 24-h period with the greatest acid exposure. In a study of 85 patients, 39 control subjects and 37 patients with GERD, the use of a definition of abnormal acid exposure as greater than 5.3 % of the study time, using only the 24-h period with the greatest acid exposure had 83.8 % sensitivity for a diagnosis of GERD and 84.5 % specificity compared to 67.5 % sensitivity and 89.7 % specificity when using only the first 24 h of data collection [55].
Monitoring of pH can be performed on or off medical therapy. In monitoring performed without medical therapy, patients are asked to stop PPI therapy for at least one week, histamine H2 blocker therapy for 48 h, and antacid use for 2 h [61]. Whether the study should be performed on or off acid-suppressive therapy depends on what information the clinician desires to gain. A pH study performed off therapy documents whether acid reflux is present at baseline, such as in a patient considering antireflux surgery or in those with atypical GERD symptoms in order to rule out the presence of acid reflux. A study performed in a patient on therapy documents whether continued acid reflux is the cause of refractory symptoms in patients with a poor or incomplete response to medical therapy .
One potential advantage of the ambulatory esophageal monitoring system is the ability to correlate symptoms with reflux episodes. However, even in patients with well-documented GERD, only half of symptomatic events are related to reflux episodes [62]. This observation has led to the development of several symptom scoring systems which can be calculated for individual symptoms attributed to reflux including heartburn , regurgitation , or chest pain [59]. The symptom index (SI) is defined as the percentage of symptom episodes related to reflux events defined by the number of symptoms associated with pH < 4 divided by the total number of symptoms during the study period [63]. Good symptom correlation is considered to be an SI over 50 % for the definition of a positive association. The second scoring system developed includes the symptom sensitivity index (SSI) in which the number of reflux events associated with symptoms is divided by the total number of reflux events during the study period [64]. The symptom-based scoring system with the greatest statistical validity is the SAP, a statistical probability calculation in which the entire pH tracing is separated into 2-min intervals and each segment is evaluated for reflux and symptom episodes; a modified chi-square test is used to calculate the probability that the observed distribution of symptoms and reflux events could have occurred by chance [65]. A SAP value of > 95 % indicates that the probability that the observed association between reflux and symptom occurred by chance is < 5 % [59]. While the SAP provides information on the statistical validity of the reflux and symptom association, the SI and SSI provide information on the strength of the association [66]. Unfortunately, no clinical trials prove that the symptom-based scoring systems predict a cause-and-effect relationship and therefore should be used as complimentary information that links a particular symptom to reflux events without a defined ability to predict response to medical or surgical therapy [59] .
Ambulatory 24-h Bile Monitoring
Duodenogastroesophageal reflux (DGER) refers to regurgitation of duodenal contents through the pylorus into the stomach, with subsequent reflux into the esophagus . DGER may be important because factors other than acid, namely bile and pancreatic enzymes, may play a role in mucosal injury and symptoms in patients with GERD [67–70]. Initially, esophageal pH greater than 7.0 during pH monitoring was considered a marker of such reflux, but alkaline reflux was later proved to be a poor marker for DGER. This finding led to the development of a fiberoptic spectrophotometer (Bilitec 2000, Synectics, Stockholm) that detects DGER in an ambulatory setting independent of pH [71]. This instrument utilizes the optical properties of bilirubin, the most common bile pigment. Bilirubin has a characteristic spectrophotometric absorption band at 450 nm. The basic working principle of this instrument is that absorption near this wavelength implies the presence of bilirubin and, therefore, represents DGER.
As in pH monitoring, data from the bilirubin spectrophotometer are usually measured as percentage of time that bilirubin absorbance is greater 0.14 and can be analyzed separately for total, upright, and supine periods. Percentage of time bilirubin absorbance exceeds 0.14 is commonly chosen as a cutoff because studies show that values lower than this number represent scatter owing to suspended particles and mucus present in the gastric contents [71]. In a study using 20 healthy controls, the 95th percentile values for percentage of total, upright, and supine times that bilirubin exceeded 0.14 were 1.8, 2.2, and 1.6 %, respectively [72]. Several reports have indicated a good correlation between Bilitec fiberoptic spectrophotometer readings and bile acid concentration measured by duodenogastric aspiration studies [71, 73–75]. Validation studies have found that this instrument underestimates bile reflux by at least 30 % in an acidic medium because of bilirubin isomerization with a shift in wavelength absorption [72]. Therefore, the instrument’s measurement of DGER must always be accompanied by simultaneous measurement of esophageal acid exposure by means of prolonged pH monitoring. Furthermore, a variety of substances may result in false-positive readings by this instrument, because it indiscriminately records any substance with an absorption band around 470 nm. This fact necessitates the use of a modified diet to avoid interference and false readings [71, 75]. As the Bilitec spectrophotometer measures reflux of bilirubin and not bile acids or pancreatic enzymes, it must be assumed that the presence of bilirubin in the refluxate is accompanied by other duodenal contents.
Development of this instrument was an important advancement in the assessment of DGER, but its clinical role is limited, and it is no longer available. While initial studies demonstrated the role of bile acids in animal models contributing to mucosal damage, further studies with this device were instrumental in showing that acid reflux and bile reflux occur together, making it difficult to incriminate duodenal contents alone as the cause of damage to the esophagus [70, 72]. Moreover, studies demonstrated a decrease in esophageal bilirubin exposure with omeprazole treatment, thereby further limiting the clinical utility of the assessment of DGER as a contributor to the development of GERD [76].
Impedance
Multichannel intraluminal impedance (MII) is a technology that measures both acid and nonacid reflux of liquid or gas consistency [77]. Impedance , a measure of the total resistance to current flow between adjacent electrodes, is capable of differentiating between liquid and gas refluxate on the basis of their inherent current and resistance properties. By incorporating multiple electrodes along the axial length of the impedance catheter, the proximal extent of the reflux event is able to be captured, as well as the differentiation of antegrade from retrograde refluxate [66]. Catheters commonly employ six or more impedance measuring segments to detect changes along variable lengths of the esophagus with placement standardly 5 cm above the LES (similar to conventional catheter-based pH testing systems) [41]. Current impedance technology has been validated against esophageal manometry studies and is sensitive for the detection of liquid boluses where drops in impedance are observed with boluses as small as 1 and 10 mL [78, 79]. The combined impedance/pH recorder is capable of also measuring characteristics of gastroesophageal reflux that are not detectable by standard ambulatory 24-h esophageal pH monitoring alone. Clinically, this approach may be useful for further evaluation of typical or atypical reflux symptoms refractory to acid suppression therapy, in assessing the role of nonacid and/or nonliquid reflux .
Although there is no doubt that MII–pH measurement is currently the most accurate and detailed method to detect reflux of all kinds, the clinical indications for its use are still evolving, and its role in the management of patients with GERD awaits further definition for two main reasons: (1) the relevance of nonacid reflux in specific clinical settings has to be further discerned and (2) there is a paucity of high-quality blinded, randomized, controlled studies examining the benefit of treating nonacid reflux.
Combining impedance with esophageal pH monitoring allows for identification of all of the parameters measured by standard pH monitoring while adding the total number of reflux events, proximal extent of reflux event, and characterization of the reflux events as acid (pH < 4) or nonacid [80]. Normal values have been established for reflux events in healthy adults, and as with ambulatory esophageal monitoring systems, symptom-scoring systems can be applied in order to correlate symptoms with reflux episodes [81]. Based on impedance values 5 cm above the LES, the median number of reflux episodes in a 24-h period was 30 of which two thirds were acid and one third was weakly acidic [81]. Identification of reflux episodes requires manual visual interpretation as current automated impedance–pH analysis software overestimates the number of reflux episodes [41].
The role of nonacid reflux in the contribution to mucosal damage was reviewed in a prospective study of patients with GERD symptoms and healthy controls that underwent combined impedance/pH monitoring off medical therapy. Among 300 individuals with GERD symptoms, erosive esophagitis was identified in 58, Barrett’s esophagus was identified in 18, and no mucosal damage was seen in 224 patients. Compared to healthy controls, those with erosive esophagitis and NERD had longer distal esophageal acid exposure time and a higher median number of acid reflux episodes. All groups had a similar median number of nonacid reflux episodes suggesting that acid reflux episodes, refluxate volume, and acid clearance are important factors in the pathogenesis of GERD, whereas nonacid reflux contributes less to esophageal mucosal damage [82] .
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






