Fig. 15.1
Complete mucus membrane cylinder at the end of the dissection. (Reproduced from [9], with permission)
Delorme’s procedure is a well-tolerated perineal operation for a full-thickness rectal prolapse. However, prolapse recurrence is common and the reported recurrence rate varies widely (Table 15.1) [8, 11–13]. Delorme’s procedure has low morbidity, and can be performed on unfit and frail elderly patients with significant comorbidities [14]. Good bowel function can be achieved [15], with incontinence reduction and improvement in rectal sensation [16]. Although abdominal operations have a lower recurrence rate, it is feasible to perform Delorme’s procedure again in cases of recurrence, without increased complications. Delorme’s procedure can achieve a favorable and better outcome for internal rectal prolapse treatment by applying stringent patient selection criteria [17, 18]. Pitfalls in performing the procedure relate primarily to associated perineal and colonic conditions. In fact, a data review showed that proximal internal prolapse with rectosacral separation at defecography, preoperative chronic diarrhea, fecal incontinence, weak sphincter tone, previous sphincter injury, and descending perineum (more than 9 cm on straining) were associated with poorer outcomes [18]. Inadequate mucosectomy because of extensive diverticular disease can prohibit effective and complete proximal mucosectomy, leading to early recurrence of the prolapse [19].
15.3 Internal Delorme’s Procedure
A modified Delorme’s procedure has been designed to treat internal rectal prolapse in symptomatic rectal obstructed defecation.
15.3.1 Technique
With the patient in the lithotomy position under epidural anesthesia, a specially designed anoscope is inserted to visualize the distal rectum. The anoscope has the same characteristics of the procedure of prolapse and hemorrhoids (PPH) anoscope, consisting of a tube 30 mm long and 29 mm diameter. It is fixed to the perineum by four stitches. Rectal submucosa is infiltrated with epinephrine and saline solution (1:200,000). The operation starts with a circular incision of the mucosa at 2 cm proximal to the dentate line using monopolar electrocauthery. Mucosal circumferential dissection from the rectal muscle layer proceeds proximally upwards for 80–150 mm, until the surgeon can feel an increased resistance while tractioning on the redundant mucosa. At the level of the resistance the mucosa is divided and the muscle is plicated longitudinally by eight 2.0 absorbable sutures. An interrupted mucomucosal suture completes the endorectal anastomosis (Figs. 15.3–15.6) [20].
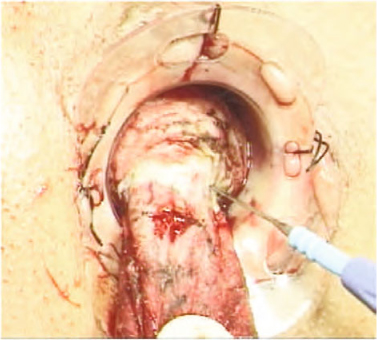
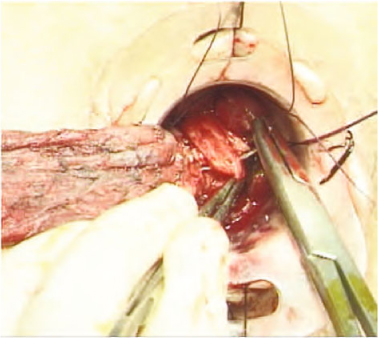
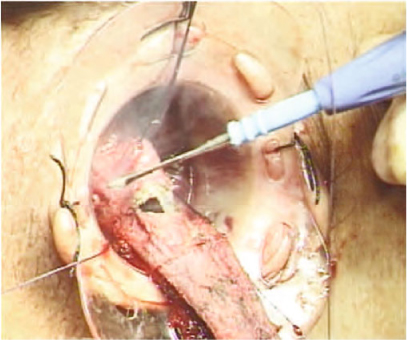
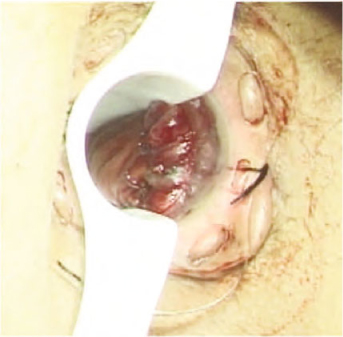
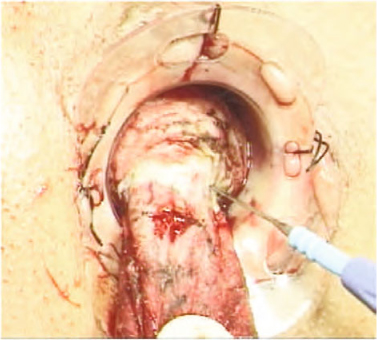
Fig. 15.3
Mucosal circumferential dissection from the rectal muscle layer
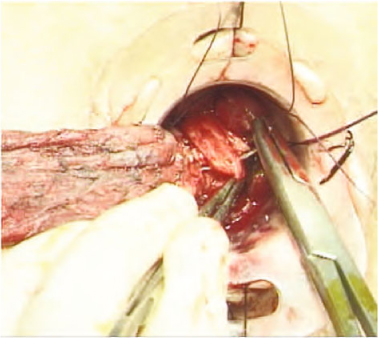
Fig. 15.4
Longitudinal rectal muscle plication
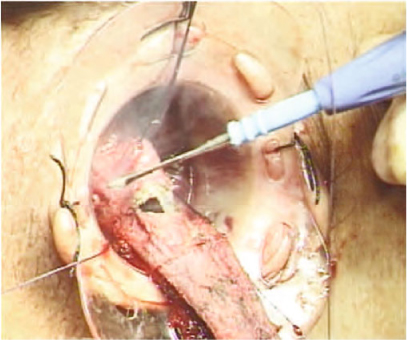
Fig. 15.5
Mucosal section
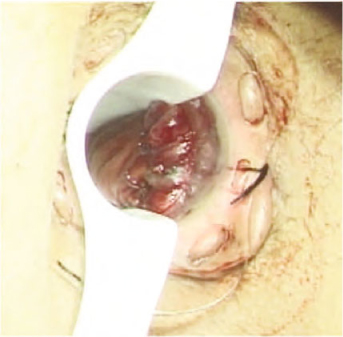
Fig. 15.6
Mucomucosal sutures complete the endorectal anastomosis
In cases of associated weak pelvic floor, or type II or III rectocele, a levatorplasty is performed through a posterior transverse vaginal incision [20].
In our institution, from October 2001 to March 2009, 167 consecutive patients underwent internal Delorme’s procedure, with or without levatorplasty, for symptomatic rectal obstructed defecation associated to rectal intussusception and rectocele. At a mean follow-up of.3.0 ± 1.5 years, fecal urgency changed from 22% to 17.6% (p = 0.754), and tenesmus fell from 53.9% to 17.1% (p < 0.001). The Cleveland Clinic Constipation Score (CCCS) and obstructed defecation syndrome score fell by 50% or more in 82% and 73.7% of cases, respectively. The CCCS did not worsen in patients who remained incontinent, while 45.7% of previously incontinent patients regained normal continence. The Patient Assessment of Constipation Quality of Life (PAC-QoL) showed a decline of the overall score preoperatively to postoperatively, with a reduction of anxiety/depression, and physical and psychological discomfort (p < 0.001). Seventeen patients (10.2%) developed a postoperative complication including anal fissure (4.2%), proctalgia (3%), suture line dehiscence with stenosis (1.8%), and Clostridium difficile colitis (1.2%) [20]. The recurrence rate of 5.4% is comparable with previously published large series of Delorme’s procedure [21, 22]. It is also comparable with the recurrence rate reported in stapled transanal rectal resection (STARR) and TRANSTARR procedure studies [23, 24]. Postoperative urgency decrease in internal Delorme’s procedure, although not statistically significant, is a crucial outcome compared with the potential complication and high urgency rate recorded after the STARR procedure [24–26]. Therefore compared with other treatments, which are discussed in other chapters, internal Delorme’s procedure can be considered a cheap, effective, and safe procedure for rectal obstructed defecation that is caused by rectal intussusceptions, with or without rectocele.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







