Caring for patients with constipation and pelvic outlet obstruction can be challenging, requiring skill, patience, and empathy on the part of the medical professional. The mainstay of treatment is behavioral with surgery reserved for a select group of patients. The evaluation, diagnostic, and treatment modalities of both constipation and pelvic outlet with a focus on current advancements and technology are explored in depth.
Key points
- •
The diagnosis of constipation is confirmed using the Rome III criteria.
- •
In addition to history and physical, it is prudent to obtain a colonoscopy in patients with new onset constipation. Further testing may be deferred until a trial of lifestyle modifications and medical therapy fails.
- •
Surgery is reserved for select patients with colonic inertia that fail medical management and have no evidence of globalized intestinal dysmotility.
- •
The first-line treatment for patients with pelvic dyssynergy is biofeedback.
- •
Rectoceles are present in up to 81% of asymptomatic women.
- •
Large rectoceles that require digital splinting may benefit from repair.
- •
A stoma may benefit select patients that fail other treatment modalities for constipation.
Introduction
Constipation is one of the most common medical complaints among Americans, affecting up to 25% of the population. The cause of constipation is oftentimes multidisciplinary, including dietary habits, genetics, psychosocial issues, medications, medical illness, and primary diseases of the colon and rectum. A clear understanding of the available diagnostic modalities and management strategies is imperative for health care providers from any discipline who will undoubtedly treat patients with constipation.
Introduction
Constipation is one of the most common medical complaints among Americans, affecting up to 25% of the population. The cause of constipation is oftentimes multidisciplinary, including dietary habits, genetics, psychosocial issues, medications, medical illness, and primary diseases of the colon and rectum. A clear understanding of the available diagnostic modalities and management strategies is imperative for health care providers from any discipline who will undoubtedly treat patients with constipation.
Definition
The complaint of constipation is quite subjective, making it difficult to reliably define. A team of international experts published diagnostic criteria (Rome III) based on the presence of the criteria listed in Box 1 for at least 3 months with onset of symptoms 6 months before diagnosis.
- •
Must include at least 2 of the following
- ○
Fewer than 3 stools per week
- ○
Hard stools in at least 25% of defecations
- ○
Manual maneuvers to facilitate at least 25% of defecations (eg, support of pelvic floor or digital stimulation)
- ○
Straining during at least 25% of defecations
- ○
Sensation of incomplete evacuation for at least 25% of defecations
- ○
Sensation of anorectal blockage for at least 25% of defecations
- ○
- •
Loose stools rarely present without the use of laxatives
- •
Insufficient criteria for irritable bowel syndrome
Symptoms must be present for at least 3 months with onset of symptoms 6 months before diagnosis.
Cause and pathology
Constipation can result from numerous conditions and medications. Perhaps the most common contributing factor to constipation is dietary. The western diet consists primarily of processed grains and, as such, is devoid of adequate amounts of fiber. Fiber intake correlates with stool bulk, which is important for colonic distension, stimulation of normal peristalsis, and efficient propulsion of stools. Furthermore, medical illnesses ranging from diabetes and hypothyroidism to neurologic illness, psychiatric disease, rheumatologic conditions, and anything leading to immobilization contributes to constipation. Finally, numerous medications lead to constipation, ranging from antihypertensives to antidepressants, iron supplements, and opioids. Mechanical causes of constipation must also be carefully considered including colon stricture, malignancy, and endometriosis. Idiopathic chronic constipation can be divided into 3 subtypes.
Constipation subtypes
- 1.
Motility disorders (11% of patients): May be isolated to the colon (colonic inertia) but can affect the entire bowel in up to 20% of patients with colonic inertia; often associated with constipation since childhood and laxative dependence
- 2.
Irritable bowel syndrome (71% of patients): Frequently associated with abdominal pain that is relieved by defecation and irregular bowel habits; a diagnosis of exclusion
- 3.
Pelvic outlet obstruction (13%–50%): Also known as obstructed defecation syndrome, anismus, and pelvic dyssynergy; characterized by sensation of incomplete evacuation, prolonged straining, and need for digital manipulation.
Initial evaluation
History and Physical
The factors listed in Box 2 should be taken as part of a full history during evaluation of the patient with constipation. Although the physical examination is oftentimes unremarkable, it does remain an important part of the evaluation. Abdominal examination may reveal distension and a palpable mass as the result of hardened stool in extreme cases. Close inspection of the pelvic floor is also important. With the patient in the left lateral decubitus position or the prone jackknife position on a Ritter table, a rectal examination should be performed to evaluate for fecal impaction, tenderness, or masses. The patient should then be asked to strain. The examiner should look for bulging into the vaginal introitus indicating a rectocele, full-thickness rectal prolapse, or bulging of the perineum below the ischial tuberosities, which indicates perineal descent syndrome. Finally, the puborectalis muscle should be palpated with the examiner’s finger in the anal canal by hooking the examining finger posteriorly over the coccyx and asking the patient to strain. Under normal conditions the anal canal should relax. However, in patients with anismus or dyssynergia, there can be an inability to relax or paradoxic puborectalis contraction when the patient strains. The sensitivity and specificity of such examination was found to be 75% and 87%, respectively, in one study.
History
- •
Stool size, frequency, consistency
- •
Characterize evacuation
- •
Age of onset
- •
Diet and exercise habits
- •
Medical and surgical history
- •
Medications
- •
Psychiatric illness, sexual abuse
- •
Other pelvic floor symptoms (eg, urinary dysfunction, prolapse)
Physical examination
- •
Abdominal examination: distension, palpation of mass/hardened stool
- •
Pelvic floor evaluation: vaginal, perineal, and rectal examination to evaluate for rectocele, full-thickness rectal prolapse, bulging of perineum
Testing
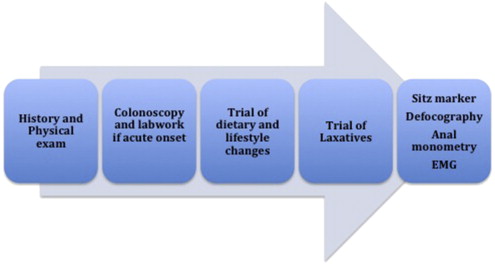
It is prudent to obtain a colonoscopy in patients with constipation to rule out an underlying malignancy. In addition, a complete blood cell count, thyroid-stimulating hormone, and chemistry panel should be obtained in patients with acute onset constipation or signs and symptoms worrisome for malignancy. Further testing may be deferred until a trial of lifestyle modifications including fiber supplementation, hydration, and exercise along with the use of laxatives fails to resolve the patient’s symptoms ( Fig. 1 ). Commonly used testing methods are described in Table 1 .
| Test | Description | Evaluates | Normal | Abnormal |
|---|---|---|---|---|
| Manometry | Uses pressure transducers to measure anal canal pressures and rectoanal inhibitory reflex (RIR) | Rectal sensation and compliance, reflexive relaxation of internal anal sphincter | Sphincter relaxes with straining, pressure in anal canal decreases RIR, rectal distension results in relaxation of internal anal sphincter |
|
| Colon transit study | Patient ingests capsule of 24 radiopaque markers, radiograph on consecutive days | Colonic motility | 80% of markers passed out or to rectum by day 5 |
|
| Defecography | 150 mL of barium paste inserted into rectum and anal canal; patient then asked to evacuate paste on specially designed radiograph table/commode | Pelvic floor relaxation—anorectal angle (ARA), perineal descent, and puborectalis length | Resting ARA: 70–140° |
|
| Balloon expulsion | 50 mL water-filled balloon placed in rectum and evacuated | Functional ability | Pass the balloon | Failure to pass balloon suggests dyssynergy or anismus |
| Dynamic MRI | Various protocols described, not standardized | Pelvic floor anatomy | Similar to defecography | Similar to defecography |
| Electromyography | Electrodes placed in anal sphincter and electrical activity of puborectalis evaluated during evacuation | Puborectalis | Puborectalis relaxes during straining with decreased electrical activity | Dyssynergy, increased electrical activity during straining |
Treatment
Medical Treatment
Medical treatment begins with avoidance of constipating medications, increasing fiber intake to 20 to 25 g per day with adequate hydration, and regular exercise. A full discussion of the medical treatment of constipation is beyond the scope of this article. However, psyllium, stool softeners, and stimulant and osmotic laxatives are commonly used in the treatment of constipation. Osmotic laxatives such as polyethylene glycol and lactulose seem to be the most effective in the treatment of constipation based on the literature. Other agents include lubiprostone, misoprostol, and colchicine, which have been used in patients with severe constipation with limited success.
Colonic Inertia
Most patients are women and complaints may include bloating, obstipation, and abdominal pain. Patients with colonic inertia have typically suffered with constipation since childhood, although it is not uncommon for women to present after pelvic surgery or childbirth. The diagnosis is confirmed with a sitz marker study; however, pelvic outlet obstruction should also be ruled out.
Surgical options
Surgical options for colonic inertia include total abdominal colectomy with ileorectal anastomosis, subtotal colectomy with ileosigmoid anastomosis, subtotal colectomy with cecorectal anastomosis, and segmental colectomy. The goal with all these procedures is to remove enough colon to relieve the constipation without inadvertently leaving the patient with disabling diarrhea and incontinence. As such, segmental colectomy and subtotal colectomy are appealing. There are no prospective studies comparing these methodologies, only small case series. Lundin and colleagues demonstrated that 23 of 28 patients undergoing segmental colectomy were pleased with their outcome. Similarly, Marchesi and colleagues demonstrated good functional results with open and laparoscopic subtotal colectomy with cecorectal anastmososis. Niether of these procedures is widely performed, however, due to the risk of recurrent or persistent constipation and the difficulty in identifying appropriate patients based on diagnostic testing. In addition, there have been reports of restorative proctocolectomy in the setting of chronic constipation. However, this should only be considered in a highly select and motivated patient population and long-term functional results are lacking.
Currently, total abdominal colectomy with ileorectal anastomosis (either open or laparoscopic) is the most widely performed procedure for colonic inertia and has demonstrated adequate long-term results. Any surgical procedure must be performed in a highly selective population:
- •
Severe medically refractory constipation
- •
No evidence of secondary or structural causes for constipation
- •
Slow transit on colonic motility study (ie, sitz marker test)
- •
Normal gastric and small bowel motility (whole gut transit scintigraphy, gastric emptying study, or small bowel follow through)
- •
Ability to relax pelvic floor musculature
- •
Understands surgical risks and long-term expectations
The patients should be fully evaluated to exclude secondary causes such as hypothyroidism. Colonoscopy should be performed to rule out a structural abnormality. Patients should also be evaluated with whole gut transit scintigraphy, a gastric emptying study, or small bowel follow through to assess for the presence of a diffuse gastrointestinal dysmotility disorder, which can accompany colonic inertia in 30% of patients. Total colectomy is generally not beneficial in patients with globalized dysmotility. A validated constipation score should be obtained to help categorize the type of incontinence and to monitor progress after therapy.
Defecography should be performed to evaluate for the presence of pelvic outlet obstruction, which can affect up to 20% of patients with colonic inertia and complicates management. Increasingly, more surgeons offer total colectomy after preoperative biofeedback with demonstration of pelvic floor relaxation. Previously, the results of colectomy in the setting of colonic inertia and combined pelvic outlet disorder were disappointing. However, more recent reports indicate similar patient satisfaction scores on follow-up surveys administered to patients with and without obstructed defecation syndrome (ODS) following colectomy for slow transit constipation.
Finally, the patients should obviously be counseled extensively about the surgical risks of the operation but also must be given realistic expectations. Although total colectomy is highly effective at improving the daily number of bowel movements in patients with colonic inertia, the effect on the patient’s overall quality of life isless well defined.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







