Kumar [24]
Perez [16]
Lezoche [15]
Bignell [20]
Tsai [28]
Allaix [25]
Bach [18]
Guerrieri [8]
Buess [14]
Patients ( n)
325
36
135
262
269
300
424
588
326
Indication:( cancer, benign, both)
Both
Both
Cancer
Both
Both
Both
Cancer
Both
Both
Complications ( %)
10.5
44
10.4
13
21
7.7
14.9
11.4
16
Mortality ( %)
0.3
0
0
0.8
0
0
1.4
0
0
Septic complications ( n)
10
20
10
8
26
11
18
54
NR
Dehiscence
0
17
9
0
3
5
0
36
3
Abscess/pelvic sepsis
2
–
1
7
–
–
5
–
–
Peritoneal entry
9
–
–
–
20
13
9
16
–
Missed peritoneal entry
1
1
–
1
–
1
1
–
–
Fistula
1
2
–
0
–
5
2
2
2
Fever UO
–
–
–
–
2
–
–
–
–
Table 40.2
Select TAMIS (transanal minimally invasive surgery) studies
Albert [10] | Lee [36] | Bridoux [37] | Barendse [38] | Lim [39] | |
|---|---|---|---|---|---|
Patients ( n) | 50 | 25 | 14 | 11a | 16 |
Indication: ( cancer, benign, both) | Both | Both | Both | Both | Both |
Complications ( %) | 8 | 4 | 21 | 7.7 | 0 |
Mortality ( %) | 0 | 0 | 0 | 0 | 0 |
Septic complications ( n) | 1 | 0 | 1 | 0 | 0 |
Dehiscence | – | – | – | – | – |
Abscess | – | – | – | – | – |
Peritoneal entry | 1 | – | 0 | – | – |
Missed peritoneal entry | – | – | – | – | – |
Fever UO | – | – | 1 | – | – |
Postoperative Fever
A high temperature in the immediate postoperative period is common. However, in most patients this is temporary and is not necessarily followed by the development of other septic complications. The cause of early postoperative fever is unknown, but may be related to transient bacterial translocation immediately after the procedure.
Wound Dehiscence
The need for closure of the rectal wound during LE in the extraperitoneal portion of the rectum is controversial. The potential advantages of wound closure include securing hemostasis and reducing fecal contamination. The chief disadvantage is the potential creation of a dead space that may become a perfect environment for the development of septic complications. The enhanced visualization and new instrumentation provided by TEMS, TEO, and TAMIS platforms facilitate suturing and knot-tying or clipping. As a consequence, rectal wounds are almost always closed watertight after TEM or TAMIS excision. The closure can be done as a running suture, which is facilitated by clips instead of knot-tying, or with interrupted sutures (Fig. 40.1).
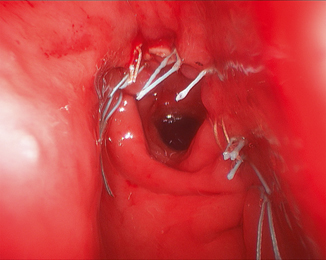
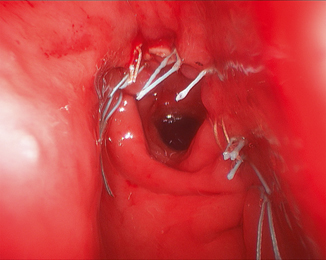
Fig. 40.1
Rectal wounds are almost always closed watertight after TEM or TAMIS excision. The closure can be done as a running suture, which is facilitated by clips instead of knot-tying, or with interrupted sutures
The reported rate of wound dehiscence ranges from 0 to 15 % and can lead to complications such as stenosis and fistula [16, 18, 19]. The true rate of wound dehiscence is probably higher because only symptomatic patients undergo rectal examination in the early postoperative period. Wounds located closer to the dentate line, particularly in patients who have received neoadjuvant chemoradiation, are more likely to dehisce [7, 17]. Table 40.3 describes the treatment for wound dehiscences in each of the major TEM and TAMIS studies discussed above. In the study by Perez et al., 9 of 11 readmissions within 30 days of TEM excision were due to severe pain secondary to wound dehiscence [16]. Furthermore, all patients with late complications had been diagnosed with early wound dehiscence. Lezoche et al. described partially dehisced suture lines in 9 of 135 patients (6.7 %), all of which were resolved with antibiotic enemas and “occasionally by fasting and parenteral nutrition” [15].
Table 40.3
Outcomes after wound dehiscence/failure of closure
Kumar [24] | Perez [16] | Lezoche [15] | Tsai [28] | Allaix [25] | Guerrieri [26] | |
|---|---|---|---|---|---|---|
# Cases | 1 | 17 | 9 | 4 | 5 | 36 |
Management | ||||||
Non-operative | 0 | 16 | 9 | 2 | 0 | 35 |
Operative | 1 | 1 | 0 | 2a | 2 | 1 |
Transanal | – | – | – | – | NR | 1 |
Abdominal | 1 | 1 | – | 2 | NR | – |
Ostomy | 1 | 1 | – | – | NR | – |
Radical resection | – | – | – | – | NR | – |
Rectal Pain
Persistent anal and rectal pain is a common complaint, particularly in patients with low rectal cancer treated with chemoradiation. In the ACOSOG Z6041 trial investigating the treatment of T2N0 rectal cancer with preoperative chemoradiation and LE, 8 % of patients complained of grade 3 anal pain [7]. This has been attributed to the dehiscence of a wound close to the anal canal, which, in contrast to the rectal wall, has rich somatic pain innervations. The pain often persists for several weeks until the dehisced wound heals [16]. A diverting temporary ostomy should be considered in patients with very low rectal tumors who have undergone radiation. A diverting temporary ostomy should be considered even in those who have not had radiation, depending on the size of the lesion and the amount of tension expected after closure. Some surgeons have also adopted the routine use of antibiotics for an extended period following excision of very distal tumors [20].
Peritoneal Perforation
Peritoneal perforation during TEM, TEO, and TAMIS occurs at a median rate of 4.8 %, although this ranges from 0 to 32 % in the literature [21]. During excision of anterior tumors, this rate may be even higher, especially in those located above 9 cm, where entry into the peritoneum should be expected [19, 22]. The consequences range from postoperative pain or distention to intraabdominal sepsis. On a practical note, peritoneal perforation compromises adequate visualization by evacuating the necessary pneumorectum for TEM, TAMIS, and TEO procedures. The most feared complication is peritonitis caused by the seeding of the abdominal cavity with rectal luminal content. There, were early concerns regarding the possibility of disseminating cancer cells into the peritoneal cavity after peritoneal perforation. As outcomes after TEM, TAMIS, and TEO continue to be studied, there is currently no evidence that peritoneal perforation compromises oncologic outcome [21]. In a multinational study specifically examining the effect of peritoneal perforation on outcomes in 888 patients, Baatrup et al. demonstrated no increase in long-term oncologic failure [23].
Entry into the peritoneal cavity is typically recognized during surgery by sudden loss of, or difficulty maintaining, pneumorectum. The overall risk of peritonitis is low, provided that the perforation is recognized intraoperatively and the peritoneal defect and rectal wound are securely closed. This can typically be accomplished transanally, though a transabdominal repair, either open or laparoscopic, may be necessary if the peritoneal or rectal wound closure is suboptimal.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








