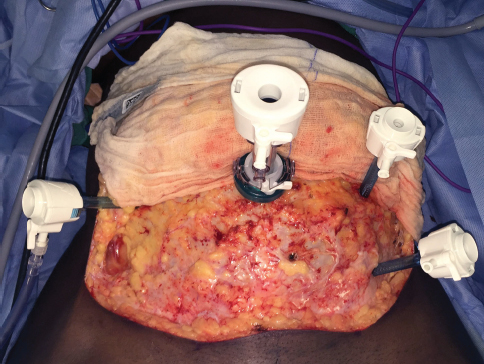
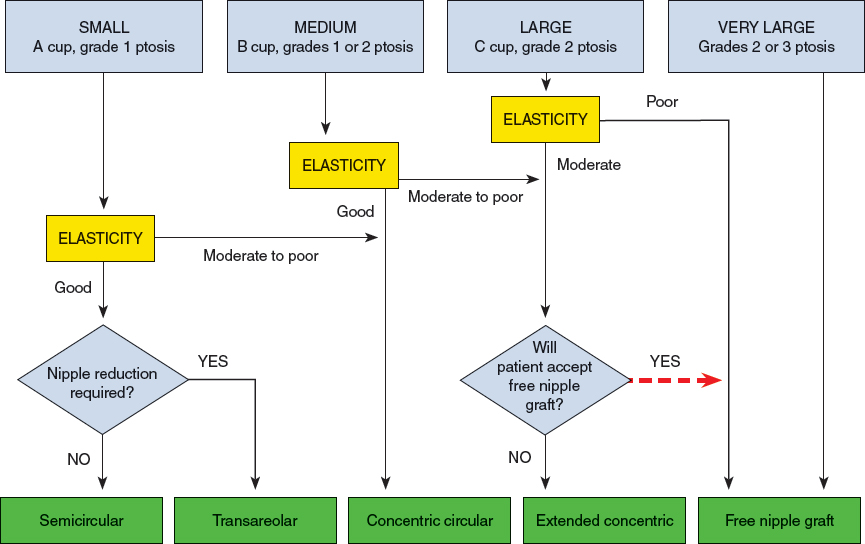
CHAPTER 4 Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People (SOC) published by the World Professional Association for Transgender Health (WPATH) are the professional guidelines that establish recommendations for performing gender affirmation surgery (GAS) on transgender patients.1 The SOC are specific in certain guidelines, such as recommending that all patients undergo at least 1 year of hormone therapy before gonadectomy to introduce a period of reversible changes in appearance before the patient undergoes irreversible surgery. However, they are notably more vague in others, because WPATH acknowledges that therapeutic and surgical goals are unique to each patient. Box 4-1 lists the WPATH SOC for breast/chest surgery and hysterectomy/oophorectomy.1 Notably, the SOC do not specify the order in which transition surgeries should occur. The number and order can vary, depending on the patient’s unique needs and how he or she chooses to coordinate a treatment plan with the surgical teams. Breast/chest surgery can be performed independently, which may be ideal for a person wishing to keep his or her reproductive organs intact. However, many patients choose to undergo gonadectomy and genital reconstructive surgery, in addition to breast/chest surgery. Specifically, for the female-to-male (FTM) patient desiring chest reconstruction, gonadectomy, and subsequent GAS, it is often beneficial to combine chest reconstruction with a total laparoscopic hysterectomy and bilateral salpingo-oophorectomy (TLH/BSO) into one procedure. Breast/Chest Surgery* 1. One referral from a mental health professional with experience in the care of transgender patients 2. Persistent, well-documented gender dysphoria for at least 1 year 3. Capacity to make a fully informed decision and to consent for treatment 4. Age of majority in a given country (if younger, follow the SOC for children and adolescents) 5. If significant medical or mental health concerns are present, they must be reasonably well controlled Hysterectomy/Oophorectomy 1. Two referrals from mental health professionals with experience in the care of transgender patients 2. Persistent, well-documented gender dysphoria for at least 2 years 3. Capacity to make a fully informed decision and to give consent for treatment 4. Age of majority in a given country (if younger, follow the SOC for children and adolescents) 5. If significant medical or mental health concerns are present, they must be well controlled 6. Twelve continuous months of hormone therapy as appropriate to the patient’s gender goals (unless hormones are not clinically indicated for the individual) * Hormone therapy is not a prerequisite. Performing these surgeries together—the former by plastic surgeons and the latter by gynecologists—can be accomplished safely and efficiently with few or no complications and can confer great benefit to the patient.2,3 The combined procedure can result in fewer total trips to the operating room, less time away from work, reduced hospital costs, and the psychological benefits of removing multiple components of the anatomy that potentiate gender dysphoria. Although the timing of surgery should always be tailored to the individual needs of the patient, combining these surgeries can be presented as a safe option to FTM patients. Another area in which the SOC are nonspecific is in the treatment of adolescents. Although they recommend that irreversible surgery should be withheld until the age of consent, they acknowledge that this decision should ultimately be left to the patient, his or her parents, and the physicians. Therefore, under the appropriate circumstances, irreversible surgery may be performed on adolescents. Existing literature supports the assertion that GAS in a carefully selected adolescent population is beneficial for alleviating gender dysphoria and contributing to a successful gender transition.4,5 Transgender patients with well-documented diagnoses of gender dysphoria who desire irreversible GAS procedures are candidates for combined chest reconstruction and TLH/BSO. The indication for surgery is generally made first by a psychiatrist or psychotherapist, who provides the patient with a referral letter containing the diagnosis of gender dysphoria. Patients should meet all the criteria outlined by the WPATH SOC to be considered candidates for surgery. Exposure to long-term testosterone therapy may also present additional indications for hysterectomy. Long-term testosterone therapy may confer increased risk of malignancy of the upper female genital tract, although the data are somewhat limited and conflicting.6,7 In addition, some evidence suggests that testosterone exposure increases the risk of abnormal uterine bleeding in certain individuals, which can also be an indication for hysterectomy.8,9 There are no absolute contraindications to combined chest reconstruction and TLH/BSO. However, careful counseling regarding options for fertility preservation must be performed by a professional (either personally or by referral) who is well versed in the available options before proceeding with surgery. The patient should be made aware of the option to preserve the uterus and use assisted reproductive technologies to become pregnant. The patient may also elect to undergo oocyte harvesting and cryopreservation before TLH/BSO. The preserved oocyte can then be used for in vitro fertilization and implanted in the uterus of a female partner or surrogate. The patient must be made aware of the fact that he will need to discontinue testosterone therapy during preparation and performance of these procedures. If he elects to attempt to carry a pregnancy, testosterone must also be discontinued for the entire gestation. Finally, cost considerations must be discussed. The expenses associated with assisted reproductive technology are generally not covered by insurers and can carry a substantial cost. Both the plastic surgeon and gynecologist who will perform the combined procedures should evaluate the patient before surgery. Respective evaluations can take place separately and can proceed in the standard fashion for presurgical physical examination for mastectomy and TLH/BSO by each physician. Presurgical evaluation for hysterectomy/oophorectomy should also include a discussion of the patient’s future plans for genital reassignment surgery (GRS) and the desire for vaginectomy, which may be performed at the time of hysterectomy or GRS. If the patient desires vaginectomy at the time of hysterectomy and the surgeon is comfortable performing this procedure, it may be incorporated into the surgical plans. If the patient desires GRS, the patient can opt to undergo vaginectomy during either surgery. However, vaginectomy at the time of GRS may be preferred, because vaginal mucosa is often used for urethral lengthening during neophallus creation. It is well known that certain factors affect wound healing and cosmetic outcomes. Surgical candidates who smoke and/or are overweight should be counseled to refrain from smoking and to achieve a healthy BMI before surgery.10,11 Conditions such as diabetes that affect wound healing should also be appropriately controlled before surgery.12 In the perioperative period, the patient’s hormone therapy is frequently discontinued, often at least 2 weeks before surgery. Supraphysiologic testosterone levels can lead to elevated serum estrogen levels, which potentially increase the risk for thromboembolic events.13 However, the incidence of thromboembolic events in transgender individuals is low.14 Therefore the decision to withhold hormone therapy before surgery is individualized based on the presentation of the patient and should be a decision involving a discussion among the surgical team, endocrinologist, and patient. Perioperative thromboembolic prophylaxis by medical treatment, such as heparin or enoxaparin, and mechanical means, such as compression stockings, sequential compression devices, and early ambulation, should also be considered. Performing two surgeries simultaneously in the same operative setting also raises concern about the increased risk of infection. Administration of antibiotic prophylaxis with coverage of both gram-negative and gram-positive organisms and anaerobes is advised. The two surgeries do not need to be performed in any particular sequence. Both TLH/BSO preceding chest reconstruction and the reverse order result in similarly successful outcomes.3 A total hysterectomy involves the complete removal of the uterus and cervix, and in transgender patients, it is generally performed in combination with a salpingo-oophorectomy, which is the removal of the ovaries and fallopian tubes. For patients who do not have another contraindication for laparoscopy, TLH is recommended. It is aesthetically pleasing because it avoids creating a lower abdominal scar and produces the best results with the fewest complications.15,16 In addition, it can potentially decrease postoperative pain and can preserve structures that are generally necessary for subsequent phalloplasty, such as the inferior epigastric vessels and rectus muscles.17 Vaginal hysterectomy, although minimally invasive, can be a challenge in transgender men, because they are frequently nulliparous and may have significant atrophy of the vaginal canal resulting from a combination of the effects of testosterone and not having receptive vaginal intercourse.18 In some patients vaginal hysterectomy may be appropriate. However, because the laparoscopic technique is more commonly performed in transgender patients, it will be described here. Fig. 4-1 TLH port site placement for an approach that uses a periumbilical port and three additional trochars. The patient underwent concomitant panniculectomy. The procedure starts by placing the patient under general endotracheal anesthesia followed by positioning him in dorsal lithotomy. After skin and vaginal disinfection, the bladder is drained by Foley catheterization. A uterine manipulator is inserted vaginally with a cup around the cervix. It can be secured to the cervix by a single suture through the ring and secured with a hemostat. Accessing the abdomen and establishing pneumoperitoneum can be accomplished by the surgeon’s preferred technique (open, direct entry, or Veress needle), taking into consideration any patient factors that could affect its safety. Pneumoperitoneum with intraabdominal pressure at 12 to 15 mm Hg is recommended to maintain adequate visualization of the pelvic organs without having an adverse impact on the need for positive-pressure ventilation. In some techniques for TLH/BSO a periumbilical port and three trocars are used (Fig. 4-1). In another technique, two incisions are placed lateral to the epigastric vessels for the 5 mm trocars. In either situation, the sites can be adjusted according to uterine size and the presence of other pathology.3,17,19 Abdominal and/or adnexal adhesions should be removed first if they are present. The round ligaments and infundibulopelvic ligaments are coagulated and cut, and the broad ligaments are opened to identify the ureters and then cut to the lateral edges of the uterus. The uterine arteries are then skeletonized. The surgeon should mobilize the inferior leaf of the peritoneum caudally and laterally to move the ureters well away from the area where the uterine arteries will be divided. After this, the vesicouterine peritoneum overlying the cervix is dissected and mobilized inferiorly. The cup that is placed around the cervix in the vagina can be pressed cephalad to aid this dissection and prevent injury to the bladder and ureters during dissection. The surgeon should carefully mobilize the bladder inferiorly only to the extent necessary to eventually amputate the cervix and uterus from the vagina. Dissecting too far inferiorly will increase the risk of bleeding and injury to the ureters. After adequate mobilization of the bladder is achieved, the uterine vessels can be coagulated and cut at the level where the incision will be made in the vaginal cuff. Afterward, the uterus and cervix must be separated from the vaginal apex by pushing cephalad with the uterine manipulator and using the cup as a backboard. Monopolar or harmonic energy devices can be used to amputate the specimen. The uterus can be pulled through the vagina if it fits, and it can remain there to maintain pneumoperitoneum during suturing. Alternatively, it can be fully removed, and a glove with two 4 × 4 sponges can be used in its place. If the uterus is too large to fit through the vagina, which is unlikely in an FTM patient, it can be morcellated transvaginally. The vaginal cuff can be closed with absorbable sutures in an interrupted fashion. The surgeon should include the vaginal mucosa and pubocervical and rectovaginal fascia. The uterosacral ligaments may be included in the closure of the apices. Finally, all instruments and ports are removed and the sites are closed. Chest reconstruction surgery is regarded as a safe and beneficial option for the FTM patient to convey a more masculine appearance.20,21 In addition, quality of life has been found to be higher in individuals who have undergone chest reconstruction.21,22 Subcutaneous mastectomy (SCM) is the technique best suited for FTM transgender patients, because it produces the aesthetic appearance of a male chest by removing breast tissue and excess skin, reducing and repositioning the nipple and areola, and obliterating the inframammary fold, the goal of which is to minimize chest scars. Liposuction alone cannot address the excess skin or allow complete redraping of the inframammary fold or repositioning of the nipple-areola complex (NAC). Although many techniques for subcutaneous mastectomy have been described, the choice should ultimately be based on the surgeon’s experience. However, the amount of skin excess rather than breast volume is the main determinant of technique. Skin elasticity is also an important factor and can be problematic for the transgender population, which often engages in “breast binding.”20,23–25 Monstrey et al26 described an algorithm of five different techniques to perform an aesthetically satisfactory SCM (Fig. 4-2). Preoperative parameters to be evaluated include breast volume, the degree of excess skin, NAC size and position, and skin elasticity. Regardless of the technique, subcutaneous fat should be preserved when dissecting the glandular tissues from the flaps to ensure thick flaps that produce a pleasing contour. The skin flaps should not be as thin as those used in oncologic mastectomies, and the surgeon must be aware of the central aspect of the flap to avoid “hollowing out.” Liposuction can be used as an adjunctive procedure to aid in contouring the lateral chest wall or to improve symmetry at the end of the procedure. The semicircular technique involves the smallest incision, usually along the inferior aspect of the areola. It is most useful for the treatment of individuals with smaller breasts and elastic skin. This technique is familiar to many surgeons, because it is frequently advocated in the excisional treatment of gynecomastia.27 A sufficient amount of glandular tissue should be left in situ beneath the NAC to avoid a depression. The advantage of this technique is the well-hidden scar. However, this incision provides the least visualization of the underlying tissue and creates a technical challenge. Furthermore, it does not allow resection of excess skin or alterations in the NAC location or size.
Combined Hysterectomy, Oophorectomy, and Chest Reconstruction in Female-to-Male Transgender Patients
Key Points
 For female-to-male (FTM) patients who desire the removal of breasts and female reproductive organs for the cessation of endogenous production of feminizing gonadal hormones, an excellent option is a combined chest reconstruction and total laparoscopic hysterectomy (TLH) with bilateral salpingo-oophorectomy (BSO).
For female-to-male (FTM) patients who desire the removal of breasts and female reproductive organs for the cessation of endogenous production of feminizing gonadal hormones, an excellent option is a combined chest reconstruction and total laparoscopic hysterectomy (TLH) with bilateral salpingo-oophorectomy (BSO).
 Combined TLH/BSO and chest reconstruction is safe and efficacious and reduces the total number of trips to the operating room that a transgender patient must undergo to alleviate his gender dysphoria.
Combined TLH/BSO and chest reconstruction is safe and efficacious and reduces the total number of trips to the operating room that a transgender patient must undergo to alleviate his gender dysphoria.
 Laparoscopic technique is recommended for the hysterectomy and oophorectomy in transgender male patients.
Laparoscopic technique is recommended for the hysterectomy and oophorectomy in transgender male patients.
 Five techniques for aesthetically pleasing subcutaneous mastectomy have been described. The appropriate technique should be selected based on breast size and the degree of ptosis.
Five techniques for aesthetically pleasing subcutaneous mastectomy have been described. The appropriate technique should be selected based on breast size and the degree of ptosis.
 Combined TLH/BSO has been shown to be successful in gender dysphoric adolescents and should be considered a viable option in this age group if these surgeries are indicated to help the patient to achieve his gender expression goals.
Combined TLH/BSO has been shown to be successful in gender dysphoric adolescents and should be considered a viable option in this age group if these surgeries are indicated to help the patient to achieve his gender expression goals.
Indications and Contraindications
Patient Evaluation
Preoperative Management
Surgical Technique: Total Laparoscopic Hysterectomy and Bilateral Salpingo-oophorectomy
Surgical Technique: Chest Reconstruction
Abdominal Key
Fastest Abdominal Insight Engine