Chapter 17 COLORECTAL CANCER
RISK FACTORS
Environmental and genetic factors can increase the likelihood of developing colorectal cancer (CRC) (Table 17.1). Although inherited susceptibility most strikingly increases the risk, the majority of CRCs are sporadic. Age is a very important risk factor. It rarely occurs before the age of 40, and the incidence begins to increase significantly in the sixth decade, with the highest rate between 65 and 75 years. The incidence rate is higher in industrialised regions, higher in African American than in whites, and it is nearly equal for males and females (M:F ratio1.3:1.0 for rectal tumours).
TABLE 17.1 Risk factors for colorectal cancer (CRC)
| Risk factor | Examples | Risk |
|---|---|---|
| Genetic disorders | Familial adenomatous polyposis | I |
| Hereditary non-polyposis colorectal cancer | I | |
| Peutz-Jeghers syndrome | I | |
| Hyperplastic polyposis | I | |
| Cowden’s syndrome | I | |
| Juvenile polyposis syndrome | I | |
| Personal history of CRC or adenoma | I | |
| Family history of CRC or adenoma | I | |
| Inflammatory bowel disease | Ulcerative colitis, Crohn’s disease | I |
| Medications | NSAIDs, aspirin, calcium, vitamin D, statins, hormone replacement therapy (in postmenopausal women) | D |
| Endocrine disorders | Diabetes mellitus | I |
| Insulin resistance | I | |
| Acromegaly | I | |
| Obesity | I | |
| Gastrin | I | |
| Surgical interventions | Cholecystectomy | I |
| Ureterocolic anastomoses | I | |
| Environmental factors | Smoking | I |
| Moderate physical activity | D | |
| Healthy diet (low calorie, rich in fruits and vegetables with low animal products) | D | |
| Alcohol (moderate and high amount) | I |
D = decrease risk for CRC; I = increase risk for CRC; NSAIDs = non-steroidal antiinflammatory drugs.
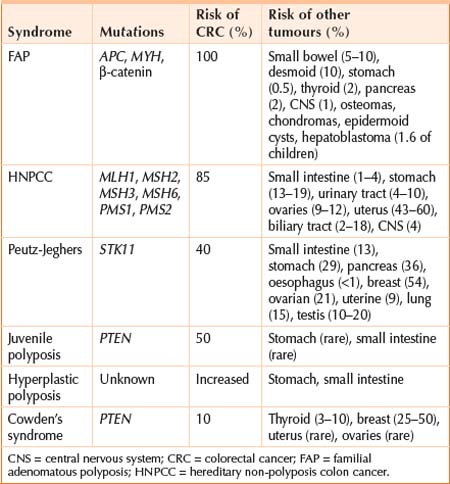
GENETICS
MULTI-STEP MODEL OF CRC
Specific genetic mutations
The APC (adenomatous polyposis coli) gene on chromosome 5 is the most critical gene in the early development of CRC. Somatic mutations in both alleles are present in 80% of sporadic CRCs. Most sporadic CRCs with wild-type APC have mutations in other genes of the Wnt signalling pathway, mostly in β-catenin.
Mismatch repair genes
Mismatch repair genes are the hallmark of HNPCC, but are also found in 15% of sporadic CRC. They are involved in correcting base mismatches and small insertions or deletions that occur during DNA replication. MSH2 and MLH1 are the most important ones followed by MSH6, MSH3, PMS1 and PMS2. The prognosis in this setting is better and the response to chemotherapy is less favourable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree