Coeliac disease
Isabel Polanco MD, PhD
Definition
Coeliac disease (CD) is an immunologically mediated enteropathy of the small intestine, characterized by lifelong intolerance to the gliadin and related prolamines from wheat and other cereals that occurs in genetically predisposed individuals1. Symptoms result from structural damage to the mucosa of the small intestine, which may cause malabsorption. Normal mucosal architecture is restored after commencing a gluten-free diet (GFD); villous atrophy reappears when gluten is reintroduced into the diet (gluten challenge)1,2,3.
Epidemiology
The true incidence of CD in susceptible populations may be dramatically higher than has been previously recognized1, 3, 4 and most cases remain undiagnosed, unless actively identified through mass serological screening. CD affects females more than males (ratio 2:1).
Genetic factors
The primary association of CD is the HLA-DQ dimer DQA1*0501/DQB1*0201. The majority of patients and first-degree relatives (and up to 20% of normal controls in susceptible populations) may express this dimer on antigen-presenting cells. The possession of this haplotype is not enough to cause gluten-induced changes, and the administration of extra-gluten to HLA-identical siblings of coeliac patients does not always result in pathological changes to the intestine. The HLA-DQ dimmer is also strongly linked to HLA-DR status8.
Pathology
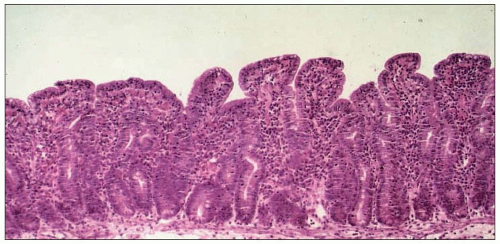
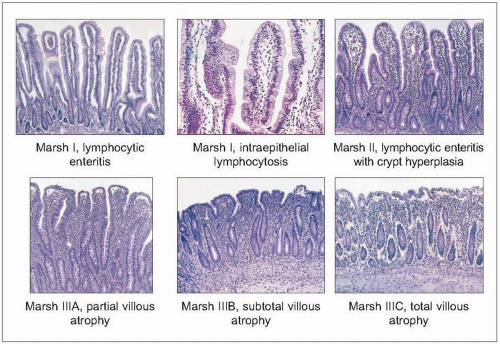
The proximal mucosa of the small intestine in patients with CD becomes abnormal on gluten ingestion and small bowel biopsy is essential to confirm the diagnosis (10.1). The abnormality is characterized by stunted or even absent villi associated with an increase in crypt length and cell numbers, the so-called ‘flat mucosa’ (10.2). The flat gut lesion is characteristic, but nonspecific of CD (Table 10.1)9.
All structural damage resolves on gluten withdrawal, but recurs if gluten is reintroduced to the diet. Similar intestinal changes are frequently found in dermatitis herpetiformis (DH), an intensely itchy, chronic papulovesicular skin
disorder, caused by granular subepithelial IgA deposits in the upper dermis. Both the cutaneous and intestinal lesions regress with a GFD. DH is now considered as a specific skin manifestation of CD.
disorder, caused by granular subepithelial IgA deposits in the upper dermis. Both the cutaneous and intestinal lesions regress with a GFD. DH is now considered as a specific skin manifestation of CD.
Table 10.1 Causes other than coeliac disease that may produce a flattened jejunal mucosa | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||
Clinical features
CD can appear with different clinical manifestations. In general, the first symptoms appear in the months following the introduction of gluten in the diet (10.3, 10.4). The earlier gluten is introduced, the shorter the interval between introduction and occurrence of the first symptoms. The first symptoms of CD, therefore, traditionally occur between 12 months and 3 years of age (Table 10.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree