CHAPTER 11 Chronic Abdominal Pain
The evaluation of any patient with a complaint of abdominal pain is challenging. Abdominal pain can be benign and self-limited or a harbinger of a serious life-threatening disease (see Chapter 10). Chronic abdominal pain poses a particularly challenging clinical problem. Not only is the management of chronic abdominal pain a frequently daunting task, but also the possibility of overlooking a structural or organic disorder is always a concern. Many disorders discussed elsewhere in this text can produce chronic abdominal pain (Table 11-1). Many of these diagnoses require careful consideration and clinical interrogation, in addition to appropriate diagnostic testing, to discern whether the entity is indeed the cause of the patient’s pain. Diagnosis of a functional gastrointestinal disorder is generally considered once potential causes of organic chronic abdominal pain have been confidently excluded. Although the causes of chronic abdominal pain are varied, the pathophysiologic pathways that produce chronic pain are common to many of them. This chapter focuses on the neuromuscular causes of chronic abdominal pain and the functional abdominal pain syndrome (FAPS). FAPS serves as a model to illustrate many of the complex issues involved in caring for patients with chronic abdominal pain.
Table 11-1 Differential Diagnosis of Chronic or Recurrent Abdominal Pain
| Structural (or Organic) Disorders |
| Inflammatory |
| Vascular |
| Metabolic |
| Neuromuscular |
| Other |
| Functional Gastrointestinal Disorders |
DEFINITION AND CLINICAL APPROACH
As for acute abdominal pain (see Chapter 10), the initial step in evaluating a patient with chronic abdominal pain is to elicit a detailed history from the patient. The chronology of the pain, including its abruptness of onset and duration, and its location and possible radiation should be determined. Visceral pain emanating from the digestive tract is perceived in the midline, because of the relatively symmetrical bilateral innervation of the organs, but is diffuse and poorly localized.1 Referred pain is ordinarily located in the cutaneous dermatomes that share the same spinal cord level as the affected visceral inputs.2 The patient should be questioned about the intensity and character of the pain, with the understanding that these parameters are subjective. The patient’s perception of precipitating, exacerbating, or mitigating factors may be useful when diagnostic possibilities are considered.
A complete physical examination is indicated to look for evidence of a systemic disease. The abdominal examination should use a combination of inspection, auscultation, percussion, and palpation. The most critical step for a patient with an acute exacerbation of chronic abdominal pain is to ascertain promptly whether a surgical abdomen is present (see Chapter 10). Although most causes of chronic abdominal pain do not require immediate surgical treatment, a complication related to a disease process ordinarily associated with chronic abdominal pain may present acutely (e.g., intestinal perforation in a patient with inflammatory bowel disease). Furthermore, a patient who has experienced chronic abdominal pain may present with acute pain related to another disease process (e.g., acute mesenteric ischemia in a patient with underlying irritable bowel syndrome [IBS]). The abdomen should be auscultated to detect an abdominal bruit, because the presence of a bruit may suggest chronic mesenteric ischemia (intestinal angina). Abdominal palpation for the presence of organomegaly, masses, and ascites and examination for hernias are particularly pertinent. Other physical findings that suggest an underlying organic illness include signs of malnutrition (e.g., muscle wasting or edema), vitamin deficiencies, or extraintestinal processes (e.g., arthropathy or skin changes). Although not entirely specific, the closed eyes sign is often seen in patients with FAPS (see later). Similarly, Carnett’s sign and the hover sign (described later) may be seen in persons with abdominal wall pain.
ABDOMINAL WALL PAIN
ANTERIOR CUTANEOUS NERVE ENTRAPMENT AND MYOFASCIAL PAIN SYNDROMES
Although ACNES was initially described in the 1970s, it remains a frequently overlooked cause of chronic abdominal pain.3,4 In ACNES, the pain is believed to occur when there is entrapment of a cutaneous branch of a sensory nerve that is derived from a neurovascular bundle emanating from spinal levels T7 to T12. The nerve entrapment may be related to pressure from an intra- or extra-abdominal lesion or to another localized process, such as fibrosis or edema. Pain emanating from the abdominal wall is discrete and localized, in contrast to pain originating from an intra-abdominal source, which is diffuse and poorly localized. Patients usually point to the location of their pain with one finger, and the examiner can often localize the area of maximal tenderness to a region less than 2 cm in diameter. During physical examination, the patient often guards the affected area from the examiner’s hands (hover sign).5 Patients often note that activities associated with tightening of the abdominal musculature are associated with an exacerbation of pain and, during physical examination, the clinician will note increased localized tenderness to palpation when the patient tenses the abdominal muscles (Carnett’s sign).6 In contrast, an increase in tenderness during relaxation of the abdominal musculature suggests an intra-abdominal source of pain.
In MFPS, pain emanates from myofascial trigger points in skeletal muscle.7 Causative factors include musculoskeletal trauma, vertebral column disease, intervertebral disc disease, osteoarthritis, overuse, psychological distress, and relative immobility. The exact pathophysiology of pain in MFPS remains unclear. Chronic abdominal wall pain may occur in patients with MFPS. Pain may be referred from another site, and the identification of trigger points (including those remote from the site of pain) is a useful physical finding. When attempting to identify a trigger point, the examiner uses a single finger to palpate a tender area. This is most often located in the central portion of a muscle belly, which may feel indurated or taut to palpation, and elicits a jump sign.8 This finding refers to a patient’s response by wincing, jerking away, or crying out as the myofascial trigger point is detected. Less commonly, trigger points may be located at sites such as the xiphoid process, costochondral junctions, or ligamentous and tendinous insertions.
Treatment of ACNES and MFPS, when successful, not only improves symptoms, but also confirms the diagnosis.9,10 The treatment strategy depends on the severity of the symptoms. With mild and intermittent symptoms that are reproducibly precipitated by certain movements, simple reassurance and a recommendation to avoid such movements may suffice. Non-narcotic analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), and application of heat can be used during exacerbations. Physical therapy may be beneficial, although no randomized studies have supported this treatment modality. For severe and persistent symptoms, injection therapy with a local anesthetic, with or without a glucocorticoid, is recommended.9–11 In one study of 136 patients in whom the history and physical examination suggested abdominal wall pain, and in whom benefit was noted with injection therapy, the diagnosis remained unchanged after a mean follow-up of four years in 97% of cases.12 In carefully selected patients with symptoms refractory to injection therapy, a prospective nonrandomized investigation has suggested that diagnostic laparoscopy with open exploration of abdominal trigger points may be beneficial.13 In this study, after intra-abdominal adhesions in close proximity to trigger points were lysed, subcutaneous nerve resection was performed. After a median postoperative follow-up of 37 months, 23 of 24 patients (96%) believed that this approach was beneficial in managing their previously intractable pain.
SLIPPING RIB SYNDROME
The slipping rib syndrome (SRS), which was described initially in the early 20th century,14,15 is an uncommonly recognized cause of chronic lower chest and upper abdominal pain. SRS ordinarily causes unilateral, sharp, often lancinating pain in the subcostal region. The acute pain may be followed by a more protracted aching sensation. The syndrome is associated with hypermobility of the costal cartilage at the anterior end of a false rib (rib 8, 9, or 10), with slipping of the affected rib behind the superior adjacent rib during contraction of the abdominal musculature. This slipping causes pain by a variety of potential mechanisms, including costal nerve impingement and localized tissue inflammation. The key to diagnosis is clinical awareness of the syndrome, in conjunction with use of the hooking maneuver; the clinician hooks his or her examining fingers underneath the patient’s lowest rib and, as the rib is moved anteriorly, the pain is reproduced and an audible pop or click is often heard.16 Conservative therapeutic measures often suffice but, on occasion, costochondral nerve blockade, response to which supports the diagnosis, or even surgical rib resection is required.17
THORACIC NERVE RADICULOPATHY
Disease related to thoracic nerve roots T7 through T12 may be responsible for abdominal pain. The disease processes that may cause this problem include neuropathy related to back and spine disorders, diabetes mellitus, and herpes zoster infection.18,19 Obtaining a complete history and performing a careful physical examination of the patient, with attention to the possibility of a systemic disease and abnormal neurologic and dermatologic findings, should lead to the correct diagnosis in most instances. Treatment depends on the specific underlying disease process.
FUNCTIONAL ABDOMINAL PAIN SYNDROME
FAPS is a distinct medical disorder. Evidence suggests that the syndrome relates to central nervous system (CNS) amplification of normal regulatory visceral signals, rather than functional abnormalities in the gastrointestinal tract.20,21 The disorder is characterized by continuous, almost continuous, or at least frequently recurrent abdominal pain that is poorly related to bowel habits and often not well localized. FAPS is properly understood as abnormal perception of normal (regulatory) bowel function rather than a motility disorder. The syndrome appears to be closely related to alterations in endogenous pain modulation systems, including dysfunction of descending and cortical pain modulation circuits.21 The Rome III diagnostic criteria for FAPS are shown in Table 11-2.20,21 Studies that included patients who meet diagnostic criteria for FAPS have revealed that only rarely is an organic cause of chronic abdominal pain found during long-term follow-up.22,23
Table 11-2 Rome III Criteria for Functional Abdominal Pain Syndrome*
| Must include all the following: |
2. No or only occasional relationship of pain with physiologic events (e.g., eating, defecation, menses) |
* Criteria fulfilled for the past three months with symptom onset at least six months prior to diagnosis.
FAPS is commonly associated with other unpleasant somatic symptoms, and, when it persists or dominates the patient’s life, it usually is associated with chronic pain behaviors and comorbid psychological disturbances.24 Patients with FAPS typically define their illness as medical, and their symptoms tend to be more severe and associated with greater functional impairment than those of patients with IBS.24 Psychological disturbances, if present, must be considered as comorbid features of FAPS rather than as part of a primarily psychiatric problem.25 When compared with patients who have chronic back pain, those with chronic abdominal pain report significantly better physical functioning, yet their overall perception of health is significantly worse.26
EPIDEMIOLOGY
Although the epidemiology of FAPS is incompletely known, in the U.S. Householder Survey of Functional Gastrointestinal Disorders, FAPS was estimated to be present in 2% of the sample and was less frequent than IBS (9%).27 A female predominance was noted (F:M = 1.5). Patients with FAPS missed more work days because of illness and had more physician visits than those without abdominal symptoms. A substantial proportion of patients are referred to gastroenterology practices and medical centers; they have a disproportionate number of health care visits and often undergo numerous diagnostic procedures and treatments.
PATHOPHYSIOLOGY
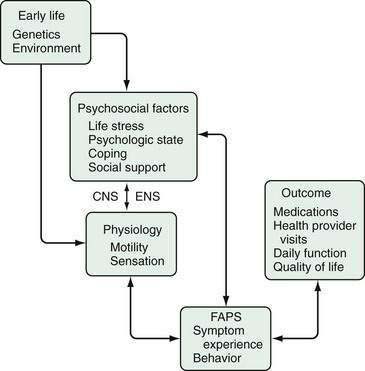
Chronic pain is a multidimensional (sensory, emotional, cognitive) experience explained by abnormalities in neurophysiologic functioning at the afferent, spinal, and CNS levels. Unlike acute pain arising from peripheral or visceral injury or disease, chronic functional pain is not associated with increased afferent visceral stimuli from structural abnormalities and tissue damage. FAPS is considered what is termed a biopsychosocial disorder related to dysfunction of the brain-gut axis (see Chapter 21).25 As shown in Figure 11-1, the clinical expression of FAPS is derived from psychological and intestinal physiologic input that interacts via the CNS-gut neuraxis. This model integrates the clinical, physiologic, and psychosocial features of FAPS into a comprehensible form, providing the basis for understanding psychological influences and application of psychopharmacologic treatments.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree