Foreign Bodies in the Gastrointestinal Tract and Anorectal Emergencies
Keywords
• Foreign bodies • Gastrointestinal tract • Endoscopic surgery • Anorectal emergency
Foreign bodies in the gastrointestinal tract
In the United States, 1500 people die each year due to ingested foreign bodies (FBs).1 Eighty percent of FB ingestions occur in young children who swallow small objects such as coins, toys, crayons, and ballpoint pen caps.2,3 Accidental FBs in adults tend to be caused by meat and bones. The remaining cases are found primarily among edentulous adults, prisoners, and psychiatric patients, who often intentionally ingest objects such as toothbrushes, spoons, and razor blades; and who are also more likely to recurrently ingest FBs.4–8 Wearing dentures is a significant risk factor in FB ingestion.9,10 Dentures eliminate the tactile sensitivity of the palate so that small objects or incompletely masticated food boluses are inadvertently swallowed. Of the FBs brought to the attention of physicians (probably a small minority of all ingestions), 80% to 90% will pass through the gastrointestinal (GI) tract spontaneously; however, 10% to 20% will require endoscopic removal, and about 1% will require surgery.11,12
Oropharyngeal foreign bodies
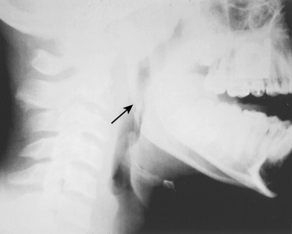
Most ingested FBs do not become impacted in the oropharynx. The most common exceptions are fish or chicken bones (Fig. 1), although any sharp or irregular object may become impacted.13–16 These objects most often lodge in the soft tissue at the base of the tongue, but may also be found in other areas such as the tonsil or piriform sinus.13 Minor lacerations and abrasions are common and self-limited. If the patient is drooling or is unable to tolerate oral intake of liquids, the clinician should be concerned about complete obstruction. Rarely, patients may also present with airway compromise. An unremoved FB may serve as a nidus for infection such as a retropharyngeal abscess, usually weeks later.17
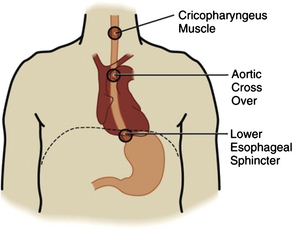
Patients usually know exactly when the object became impacted. Typically they present to the Emergency Department (ED) with a FB sensation and odynophagia several hours after ingestion, and they may have attempted one or more home remedies such as drinking fluid, eating bread, or trying to grasp the object with their own fingers. Due to the sensory innervation by the vagus and glossopharyngeal nerves, patients are able to accurately lateralize and determine the level of a FB in this region (Fig. 2).18 With larger objects the patient may also be drooling, retching, or vomiting.
More commonly, no FB can be identified. Indeed, less than 25% of patients with FB sensation after eating fish or chicken actually have an FB located by endoscopy.19–21 Despite this low rate, endoscopy within 24 hours rather than imaging studies is the next logical step, because radiography alters management extremely rarely (in only 1.5% [4 of 267] in one series).5,16,20,22,23
If imaging modalities are indicated because of the ingestion of a radiopaque object, plain films are usually the first step.13,16,24–26 Most radiopaque objects such as metal or glass should be visible. The visibility of fish bone depends on the fish species, location, and orientation; however, the majority are not seen on plain films, with much higher success in the hypopharynx than oropharynx.13,19,25,27
If plain films do not successfully locate an FB, an esophagogram with diluted barium or gastrografin can be performed in an attempt to outline the object.22,23,28 Further radiographs with barium-impregnated cotton balls and xeroradiography may be useful.5,23,29 Finally, computed tomography (CT) may identify fish or chicken bones missed on plain film.13,19,30,31
With the limited availability of prompt endoscopy at many times and in many EDs, there is likely to be a continued role for imaging studies in the initial assessment of these patients, even though most patients who present with an FB sensation will have no definitive findings at the conclusion of an extensive radiologic workup. At this point, because lacerations and abrasions may also cause an FB sensation and most serious complications are delayed, patients with a negative evaluation may be discharged home with strict return instructions and referral for endoscopy.5
Esophageal foreign bodies
Anatomy
The esophagus is a muscular tube that is continuous with the hypopharynx proximally and extends 18 to 25 cm distally to the gastroesophageal junction. It is divided anatomically into thirds: the proximal third consists of striated (voluntary) muscle, the distal third consists of smooth (involuntary) muscle, and the middle third is a mixture of the two. The proximal third has both somatic motor and sensory innervation through branches of the recurrent laryngeal nerve, similar to the oropharynx, which allows patients to localize proximal FBs accurately (see Fig. 2).18
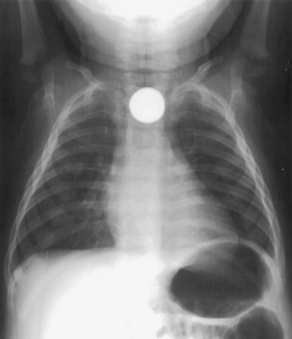
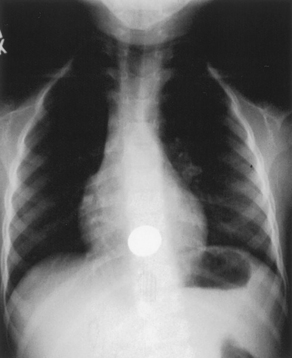
There are 3 areas of physiologic narrowing along the adult esophagus where blunt FBs most commonly become impacted (Fig. 3). The first area is located posterior to the cricoid cartilage, at the level of the C-6 vertebra, where the esophagus begins with the upper esophageal “sphincter” (UES) or cricopharyngeus muscle. The UES is the most common site of impaction in pediatric patients (Fig. 4).3,4,32 The second is at the level of T-4 where the distal aortic arch descends posterior to the mid-esophagus. Distally there is also an area of narrowing at the lower esophageal sphincter (LES). The LES is the narrowest point of the entire gastrointestinal tract in adults, and it is the location where most FBs become impacted (Fig. 5).4,32 Patients with an anatomic abnormality or motor disturbance of the esophagus are more prone to entrapment of food or other objects, and will usually present with a history of chronic swallowing problems. Anatomic abnormalities include strictures, webs, rings, diverticula, and malignancies.6,7 Motor disturbances are much rarer and include achalasia, scleroderma, diffuse esophageal spasm, or nutcracker esophagus.6,7
Epidemiology
Patients with retained esophageal FBs usually fall into 1 of 4 groups: pediatric, intentional adult ingestions, denture users, and adults with underlying esophageal pathology. Pediatric patients account for approximately 80% of retained esophageal FBs, with the peak incidence at 18 to 48 months.11,22,23,33–39 These small children habitually place objects in their mouths and can inadvertently swallow or aspirate them. The most commonly ingested objects in this age group are coins,5,6,36,40,41 but other small objects such as buttons and marbles are also commonly ingested.5,11,33,36,42 Unusual or multiple FBs should alert the examining clinician to possible child abuse.43 Patients with esophageal dysmotility are prone to impaction from even relatively small pieces of swallowed food.5–742
Complications
Many complications may arise from esophageal FBs, ranging from superficial mucosal injury to vocal cord paralysis, perforation, and life-threatening conditions such as retropharyngeal abscess and vascular injuries such as aortoesophageal fistula.44–50 Complications are more likely with FBs that have been impacted for more than 24 hours and with sharp objects.5,33 Most mortality from ingested FBs occurs because of complications from esophageal perforation.1,23
Presentation
Patients with an impacted esophageal FB usually present shortly after ingesting the object, and most adults and older children are able to provide a clear history of ingestion. The object is easily localized by the patient when it is located at the UES and upper third of the esophagus; however, when the object is located lower in the esophagus the patient may only have vague symptoms such as dysphagia, odynophagia, or a dull FB sensation that is not easily localizable. FBs at the UES may also cause gagging or vomiting.42 Drooling or the inability to handle secretions suggests complete esophageal obstruction.6
Patients in the 18- to 48-month-old age group, which has the highest incidence of FB ingestion, may present with carers who are unable to provide a history of FB ingestion. A high index of suspicion is required, and clinicians should inquire about an object that was in the patient’s mouth that “disappeared” or a transient history of coughing or gagging. An estimated 40% of FB ingestions in children are unwitnessed, and up to 50% never develop symptoms.51–56 Symptoms are nonspecific and include irritability, poor feeding, vomiting, coughing, wheezing, behavioral changes, and failure to thrive.6,14,51,57–59 Children are more likely than adults to have respiratory symptoms from an impacted esophageal FB, as their airway is softer and more compressible. Additional respiratory symptoms may include stridor, airway obstruction, and cardiac arrest.
Evaluation
When evaluating for an esophageal FB, the physical examination is usually normal.6,7 As noted, drooling suggests complete obstruction.6 Subcutaneous emphysema in the cervical region suggests esophageal perforation. Airway symptoms should be sought in children due to their softer and more compliant trachea.32
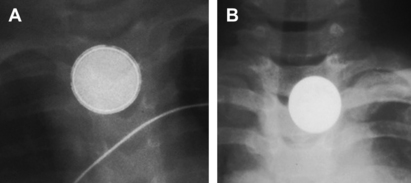
Because many patients are asymptomatic, and physical examination is usually normal, there should be a low threshold for obtaining plain radiographs.5 Plain films usually detect radiopaque FBs such as glass and metal, but most ingested objects (food bolus, toothpick, aluminum beverage pull-tab, and many fish and chicken bones) are missed by plain films.20,21,25,26,30,60 Because FBs preferentially become lodged at the UES in children and at the LES in adults, they will appear posterior to the tracheal air column on lateral view in children and beyond it in adults. Flat FBs are typically found to be lying in the frontal plane (see Figs. 4 and 5).61
For most patients with a food bolus impaction a plain film prior to propulsive therapy is prudent, as it may identify identification of a sharp fragments or other unanticipated disease in the thorax. If the diagnosis is in doubt, a contrast esophagogram may be obtained, although this decision is likely to make esophagoscopy much more difficult if it is required and is not without risk of aspiration, especially with high-grade obstructions.60,62,63 Esophagograms are also limited by high reported false-positive (19%–26%) and false-negative (40%–55%) rates.21,64 Barium is preferred to gastrografin unless there is risk of esophageal perforation, because it is much less toxic if aspirated. Newer nonionic solutions have been shown to be safe in either situation, but they are costly and may not be widely available.7,42 Consultation with an endoscopist, if available, is prudent before performing a contrast swallowing study.
An increasingly widely available alternative to both esophagograms and esophagoscopy is noncontrast CT of the neck and mediastinum (Fig. 6).19,62,65 In one study, CT found all impacted bony FBs located by endoscopy. In this study there was one false positive caused by esophageal calcification, and no false negatives.30 Another study also demonstrated 100% sensitivity of CT for localizing esophageal FBs as well as demonstrating that CT may provide the additional benefit of identifying complications, including an esophageal perforation that was not seen with barium swallow.31 A different study demonstrated this same benefit by locating an aortoesophageal fistula 7 days after the ingestion of a bone splinter.66
Management
Esophagoscopy
Esophagoscopy is the best available technique for retrieval of most esophageal FBs, and allows for evaluation of secondary injury.23,39 In many EDs the availability of esophagoscopy is limited, in which case other techniques described in this article may be needed. Clinical indications for immediate esophagoscopy include airway compromise (including stridor, coughing, or wheezing), evidence of obstruction or any FB that has been impacted for more than 24 hours, or if signs of perforation are present.5,39,40,67 Sharp or elongated FBs should be removed endoscopically, as there is a high risk of perforation (Fig. 7). Button batteries that cannot be passed into the stomach with swallowed water require immediate endoscopic removal. Patients with signs of obstruction should be encouraged to sit in whatever position is most comfortable for them (upright in most cases) and should be allowed to suction their own secretions. For obtunded or gagging patients, placement of a nasogastric tube in the esophagus above the obstruction may succeed in draining pooled secretions.
If esophagoscopy is not immediately available, the patient should be transferred to a facility where an experienced endoscopist is on hand. The success rate for the endoscopic removal of a sharp object is between 94% and 100%.23,39,68 Endoscopy should be performed under procedural sedation to prevent patient movements that may result in perforation or loss of the object into the patient’s airway. Failed endoscopic removal will require removal in the operating room.
Button batteries
Button batteries contain an alkaline solution that can rapidly cause liquefaction necrosis of the esophageal mucosa (Fig. 8). Perforation may occur within 4 hours, with catastrophic complications such as esophagotracheal or esophagoaortic fistula.49,69 If a child can cooperate, an attempt should be made to pass the battery into the stomach with swallowed water. Endoscopic removal of a button battery is challenging because of their smooth edges, and a collective review demonstrated that endoscopic removal failed 62.5% of the time.70 When removal fails, the battery can be pushed distally to the stomach where it will likely pass through the gastrointestinal tract without difficulty.70–73 Management of button batteries in the stomach is described in the section “Stomach and duodenal foreign bodies.” Follow-up with barium swallow studies to evaluate for a fistula or stricture is usually recommended at 24 to 36 hours and 10 to 14 days after the battery has been removed from the esophagus.23 Antibiotics are recommended when significant mucosal damage is present.
Coins
As with other esophageal FBs, coins tend to lodge at the level of the cricopharyngeus in children and the LES in adults (see Figs. 4 and 5).23 In young adults, accidental coin ingestion has become more common, due to a popular college drinking game called “Quarters.”5 Because coins in either the GI tract or the airway may cause similar symptoms, plain radiographs should be taken to determine the location of the coin.74–77 Mouth to anus films are indicated in the pediatric population to determine if more than one FB is present.5
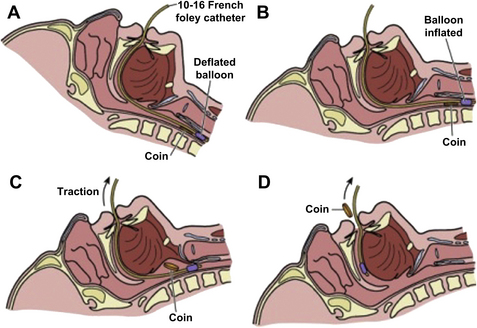
Coins lodged in the proximal or mid esophagus should undergo prompt extraction to avoid complications that are correlated with impaction times of longer than 24 hours.33,78–80 Although some authorities state that an asymptomatic patient with a coin in the distal esophagus may be given 12 to 24 hours to allow the coin to pass into the stomach, this approach may not be practical in settings with limited and unreliable follow-up.34–36,81,82 In most cases, impacted esophageal coins should be removed expeditiously, usually by endoscopy or, in children, by bougienage.5,68,81 The catheter technique for removal of esophageal coins and other foreign objects was widely practiced in the era prior to the wide availability of endoscopy (Fig. 9). Many complications can ensue, including esophageal perforation, laceration, regurgitation with or without aspiration, and airway obstruction. These risks are compounded by most emergency physicians’ lack of experience or familiarity with this techniques and the fact that more than 24 hours’ impaction, one of the indications for intervention, is itself a contraindication to Foley extraction. The technique may still be useful in remote or austere settings where endoscopy is not available. If it is undertaken, all precautions should be taken to protect the airway. The Foley catheter should be placed orally rather than nasally to ensure that the coin is not pulled into the nasopharynx, and the patient should be placed in deep Trendelenburg to minimize the risk of aspiration. Fluoroscopy may make this procedure safer.83,84
Bougienage, which has been successfully used to dislodge impacted esophageal coins in children, attempts to blindly advance the coin into the stomach. This technique has been used effectively by emergency physicians in pediatric patients, with a greater than 95% success rate and few reported complications, and results in significant reductions in ED length of stay and costs.38,85–88 However, the technique requires equipment that is not available in many EDs (a Hurst-type bougie in a variety of sizes), and has been reported in settings where the emergency physicians have received special training in centers that have developed extensive experience in the technique. Postprocedure films should be obtained to document coin location. Patients may be discharged home with instructions to obtain follow-up radiographs if the coin is not noted in the stool within a week. All adults should obtain follow-up to evaluate for an underlying esophageal disorder.5
Pharmacologic therapies
FBs that pass the LES are usually able to pass along the remainder of the GI tract without complication. Several pharmacologic therapies have been developed to aid a blunt or smooth FB at the LES to pass into the stomach. Some of these such as atropine, meperidine, and diazepam have been shown to have success rates lower than observation alone.33,42 Papain was used in the past to dissolve impacted meat,89 but this practice has been abandoned because it can also dissolve the esophageal mucosa, resulting in esophageal rupture.90,91 Glucagon, nitroglycerin, nifedipine, and gas-forming agents have proved to be the most effective pharmacologic agents in the management of distal blunt esophageal FB impactions, and are discussed individually here. Anxiolysis and pain control are also an important aspect of FB management, and may account for some of the success of the other pharmacologic agents discussed.92
Glucagon
The action of glucagon is thought to result from relaxation of the smooth muscle found in the distal esophagus and a decrease in the LES resting pressure.93 Glucagon has no effect on the striated muscle of the proximal esophagus, where children often have impacted FBs. The therapeutic dose is 0.25 to 2.0 mg administered intravenously.
A common side effect of glucagon, if administered too rapidly, is nausea and vomiting. This effect may be responsible for some of the drug’s success in clearing obstruction94; however, there is a theoretical risk of rupture of an obstructed esophagus with vomiting, so slow injection over 1 to 2 minutes is recommended. Mild elevation of blood glucose may also occur, but blood glucose does not need to be monitored.
The onset of action is less than a minute and the effects last about 25 minutes. After administration, the patient should be sitting upright and should be encouraged to take a sip of water approximately 1 minute after injection to induce esophageal peristalsis. A second dose may be used if the first is not successful. Glucagon is often thought of as a first-line agent. Its success rate of less than 38% can be improved when combined with gas-forming agents or carbonated beverages.95–97
Nitroglycerin and nifedipine
Sublingual nitroglycerin and nifedipine have been used in a manner analogous to that of glucagon for the disimpaction of distal blunt esophageal FBs.98–100 Nitroglycerin reduces distal esophageal spasm and contraction, and nifedipine relaxes the LES in a manner similar to glucagon. Either may be used in combination with glucagon, but nitroglycerin and nifedipine should not be used simultaneously. The therapeutic dose is 1 to 2 (0.4 μg) sublingual nitroglycerin tablets or 5 to 10 mg of nifedipine. Patients with impacted esophageal FBs may be dehydrated because of an inability to swallow, and may be extremely sensitive to these agents, placing them at risk of iatrogenic hypotension. Intravenous access with a widely patent line sufficient for volume resuscitation should be placed, and the patient adequately hydrated before administration of these medications.
Gas-forming agents
Gas-forming agents and carbonated beverages have been used successfully for the treatment of distal esophageal food impactions. These solutions produce carbon dioxide, which is thought to distend the esophagus, relaxing the LES, and pushing the FB distally into the stomach.96,101,102 Their use may increase the success of other spasmolytic agents.101,103 Solutions described in the literature include a combination of 15 mL tartaric acid (solution of 18.7 g/100 mL water) followed immediately by 15 mL of sodium bicarbonate (10 g/100 mL water) or 1.5 to 3 g of tartaric acid dissolved in 15 mL of water followed by 2 to 3 g of sodium bicarbonate in 15 mL of water.96,101 Commercially available gas-forming granules have also been used successfully.104 Carbonated beverages (100 mL) may also work, and are more likely to be readily available in the ED.97,102 Gas-forming agents should not be used if the FB has been impacted for more than 6 hours; if the patient is complaining of chest pain suggestive of esophageal injury; or if there is concern for obstruction, as there have been rare reports of esophageal perforation.96,101,105
If the patient has improvement of symptoms after pharmacologic intervention, a postprocedure radiograph or contrast study may be obtained to confirm passage into the stomach. Adult patients may be discharged home after successful disimpaction of an esophageal FB, but they should have close follow-up, as the majority will have an underlying esophageal disorder.23 Patients who have had an esophageal FB dislodged by any method should be instructed to return to the ED with any chest or abdominal pain, persistent vomiting, hematemesis, difficulty swallowing, or shortness of breath.96
Stomach and duodenal foreign bodies
The vast majority of FBs that enter the stomach pass through the entire GI tract uneventfully. Objects longer than 5 cm may have difficulty negotiating the tight curve of the duodenum, and objects larger than 2 cm in diameter may have difficulty passing the pylorus or ileocecal valve.106,107 Less than 1% of FBs that enter the stomach cause perforation of the bowel108; however, some investigators describe an intestinal perforation rate of 35% with sharp objects (usually at the ileocecal valve) whereas others, especially in the pre-endoscopic era, reported much lower rates.78,109
Management of the patient with an FB in the stomach or duodenum varies depending on the nature of the FB and the patient’s symptoms. Emergent endoscopy is a high priority if objects are long (>5 cm), of large diameter (>2 cm), or sharp, especially needles or toothpicks.5,40,67,110 Small blunt objects can be observed and followed with serial radiographs.6 If an object remains in the stomach for more than 7 days, the patient should be referred to a gastroenterologist for removal. If a patient becomes symptomatic, the object should be removed. Button batteries and drug packets require special attention and are discussed further.
Button Batteries in the Stomach
Button batteries should be followed with daily radiographs. Up to 85% will pass through the entire GI tract within 72 hours.69,81 A button battery should be removed endoscopically if it remains in the stomach for more than 36 to 48 hours or if the patient becomes symptomatic. H2 blockers have been suggested to decrease the stomach acid reaction with the battery, but no benefit from this therapy has been confirmed.69 Once past the duodenum, FB are no longer endoscopically accessible. Radiographs are needed only every 3 to 4 days to document progression if the FB has not been identified in the stool. A button battery that fails to pass or becomes symptomatic must be removed surgically. Although extremely rare, toxic serum concentrations of mercury have been reported, especially if the integrity of the battery (as determined by history or radiograph) has been disrupted, and may require chelation therapy.69,111–113
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree