CHAPTER 63 Biliary Tract Motor Function and Dysfunction
ANATOMY AND PHYSIOLOGY
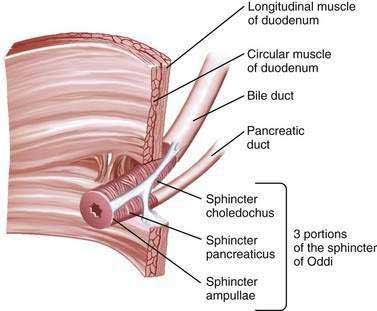
The sphincter of Oddi (SO) is composed of layers of smooth muscle that are embedded in, but functionally separate from, the muscle of the duodenal wall and that serve as a 6 to 10 mm high pressure zone. Three portions of the SO are identified: a small segment (sphincter ampullae) that covers the common channel formed by the union of the bile and pancreatic ducts (when a common channel is present); a second small portion (sphincter pancreaticus) that surrounds the beginning of the main pancreatic duct; and the largest portion (sphincter choledochus) that covers the distal bile duct (Fig. 63-1). In addition, the fasciculi longitudinales are muscle bundles that span intervals between the bile and pancreatic ducts and promote the flow of bile into the duodenum during contraction (see Chapter 62). In humans, the SO functions primarily as a resistor, with tonic contraction that limits bile flow during the interdigestive period. It also serves as a pump, with phasic contractions that facilitate the flow of bile into the duodenum, perhaps serving a housekeeping function for the distal bile duct. The SO participates in the migrating motor complex, with motilin-induced increases in the frequency and amplitude of sphincter contractions shortly before and during bursts of intense duodenal contractions. The complex neurohormonal control of biliary motility involves sympathetic, parasympathetic, and enteric nerves. Almost every neurotransmitter in the enteric nervous system has been identified in the biliary tree.
GALLBLADDER DYSKINESIA
Biliary dysmotility, or clinical problems related to abnormal biliary tract motility, can occur in either the gallbladder or the SO. Although gallbladder stasis clearly predisposes to sludge and stone formation, whether gallbladder dysfunction, or delayed emptying of the gallbladder in the absence of stones or sludge, causes biliary symptoms is unclear. Patients who experience typical biliary pain but have no evidence of gallstones may be studied with scintigraphic imaging of the gallbladder during intravenous infusion of cholecystokinin (CCK). Delayed gallbladder emptying has been reported to be predictive of pain relief after cholecystectomy,1,2 although this finding remains controversial.3,4 Delayed gallbladder emptying is more common in patients with functional bowel disorders than in control subjects.5 In many of these patients, symptoms are probably caused by the underlying functional bowel disorder, and the gallbladder dysmotility is incidental. The histologic diagnosis of chronic cholecystitis in resected gallbladders has been proposed as confirmation of a gallbladder source of symptoms,1,2 although this suggestion also has been disputed.6 A meta-analysis of 9 studies3 and a systematic review of 23 studies4 concluded that evidence that the gallbladder ejection fraction predicts symptomatic relief after cholecystectomy is lacking (see Chapter 67). A more recent, smaller meta-analysis of mostly retrospective data, however, demonstrated a statistically significant benefit to cholecystectomy in symptomatic patients with gallbladder dyskinesia.7 To complicate matters further, many patients with biliary pain, no stones on ultrasound (US), and normal CCK scintigraphy experience symptomatic improvement after cholecystectomy.8 Although many surgeons offer laparoscopic cholecystectomy to patients with biliary pain and delayed gallbladder emptying, further prospective clinical trials are necessary to determine definitively the role of CCK cholescintigraphy in the management of acalculous biliary pain.
SPHINCTER OF ODDI DYSFUNCTION
EPIDEMIOLOGY
The frequency of manometrically detected SOD in patients with an intact gallbladder has not been well studied. Elevated basal SO pressure has been reported in 40% of patients with gallbladder stones, with or without biliary pain (“biliary colic”).9 When elevated levels of liver enzymes were present, 40% of 25 patients with gallbladder stones but without bile duct stones had an elevated basal SO pressure. Ruffolo and coworkers reported that approximately 50% of 81 patients with biliary-type pain, an intact gallbladder, and no evidence of gallstones had delayed gallbladder emptying, SOD, or both.10 By contrast, no basal SO pressure elevation greater than 30 mm Hg was found in 50 asymptomatic volunteers without gallstones.11
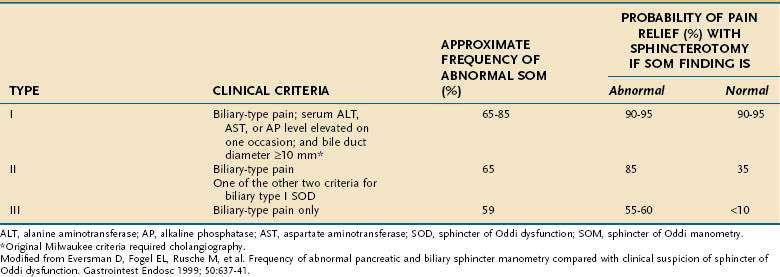
The frequency of SOD in postcholecystectomy patients with persistent or recurrent biliary-type pain has been better studied but depends on the criteria for patient selection. Pain resembling preoperative biliary pain occurs in 10% to 20% of postcholecystectomy patients.12 The most common explanation is that the preoperative symptoms were not caused by gallstones. The most likely diagnosis in this group of patients is a functional gastrointestinal disorder such as irritable bowel syndrome or functional (nonulcer) dyspepsia. SOD has been reported in 9% to 14% of patients evaluated for postcholecystectomy pain.13 When other causes of postcholecystectomy pain have been excluded and SO manometry (SOM) (see later) has been performed in a more carefully screened group, the frequency of SOD is 30% to 60%.14 When these patients are classified by the Milwaukee classification for possible SOD (Table 63-1), the frequencies of elevated basal SO pressure are 86%, 55%, and 28% for patients with suspected types I, II, and III SOD, respectively (see later).
CLINICAL FEATURES
SOD is a possible cause of three clinical conditions: (1) persistent or recurrent biliary-type pain following cholecystectomy, (2) recurrent idiopathic (unexplained) pancreatitis, and (3) biliary-type pain in patients with an intact gallbladder but without cholelithiasis (the least studied and most controversial clinical association) (Table 63-2). SOD generally occurs spontaneously, but has also been described with increased frequency in patients who have undergone liver transplantation,15 have the acquired immunodeficiency syndrome,16 are chronic opium users,17 or have hyperlipidemia.18
Table 63-2 Clinical Associations with Sphincter of Oddi Dysfunction
| Strong | Biliary-type pain postcholecystectomy |
| Probable | Biliary-type pain in a patient with an intact gallbladder |
| Idiopathic acute recurrent pancreatitis | |
| Possible | Acquired immunodeficiency syndrome–associated viral and protozoal infections |
| After liver transplantation | |
| Chronic pancreatitis | |
| Hyperlipidemia | |
| Opium use |
Although biliary SOD has been diagnosed in all age groups, it is most common in middle-aged women. The female preponderance varies from 75% to 90%. The pain is typical of biliary pain; it is severe and occurs in the epigastrium or the right upper quadrant and may radiate to the back or right shoulder blade. The pain is episodic, lasts more than 30 minutes, and occurs at least once a year.19 Less than half of affected patients have abnormal liver biochemical test results with or without the pain, although transient elevation of serum aminotransferase levels during attacks of pain supports the diagnosis of SOD.
CLASSIFICATION
According to the modified Milwaukee classification system (see Table 63-1), type I SOD is diagnosed in patients with biliary-type pain, serum liver enzyme (aminotransferase or alkaline phosphatase) levels that are elevated (more than 1.1 times the upper limit of normal), and bile duct dilatation to a diameter greater than 9 mm. Type II SOD is defined as biliary-type pain and either elevated liver enzyme levels or a dilated bile duct. Type III SOD is defined as biliary-type pain without any of the other objective abnormalities. This classification system does not require that the liver enzyme elevations be timed with attacks of pain, although such an association may be a predictor of response to treatment.
The original Milwaukee classification system incorporated more stringent criteria, including aminotransferase or alkaline phosphatase elevations greater than twice the upper limit of normal on two separate occasions, biliary dilatation greater than 12 mm, and delayed drainage (>45 minutes) of bile into the duodenum at cholangiography. The stringency of these criteria has been questioned,20–22 and their use in clinical practice has diminished.
A similar classification system for possible pancreatic SOD has been proposed.23 Patients with pancreatic SOD type I have pancreatic-type pain, a serum amylase or lipase level of at least 1.1 times the upper limit of normal on one occasion, and pancreatic duct dilatation (>6 mm in the head and >5 mm in the body); those with pancreatic SOD type II have pain and one of the other criteria; and those with pancreatic SOD type III have pancreatic-type pain only. Several studies have demonstrated a high frequency (30% to 65%) of SO hypertension in patients with unexplained recurrent pancreatitis and a frequency of 50% to 87% in those with chronic pancreatitis.24 The usefulness of this classification system for pancreatic SOD has not been tested and will depend on studies of the symptomatic outcome following pancreatic sphincter ablation.
DIAGNOSIS
Noninvasive Tests
Biliary scintigraphy can be used to assess flow of bile into the duodenum and has been proposed as a safe screening test before SOM. Although scintigraphy findings are usually positive in patients with dilated bile ducts and high-grade biliary obstruction, the modality lacks sufficient sensitivity in patients with lower-grade obstruction (Milwaukee classification types II and III SOD).25 After a lipid-rich (fatty) meal or intravenous administration of CCK, the bile duct may dilate under pressure if the SO is dysfunctional, and this change can be detected on transcutaneous ultrasonography. Compared with SOM in postcholecystectomy patients, fatty meal ultrasonography has a sensitivity of 21% and a specificity of 97% for SOD.26 Similarly, after stimulation by intravenously administered secretin, the pancreatic duct may dilate, and this test therefore can be used to assess pancreatic sphincter dysfunction. Compared with SOM, secretin-stimulated ultrasonography testing has a sensitivity of 88% and a specificity of 82% for SOD in patients with recurrent acute pancreatitis.27
Secretin-stimulated magnetic resonance pancreatography has also been used to assess pancreatic outflow obstruction in patients with idiopathic acute recurrent pancreatitis. Preliminary reports have shown high specificity but low sensitivity rates compared with SOM.28 Similarly, in one study secretin-stimulated endoscopic ultrasonography showed limited sensitivity in the evaluation of patients with recurrent pancreatitis and manometrically proved SOD.29
Invasive Tests
Patients in whom SOD is suspected have the highest complication rates for endoscopic retrograde cholangiopancreatography (ERCP). Such patients have a three-fold increase in the risk of post-ERCP pancreatitis, with absolute rates exceeding 25%.30 Although the prophylactic placement of a temporary pancreatic stent reduces the risk of post-ERCP pancreatitis,30,31 substantial morbidity and occasional mortality occur in patients who undergo ERCP for SOD. Therefore, ERCP with manometry should be reserved for persons who have severe or debilitating symptoms. Cholangiography is essential for excluding stones or tumors as the cause of biliary obstruction and associated symptoms. Although alternative biliary imaging methods, such as magnetic resonance cholangiopancreatography and endoscopic ultrasonography, are safer than ERCP for excluding stones, tumors, and pancreas divisum, they cannot diagnose (or be used to treat) SOD.
Occasionally, an intra-ampullary neoplasm may simulate SOD. If there appears to be excess tissue in the ampulla after endoscopic sphincterotomy, biopsy specimens of the area should be obtained.32