CHAPTER 7 Bariatric Surgery
EPIDEMIOLOGY OF MORBID OBESITY
Morbid obesity is the leading public health crisis of the industrialized world (see Chapter 6).1,2 The prevalence of obesity in the United States continues to rise at an alarming rate, with two thirds of adults currently considered overweight, half of whom are obese.3 Being overweight is defined by the body mass index (BMI): normal BMI = 25 kg/m2; BMI for obesity > 30 kg/m2; BMI for morbid obesity > 40 kg/m2; and BMI for supermorbid obesity > 50 kg/m2. Rising rates of obesity are seen across the United States in men and women and in all major racial, ethnic, and socioeconomic groups.4 Morbid obesity reduces life expectancy by five to 20 years and, for the first time in history, it is predicted that the current generation may have a shorter life expectancy than the last.5,6
BARIATRIC SURGERY AS TREATMENT FOR MORBID OBESITY
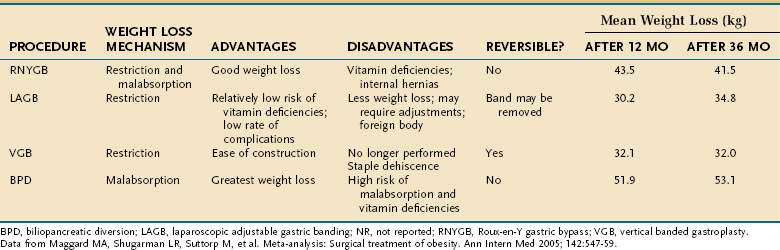
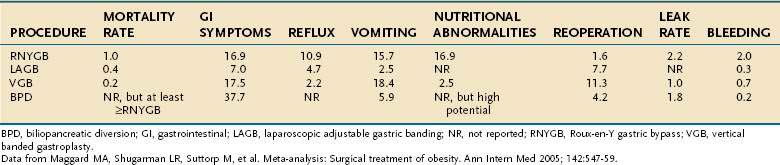
Bariatric surgery remains the only effective and enduring treatment for morbid obesity. Since 1997, the number of bariatric surgical procedures in the United States has grown sevenfold as evidence has proven their safety and efficacy.7 Weight loss operations can be classified as malabsorptive or restrictive (Fig. 7-1). Roux-en-Y gastric bypass (RNYGB), which accounts for 88% of bariatric procedures in the United States, is restrictive and malabsorptive. Biliopancreatic diversion–duodenal switch (BPD-DS), the other malabsorptive procedure, is not as commonly performed in the United States because of its higher risk profile. Purely restrictive procedures include the laparoscopic adjustable gastric banding (LAGB), vertical banded gastroplasty (VBG), gastrectomy, and sleeve gastrectomy procedures, all of which reduce the size of the stomach so it is unable to accommodate more than a few ounces of food. VBG is no longer performed commonly because of its potential for staple line dehiscence and subsequent weight gain. Advantages, disadvantages and complications of the major weight loss operations are shown in Tables 7-1 and 7-2.
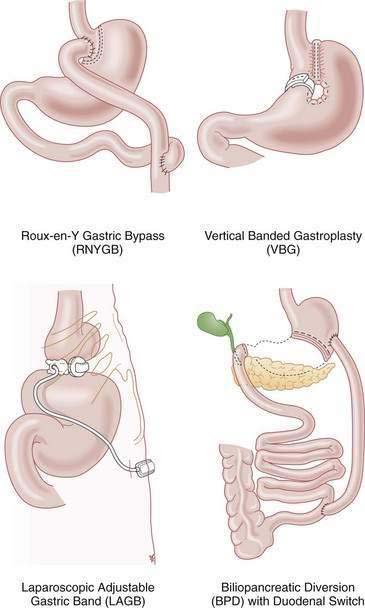
Figure 7-1. Types of weight loss operations.
(From the American Society for Bariatric Surgery. The story of surgery for obesity, 2005. Available at www.asbs.org.)
PREOPERATIVE EVALUATION
To qualify for bariatric surgery, patients must meet the 1991 NIH consensus criteria, which include having a BMI > 40 kg/m2 or a BMI > 35 kg/m2 with obesity-related comorbidities, and at least six months of documented, medically supervised weight loss attempts.8 Some bariatric surgeons require patients to lose additional weight through diet and exercise between the time of initial bariatric surgery consultation and the date of operation. This additional required preoperative weight loss is not correlated with comorbidity resolution or complication rates, but is associated with shorter operative times and greater weight loss at one year after the surgery; therefore, it should be encouraged in all patients.9,10
Prior to surgery, patients must complete an extensive screening process, including consultation with a surgeon, psychologic evaluation, nutrition consultation, chest roentgenography, electrocardiography, pulmonary function testing, a sleep study, and an esophagogastroduodenoscopy (EGD). The EGD was recommended by the European Association for Endoscopic Surgery to detect and treat any upper gastrointestinal lesions that may cause postoperative complications or influence the decision of which type of bariatric surgery should be performed.11
In a study of 272 gastric bypass patients who underwent preoperative EGD, 12% had clinically significant preoperative findings that included erosive esophagitis (3.7%), Barrett’s esophagus (3.7%), gastric ulcer (2.9%), erosive gastritis (1.8%), duodenal ulcer (0.7%), and gastric carcinoid (0.3%); 1.1% had more than one lesion. Given that 12% of patients who eventually underwent RNYGB had clinically significant preoperative findings, and only 67% of them had upper gastrointestinal symptoms, it is important to perform EGD preoperatively, because the excluded distal stomach cannot be evaluated easily after a RNYGB procedure.12 Patients undergoing LAGB surgery also should undergo a preoperative EGD, especially to evaluate gastroesophageal reflux disease (GERD). Gastric banding leads to satiety and weight loss by creating a small restrictive stomach with a slow gastric emptying time. Patients who overfill their small stomach pouch post-LAGB can force food and stomach acid back up into their lower esophagus, thereby worsening any preexisting GERD.13,14 In addition, overzealous banding adjustment may lead to pseudoachalasia with an increased pressure zone below the lower esophageal sphincter, furthering any incompetence.
EFFICACY
The steep rise in the use of bariatric surgery can be attributed to its proven efficacy as a treatment for morbid obesity. Two meta-analyses have provided strong validation that bariatric surgery leads to successful weight loss and mortality reduction.15,16 A meta-analysis by Buchwald and colleagues that included 22,094 patients found the mean percentage of excess weight loss (EWL) for all patients to be 61.2%.15 EWL is highest for VBG (68.2%), lower for RNYGB (61.6%), and lowest for LAGB (47.5%). A meta-analysis by Maggard and associates found similar weight loss trends at three or more years postoperatively, with the greatest weight loss achieved after the malabsorptive procedures of BPD-DS (53 kg) and RNYGB (42 kg), and less weight loss after the restrictive LAGB (35 kg) and gastroplasty (32 kg).16
EFFECTS ON MORTALITY AND MORBIDITY
Such substantial weight loss is associated with a clear reduction in long-term mortality. A retrospective cohort study of 9,949 RNYGB patients matched to 9,628 severely obese controls found that having RNYGB surgery reduces the adjusted long-term mortality from any cause of death by 40%.17 Among RNYGB patients, mortality was decreased 56% from coronary artery disease, 92% from diabetes, and 60% from cancer. In another study, a 14% decrease in cancer incidence was shown in patients who underwent RNYGB, the biggest reductions in which were seen among types of cancers that are considered obesity-related: esophageal adenocarcinoma (2% reduction), colorectal cancer (30% reduction), breast cancer (9%), uterine cancer (78%), non-Hodgkin’s lymphoma (46%), and multiple myeloma (54%).18 The lower cancer risk of patients after RNYGB presumably was caused by weight loss, which has been shown in many studies to reduce cancer incidence. Furthermore, once obese patients lose weight, they may have better access to needed health surveillance, such as Pap smears and colonoscopy. Finally, given that increased BMI leads to worse surgical oncologic outcomes, it may be surmised that with weight loss, a better surgical outcome may be anticipated.
Overall, bariatric surgery dramatically improves survival and decreases mortality from all disease-related causes of death. Only rate of deaths not caused by disease, including deaths resulting from accidents and suicide, increased after bariatric surgery and were 58% higher in the RNYGB patients17; it has been speculated that alcohol abuse may explain why accidents and suicides were higher in the surgical group. One study demonstrated altered alcohol metabolism after gastric bypass surgery, with the gastric bypass patients having a greater peak alcohol level and a longer time for the alcohol level to reach a zero blood level than in controls.30 Another study of bariatric surgery candidates found that 9% reported having attempted suicide and 19% reported having abused alcohol preoperatively.19 There is concern that this vulnerable patient population has additional difficulty with the psychological adjustments to weight loss, further supporting the need for psychological counseling before and after surgery.20,21
In addition to benefiting from a decreased mortality, bariatric patients benefit from decreased morbidity. Morbidly obese patients suffer from more intense gastrointestinal symptoms (e.g., abdominal pain, heartburn) and sleep disturbances than normal-weight patients. By six months after RNYGB, however, the frequency and severity of gastrointestinal symptoms of many morbidly obese patients have decreased to levels seen in normal weight patients. Dysphagia is common in morbidly obese patients, all of whom experience increased intra-abdominal pressure. Dysphagia is the only gastrointestinal symptom that worsens after RNYGB, probably from further increase in esophageal pressure because of overeating and overfilling of the restrictive small gastric pouch; this observation again underscores the need for preoperative and postoperative education regarding diet.27
Quality of life, as measured by the validated SF36 survey, improves greatly after RNYGB surgery. Preoperatively, morbidly obese patients score significantly lower than U.S. population norms in the categories of general health, vitality, physical functioning, bodily pain, emotional, and social functioning. As soon as three months following RYNGB, these same patients scored no differently than U.S. norms in these categories.28
COMORBIDITY RESOLUTION
Weight loss surgery is a singular medical intervention that can reverse or improve the numerous medical conditions associated with obesity. RNYGB results in a substantial reduction in cardiac risk factors with the following resolution rates: diabetes (82%), hypertension (70%), and hyperlipidemia (63%).29 Gastric bypass has assembled the most evidence of comorbidity resolution; however, all weight loss operations result in some degree of improvement. The meta-analysis by Buchwald and coworkers15 found that bariatric surgery reverses, ameliorates, or eliminates major cardiovascular risk factors:
One study found resolution of all conventional abnormal risk factors, including serum levels of total cholesterol, low-density lipoprotein, high-density lipoprotein (HDL), triglyceride, high-sensitivity C-reactive protein, homocysteine, and lipoprotein A at one year after RNYGB.30
The Swedish Obese Subjects (SOS) Study has provided further demonstration of the ameliorative effect of bariatric surgery. At 10 years of follow-up, surgically treated obese patients had 25% reduction in hypertension, 43% improvement in HDL, and 75% reduction in diabetes compared with the medically treated group.31
Beyond the significant improvement in cardiac risk factors, weight loss surgery also provides substantial relief of the many medical problems that obesity causes. One study found that a leading digestive health complaint, GERD, is cured or improved at a 96% rate.29 Other studies also have documented a highly significant reduction in GERD symptoms after bariatric surgery.27,32
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree