Presenting complaint
N
Chordee (11 fistula)
41
Urethral stricture + chordee or fistula
35
Lichen Sclerosis (LS)
11
Hairy urethra (stones or retention)
8
Spraying of urine/subterminal meatus
57
Aesthetic concerns ± spraying
59
Primary repair (6 distal, 4 mid-penile)
10
Total
221
History
Perhaps no other surgical condition in pediatric urology has inspired more surgical innovations than hypospadias. There are more than 200 surgeries that have been described for hypospadias correction and a recent Medline search revealed more than 5,000 publications on the subject. There is nothing new in hypospadias surgery that has not been previously described. As with any surgical procedure, the results we see today are directly attributable to the building process in medicine, capitalizing on other ideas, refining them and adding subtle improvements to end up with a surgical technique that is reliable and reproducible by other surgeons.
The significance of chordee was appreciated by Galen in the second century AD and forgotten until Mettauer [7] in 1842 recognized skin shortening as a cause of chordee. It was not rediscovered until 1967 by D.R. Smith [8] and 1970 by Lowell King [9] who reemphasized that the principal structure of the penile curvature is commonly proximal to the meatal orifice, a concept described by Mettauer more than 100 years prior when he advocated “a succession of subcutaneous incisions until the organ is liberated” [7].
In 1869, Professor C. Thiersch [10] reported that in 1857 and 1858 he tubularized the urethral plate in a child born with epispadias and credited the technique to August Brauser, his one-time assistant. Thiersch’s classic article illustrated the design of the flaps and the asymmetric lateral incisions so that the suture lines are unopposed. In 1874, Duplay [11] described the tubularization of the urethral plate distal to the hypospadic meatus. He also stressed the importance of complete chordee release before urethroplasty.
In prior years, glandular and coronal hypospadias were often not repaired because the complications overshadowed the benefits of surgical correction. Duckett’s [12] meatal advancement and glanduloplasty technique (MAGPI) was designed to reduce the risks of formal urethroplasty in distal hypospadias. Zaontz [13] applied the Thiersch–Duplay principle to the repair of distal hypospadias. He reported excellent results with the glans approximation procedure (GAP), an operation indicated for patients with coronal meatus and a deep glandular groove. This procedure can be used in adults with equal success. Midline incision of the urethral plate was first reported by Reddy in 1975 [14]. He made the incision to excise the “fibrous tissue” in the midline that he believed to be the cause of chordee. He then combined the incision with the Thiersch–Duplay method and tabularized the urethral plate. Rich et al. [15] incised the plate to create a normal slit-like meatus by hinging the distal urethral plate longitudinally in the midline, but Snodgrass [16] reported and popularized the tubularized incised plate urethroplasty (TIP) repair which is currently the most widely used technique.
Epidemiology
Hypospadias is the most common urogenital malformation second only to cryptorchidism and occurs in 1/250–300 [17, 18]. It has been previously postulated that the incidence of hypospadias in children is rising [19]; however, subsequent studies have not shown the same results [20]. Hypospadias has been associated with advanced maternal age [21, 22] and in vitro fertilization [23].
Given the dearth of longitudinal literature on hypospadiacs, little is known about the natural history of this population. While it is well documented that hypospadias patients—both previously repaired and never-repaired, frequently present with urinary complications in adolescence and adulthood [6, 24], the “hypospadias cripple” presents the greatest surgical challenge and these patients are subject to the highest complication rates [25]. The incidence of late complications is uncharacterized, with some studies reporting about 50 % of patients experiencing some complications. While about 1/3 of these complications occur in the first 5 years, nearly 1/5 of the complications occur after 5 years [26]. Importantly, this study did not include patients who underwent staged reconstructions, and therefore, this cohort represents a group of patients with “mild to moderate” defects. Complications can come in the form of cosmetic issues, chordee, fistula/diverticulae, foreign material in the urethra (typically hair/stone), and recurrent stricture. Surgical therapy therefore must be tailored to the complication and a detailed discussion of all these problems is beyond the scope of this project.
Long-Term Outcomes: Psychosocial, Erections, Ejaculation, Micturition (Figs. 4.1, 4.2, 4.3, and 4.4)

Fig. 4.1
116/221 adults complain of spraying from subterminal meatus and poor aesthetics
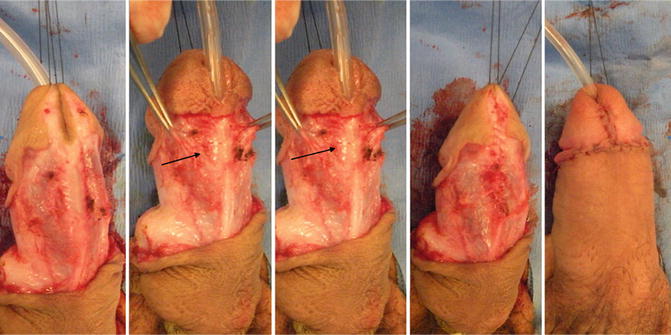
Fig. 4.2
Urinary spraying, subterminal wide meatus and spongiosum deficiency (arrow). GAP repair and spongiosal approximation to prevent diverticulum formation
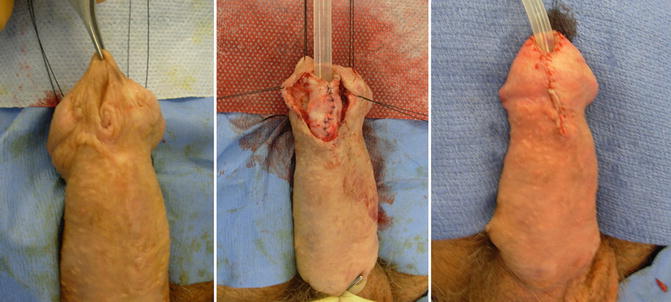
Fig. 4.3
Distal urethroplasty and glandular sculpting for urine spraying and cosmesis
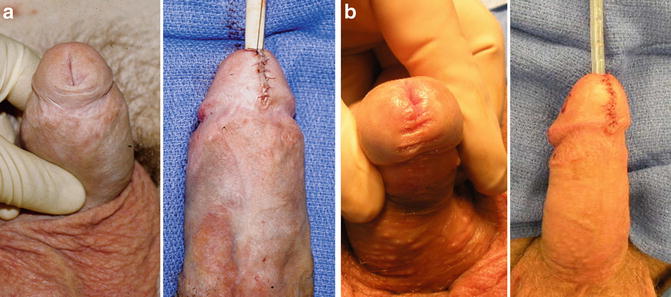
Fig. 4.4
(a) Urine spraying: GAP repair. (b) Suture tracts: glans sculpting
Questions on the long-term adjustment of patients have now become de rigueur and a number of validated study questionnaires have been developed to follow these patients into adolescence and adulthood to assess the quality of repair and perhaps illustrate the importance of continued follow-up. Unfortunately, not all studies use validated questionnaires and therefore comparing results is problematic. As evidenced by the increasing literature on hypospadias failures presenting in adulthood, hypospadias in childhood has the potential to produce long lasting effects well into adulthood.
When reviewing studies on long-term patient-centered outcomes, it is important to consider the timeline in which the repairs were performed. Older techniques have historically worse outcomes and have fallen out of favor, influencing the reported outcomes. Adults and adolescents with subterminal or irregular meatus who had proximal hypospadias repaired during childhood often complain of spraying and angulation of their urinary stream. These patients also commonly note post-void dribbling of urine and the need to milk the ejaculate as the seminal fluid stagnates in the neourethra which lacks spongiosum tissue. In our experience, 116/221 (52.4 %) adolescents and adults with previous hypospadias repair complained of urine spraying and aesthetic concerns. They reported more sexual dissatisfaction as well as dissatisfaction with penile appearance. However, the majority had no difficulty with sexual intercourse except in patients with significant curvature.
In 1989, Bracka published a long-term follow-up of 213 patients with a history hypospadias in childhood of whom 196 had undergone surgery [27]. This landmark study followed patients with questionnaires and physical examinations for those who had a “meatal ventralizing or terminalizing repair” of hypospadias. Patients were assessed for location of meatus, urinary dysfunction, appearance, penile size, sexual behavior and performance adequacy of follow-up and guidance. The impetus for review was based on older reports that patients did not need long-term follow-up after hypospadias repair. The number of procedures required for repair varied from 3.6 to 7.2 with higher numbers in those with “short urethra” and proximal hypospadias. On review, many of the patients had a sub-glandular meatus, which Bracka theorized was due to retraction during growth. Not surprisingly, these patients also reported more spraying on the questionnaire. 38 % of patients reported feeling deformed and 72 % felt appearance was just as important as function. When asked about understanding of their condition, a surprising 60 % had never heard of hypospadias and the Bracka postulated that ignorance of their condition caused further social anxiety. In fact, on further review 44 % of patients requested further surgery for dissatisfaction with stream, appearance, residual curvature, or stricture. In 181 patients who had reached sexual maturity, 1/3 felt inadequate about the size of the penis and in those who underwent proximal hypospadias repair penile length was shorter in flaccid, stretched and erect position compared to the more distal repairs. While 77 % reported having had satisfactory sexual intercourse, ejaculatory complaints predominated with 33 % of patients reporting dribbling ejaculation and 4 % dry ejaculate.
Mureau et al. [28] reported outcomes in 116 patients who underwent hypospadias repair between 1960 and 1992 at two different hospitals. The patients were compared to a group of 88 controls who had undergone inguinal hernia repair. A semistructured interview was performed in boys with an average age of 14.4 years vs. 13.9 years for controls. Patients with hypospadias were more likely to have anxiety and inhibition in seeking sexual contact and 25 % were dissatisfied with penile appearance. The severity of hypospadias or number of surgical procedures did not seem to differ between the groups. However, 19 % of patients in whom surgery was performed after 6 years of age were less satisfied with the surgical result and had a worse genital view than the younger children. Older boys at the time of study (13–18 years) were less satisfied with appearance than their younger counterparts (9–12 years), 31.6 % vs. 13.2 %, respectively. Overall, 39 % patients expressed desire for further correction. The importance of early hypospadias surgery was reiterated by Jones et al. [29] who demonstrated that using validated questionnaire, Hypospadias Objective Scoring Evaluation (HOSE) 80 % of patients had excellent surgical outcome. They concluded that when surgery was completed before age 5 years, boys had no preoperative memories. An association was found between no recollection of surgery and satisfaction with body appearance. The HOSE scheme comprises five domains including meatal location, meatal shape, urinary stream, curvature at erection and fistula.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




