CHAPTER 116 Appendicitis
HISTORICAL PERSPECTIVE
The first anatomic mention of the appendix was made by Leonardo da Vinci in the early 15th century. The first clearly recognizable case report of appendicitis was recorded in 1711 by the German surgeon Lorenz Heister,1 but it was not until 25 years later that the first inflamed appendix was removed by Claudius Amyand, a Sergeant Surgeon to Queen Ann, King George I, and King George II. Amyand operated on an 11-year-old boy with a perforated appendix within a scrotal hernia that he was able to excise and repair, respectively.2 Throughout the 18th and 19th centuries, the prevailing medical opinion was that acute abdominal pain and right lower quadrant inflammation was a consequence of inflammation of the cecum or its surrounding tissues. The modern description of the pathophysiology of appendicitis and the role of the appendix in acute abdominal syndromes dates to 1886, the year Reginald Fitz presented a paper to the Massachusetts Medical Society in which he coined the term appendicitis and espoused early surgical intervention as its appropriate treatment.1
The first now-customary appendectomy for classic acute appendicitis actually had been performed by Lawson Tait in 1880, but it was not reported until Charles McBurney, one of the great contributors to our understanding of appendicitis, published his recommendation for early laparotomy for the treatment of appendicitis in 1889.4 It is in this paper that what subsequently became known as McBurney’s point is described as the point of “maximum tenderness, one half to two inches inside the right anterior spinous process of the ilium on a line drawn from the umbilicus.”2,3
Almost a century later, the first laparoscopic approach to appendectomy was described by Kurt Semm,4 and with development of natural orifice transluminal endoscopic surgery (NOTES), the first successful transvaginal appendectomy was reported by Sanntiago Horgan and Mark A. Talamini in early 2009.5
EPIDEMIOLOGY
Appendicitis is the most common acute abdominal emergency seen in developed countries. The crude incidence rate of appendicitis in the United States for all age groups is 11/10,000 persons per year,6 and similar rates are noted in other developed countries. Inexplicably, the rates of appendicitis are as much as 10 times lower in many less-developed African countries.7 The incidence rate of the disease peaks between 15 and 19 years of age at 48.1/10,000 population per year and falls to about 5/10,000 population per year by age 45 years, after which it remains constant.6 Men are at greater risk than women, with a case ratio in most series of 1.4 : 1. The lifetime risk of appendicitis has been estimated at 8.6% in men and 6.7% in women.6
Approximately 250,000 appendectomies are performed each year in the United States; data from most developed countries suggest that the incidence of appendicitis is decreasing. Between 1989 and 2000, a 15% decrease in the overall incidence of appendicitis was noted in an English study8; similar trends have been noted in Canada and Greece.9,10 One paper, however, suggests that, at least in the United States, the number of appendectomies performed for acute appendicitis has been increasing since 1995.11 Regardless of the direction of the epidemiologic trend, appendicitis remains the most common indication for emergency abdominal surgery.
ANATOMY AND EMBRYOLOGY
The vermiform appendix and the cecum are best thought of as a single anatomic unit. Developmentally part of the midgut, the appendix and cecum form between the 8th and 12th weeks of gestation as a bud arising from the midgut loop, before the ascending colon has become delineated. Congenital malformations of the appendix such as agenesis and duplication are very rare. With an average length of 9 cm,12 the origin of the appendix varies and the appendix may assume any of the positions of a clock hand, with the center considered the appendiceal origin.
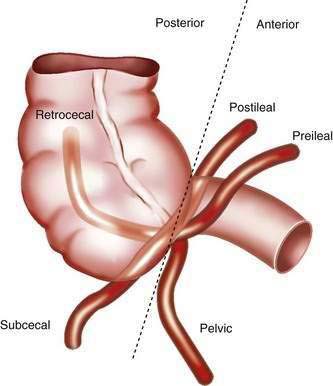
Although the right colon is fixed in the retroperitoneum, the appendix and cecum have a more variable position within the abdomen. The position of the appendix depends upon a number of factors: the degree of cecal descent and peritoneal fixation, the configuration of the cecum, appendiceal length, associated adhesions, and the habitus of the person.13 Typically, the location of the appendix is described as retrocecal, pelvic, subcecal, or para-ileal (Fig. 116-1). The position of the appendix has important clinical implications: For example, the classic progression of symptoms requires irritation of the parietal peritoneum by a mobile appendix; as many as 60% of people have a retrocecal or pelvic-positioned appendix, resulting in an atypical clinical presentation of acute appendicitis.
The classic surface anatomy of the appendix was described by McBurney in 1889, and as mentioned earlier, McBurney’s point is located at the junction of the lateral and middle thirds of a line drawn from the right anterior superior iliac spine to the umbilicus.4 Classically, this surface marking has been important in both the diagnosis and treatment of acute appendicitis; however, investigators have shown that the appendix is located within 5 cm of McBurney’s point in less than 50% of the cases.14 This anatomic finding helps explain why pain or tenderness located at McBurney’s point is not found in all cases of appendicitis.
PATHOLOGY
Acute appendicitis is classified as acute, gangrenous, or perforated. The earliest gross findings of acute appendicitis are injection of the serosal blood vessels and edema of the appendiceal wall. In more-advanced cases, the serosal surface appears dull and is covered by fibrinopurulent exudates. Over time, focal areas of gangrene develop, marked by greenish and black discoloration of the wall; with perforation, focal necrosis of the appendiceal wall develops and adjacent abscesses form.15
Microscopically, each of these forms of appendicitis has distinctive characteristics. In acute or suppurative appendicitis, a neutrophilic infiltrate involves the muscularis propria layer circumferentially, accompanied by acute inflammation and ulceration of the mucosa, edema and microabscesses in the appendicular wall, and vascular thrombosis. The hallmarks of gangrenous appendicitis are transmural inflammation of the appendix with focal areas of mural necrosis. Vascular thrombosis is more prominent in gangrenous than in suppurative appendicitis. The presence of mucosal inflammation alone (“catarrhal” inflammation) is more characteristic of infectious enteritis or colitis and is not considered evidence of acute appendicitis; for the microscopic diagnosis of appendicitis to be made, inflammation must extend to the muscularis propria.15
PATHOGENESIS
Despite more than 100 years of study, there still is no single explanation for all cases of appendicitis. The classic hypothesis is that obstruction of the appendiceal lumen by either a fecalith or lymphoid hyperplasia produces an increase in intraluminal pressure, which in turn results in venous hypertension, ischemia of the appendiceal wall, and subsequent bacterial invasion of the appendix with necrosis and perforation. Experimental evidence in animal models exists to support this hypothesis of the etiology of acute appendicitis.16 This hypothesis, however, does not explain all cases of appendicitis. Careful review of pathologic series shows that luminal obstruction is found in a minority of cases. Fecaliths are present in only 8% to 44% of cases of acute appendicitis, with most series at the lower end of the range,15,17 and lymphoid hyperplasia is more common in noninflamed appendices than in acute appendicitis.18 Other causes of luminal obstruction such as foreign bodies, tumors, and fibrous bands are uncommon. Direct measurement of intraluminal pressure at appendectomy for appendicitis reveals an elevated pressure in only a minority of cases.19
An alternative hypothesis for the etiology of appendicitis is based on the concept that either bacterial or viral enteric infection leads to mucosal ulceration of the appendix and subsequent bacterial invasion from the normal colonic flora. The finding that up to 75% of cases of appendicitis demonstrate well-defined superficial mucosal ulceration supports this theory. Furthermore, mucosal ulceration is a more consistent finding than dilatation of the appendix or fecaliths and is found earlier in the course of appendicitis.20 One report found human cytomegalovirus (HCMV) early antigen expression in 64% of cases with acute appendicitis and no HCMV antigens in normal appendices, suggesting that in some cases CMV, infection might produce mucosal ulcerations leading to acute appendicitis.21
Additional support for the role of infection in the etiology of appendicitis is found in two lines of epidemiologic evidence. The first is based in the hygiene theory of appendicitis advocated by Barker in the mid 1980s.22 According to this hypothesis, changes in sanitation tied to the Industrial Revolution resulted in a decrease in enteric infections in infants, with subsequent decreased immunity to the same infections in childhood and young adulthood. Acquisition of these infections later in life was believed to predispose people to appendicitis, explaining the rise in the incidence rates of appendicitis in the first half of the 20th century. The decrease in the overall rate of enteric infections during the last half of the 20th century explains the overall decline in appendicitis. The second line of epidemiologic evidence supporting the role of infection in the etiology of appendicitis is the seasonal variance in incidence of appendicitis and the occurrence of temporal and spatial clusters of appendicitis, both hallmarks of infectious diseases.23 It is important to recognize, however, that no specific infectious agent has been linked with all cases of appendicitis, suggesting that infection is not the complete story.
A decrease in dietary fiber intake (the fiber hypothesis) also has been proposed as a cause of appendicitis. According to this hypothesis, decreased dietary fiber causes firm stool and an increased enteric transit time, resulting in more fecaliths and more appendicitis. This hypothesis was felt to explain both the rise in appendicitis rates in the early 20th century and the marked differences in appendicitis rates between more-developed Western countries and less-developed African countries. Doubt has been cast upon this hypothesis, however, for several reasons. First, although dietary fiber ingestion has been falling in urban Africans, appendicitis rates have not risen markedly.24 Second, rates of appendicitis in the Western world have fallen without changes in dietary fiber intake. Finally, a prospective series from Africa demonstrated continued high fiber intake even in patients with appendicitis.25
CLINICAL FEATURES
A detailed history and careful physical examination remain cornerstones of the diagnosis of acute appendicitis. Although no single item of the history, in isolation, allows the diagnosis to be made reliably, combination of the classic symptoms and the typical progression of symptoms coupled with right lower quadrant tenderness allows good diagnostic accuracy. In the classic presentation of acute appendicitis, patients first note vague, poorly localized epigastric or periumbilical discomfort, which typically is not severe and often is attributed to “gastric upset.” Patients commonly report feeling that a bowel movement should make the pain better, a sensation known as the downward urge.26
Diarrhea sometimes is seen early on with appendicitis, but this is not common. Within 4 to 12 hours of the onset of pain, most patients also note nausea, anorexia, vomiting, or some combination of these three symptoms. The nausea usually is mild to moderate, and most patients have only a few episodes of emesis. If vomiting is the major symptom, the diagnosis of appendicitis should be questioned. Likewise, emesis that occurs before the onset of pain should suggest other diagnoses.27 Many patients report a mild fever or chills; high fevers or significant rigors are uncommon. The patient’s abdominal pain typically increases in intensity, and a characteristic shift in the pain to the right lower quadrant occurs over 12 to 24 hours. The character of the pain becomes achy and more localized. Localization of the pain to the right lower quadrant is a valuable finding when present and occurs in more than 80% of patients with appendicitis.27
On physical examination, most patients appear slightly ill. Tachycardia is uncommon with simple appendicitis, but it may be seen with complicated appendicitis. Most patients with simple appendicitis have a temperature less than 100.5°F; temperature greater than 100.5°F is most often associated with perforated or gangrenous appendicitis.17 Patients with appendicitis, like other patients with peritonitis, tend to lie still rather than move about. Right lower quadrant tenderness and rigidity, both voluntary and involuntary, are common findings. Localized right lower quadrant tenderness is an important finding when present, but its absence does not rule out appendicitis. A variety of methods exist to elicit localized right lower quadrant peritonitis, including the cough sign (the presence of point tenderness with a cough), percussion tenderness, and formal elicitation of rebound tenderness. Although all of these techniques are reasonably sensitive, one small study showed rebound tenderness to be the most accurate predictor of the localized peritonitis associated with appendicitis.28
Additional findings that may be helpful in diagnosing appendicitis include the psoas sign, the obturator sign, Rovsing’s sign, and rectal tenderness. The psoas sign is sought by having a supine patient actively flex the right hip against resistance, or by the examiner flexing and extending the patient’s right hip with the patient in the left lateral decubitus position. Pain with either of these maneuvers is thought to result from irritation of the underlying psoas muscle by an inflamed retroperitoneal appendix. The obturator sign is elicited by internally and externally rotating the flexed right hip. Pain is thought to arise when the inflamed pelvic appendix irritates the adjacent obturator internus muscle. Rovsing’s sign is the finding of right lower quadrant pain during palpation of the left side of the abdomen or when left-sided rebound tenderness is elicited. All of these findings are valuable when present, but their absence does not exclude appendicitis.27
Appendicitis in infants and young children remains a difficult diagnostic challenge because of difficulties in obtaining an accurate history. In young patients, the characteristic history of pain is difficult to elicit, and nonspecific findings of vomiting, lethargy, and irritability tend to predominate. Physical examination is difficult to perform because of poor patient cooperation and because localized right lower quadrant tenderness is found in less than 50% of patients.29 In addition, the characteristic laboratory findings often are not present. Leukopenia is as common as leukocytosis in young infants.30 As a result, errors in diagnosis are common, and the frequency of complicated appendicitis is as high as 40% to 70%.31
The diagnosis of appendicitis in elderly patients also may be a challenge. In the elderly, the classic pattern of pain migration, right lower quadrant tenderness, fever, and leukocytosis are observed in only 15% to 30% of cases.30,32 Older patients also tend to present to medical attention in a delayed time frame relative to younger patients. For all of these reasons, the complication and perforation rates can be as high as 63% in patients older than 50 years.33
The presentation of appendicitis during pregnancy also is associated with an atypical clinical presentation, particularly in the later stages of pregnancy. In one series, only 57% of pregnant women with appendicitis had the classic progression of pain.34 Nausea and vomiting tend to be more common in pregnant women with appendicitis, but they also are common occurrences during normal pregnancy. Fever and leukocytosis are less commonly seen in pregnant woman than in other patient groups, and the value of leukocytosis is obscured by the physiologic leukocytosis of pregnancy. Although right-sided abdominal pain and tenderness are found in more than 90% of pregnant women with appendicitis, pain is located in the right lower quadrant only 75% of the time.34
Immunocompromised patients in general, and patients with AIDS in particular, represent a challenging group in which to diagnose appendicitis. Abdominal pain is reported in 12% to 45% of AIDS patients with appendicitis. The range of diagnoses responsible for this pain is significantly greater than in patients without HIV and includes opportunistic infections and malignancies, although in most cases, the pain is related to a diagnosis not associated with HIV.35 Research suggests that appendicitis occurs more often in HIV-infected patients than in HIV-negative patients, with as much as a four-fold increase in incidence.36 Although patients with AIDS usually present with the classic symptoms of appendicitis, there often is a history of chronic abdominal pain. Diarrhea also is a more common presenting symptom of appendicitis in HIV-positive patients, and leukocytosis is relatively uncommon. Declining CD4 counts are associated with delays in presentation to medical attention and increased perforation rates.37 Despite the challenges of diagnosing appendicitis in patients with HIV, the surgical outcomes with appropriate treatment are quite good; the largest series to date had no mortalities and a 13% complication rate, which is comparable to outcomes in patients without HIV.37
DIAGNOSIS
Diagnosis of appendicitis remains a significant clinical challenge because of the many different entities that manifest with acute abdominal pain and the relatively nonspecific initial presentation of the disease. Because the natural history of appendicitis is a time-dependent progression to perforation, there is some urgency in making a prompt and accurate diagnosis. Not all causes of acute abdominal pain, however, require surgical intervention, and a negative appendectomy carries some risks for the patient, including adhesion formation, infection, and postoperative disability. Table 116-1 illustrates common diagnoses that can mimic acute appendicitis. Compounding this diagnostic challenge, there is no single symptom, finding, or laboratory test that is completely sensitive or specific for appendicitis.27
Table 116-1 Differential Diagnosis of Appendicitis
| DIAGNOSIS | FINDINGS THAT HELP DIFFERENTIATE FROM APPENDICITIS |
|---|---|
| Bacterial or viral enteritis | Nausea, vomiting, and diarrhea are severe; pain usually develops after vomiting |
| Mesenteric adenitis | Duration of symptoms is longer; fever is uncommon; RLQ physical findings are less marked; WBC count is usually normal |
| Pyelonephritis | Pain is more likely to be felt in the right flank; high fever and rigors are common; marked pyuria or bacteriuria and urinary symptoms are present; abdominal rigidity is less marked |
| Renal colic | Pain radiates to the right groin; significant hematuria; character of the pain is clearly colic |
| Acute pancreatitis | Pain and vomiting are more severe; tenderness is less well localized; serum amylase and lipase levels are elevated |
| Crohn’s disease | History of similar attacks; diarrhea is more common; palpable mass is more common; extraintestinal manifestations may occur |
| Cholecystitis | History of prior attacks is common; pain and tenderness are greater; radiation of pain is to the right shoulder; nausea is more marked; liver biochemical tests are more likely to be abnormal |
| Meckel’s diverticulitis | Very difficult to distinguish preoperatively from appendicitis |
| Cecal diverticulitis | Difficult to distinguish preoperatively from appendicitis; symptoms are milder and of longer duration; CT scan is helpful |
| Sigmoid diverticulitis | Usually occurs in older patients; changes in bowel habits are more common; radiation of pain is to the suprapubic area, not RLQ; fever and WBC count are higher |
| Small bowel obstruction | History of abdominal surgery; colicky pain; vomiting and distention are more marked; RLQ localization is uncommon |
| Ectopic pregnancy | History of menstrual irregularities; characteristic progression of symptoms is absent; syncope; positive pregnancy test |
| Ruptured ovarian cyst | Occurs in the middle of the menstrual cycle; pain is of sudden onset; nausea and vomiting are less common; WBC count is normal |
| Ovarian torsion | Vomiting is more marked and occurs at the same time as the pain; progression of symptoms is absent; abdominal or pelvic mass often is palpable |
| Acute salpingitis or tubo-ovarian abscess | Longer duration of symptoms; pain begins in the lower abdomen; often there is a history of STDs, vaginal discharge, and marked cervical tenderness often are present |
CT, computed tomography; RLQ, right lower quadrant; STD, sexually transmitted disease; WBC, white blood cell.
LABORATORY STUDIES
Laboratory findings in acute appendicitis include a variety of markers of acute inflammation. An elevated white blood cell count (WBC) in the range of 11,000 to 17,000/mm3 is seen in approximately 80% of patients, but the specificity of this finding for acute appendicitis versus other causes of acute abdominal pain is poor.38 An elevated proportion of granulocytes in the total white count or an elevated total neutrophil count (left shift) also is seen in the vast majority of patients with appendicitis, but is not specific for appendicitis.38 C-reactive protein (CRP), an acute phase reactant synthesized by the liver, is thought to rise within 12 hours of the development of an acute inflammatory process. Although CRP is elevated in 50% to 90% of cases of appendicitis, CRP is nonspecific when cutoff values of 5 to 25 mg/L are used.39 A urinalysis often is obtained in patients with acute appendicitis to exclude urinary tract infections, but mild abnormalities, either pyuria or hematuria, are present in about 50% of cases of appendicitis.40
The value of laboratory investigations in diagnosing acute appendicitis has been a matter of some debate. In patients with a classic presentation by history and physical examination, many authors think that little additional information is obtained from laboratory studies. When all cases of appendicitis are considered, however, adding laboratory studies such as WBC, left shift, and CRP has been shown to improve diagnostic accuracy.41 When clinical findings are compared with inflammatory markers, inflammatory markers are stronger predictors of appendicitis than individual history or physical findings. Direct comparison of WBC and CRP suggests that total WBC or total granulocyte count is more sensitive and accurate than CRP for detecting acute appendicitis.39,41 The diagnostic performance of inflammatory markers is even better in identifying patients with perforated appendicitis.
All patients with suspected acute appendicitis should have a CBC. A pregnancy test should be obtained in women of childbearing age. The value of other laboratory tests such as amylase, liver biochemical tests, or urinalysis lies in helping to exclude other diagnoses that can mimic acute appendicitis (see Table 116-1).
IMAGING STUDIES
Traditionally, there has been little role for routine imaging studies in patients with suspected acute appendicitis. As is stated in the classic text Cope’s Early Diagnosis of the Acute Abdomen, “Over reliance on laboratory tests and radiological evaluations will very often mislead the clinician, especially if the history and physical examination are less than diligent and complete.”28,27 In 50% to 60% of cases, the diagnosis of appendicitis requires no imaging studies and can be made on clinical grounds alone.42,43 When diagnosis is less certain, a variety of imaging tests has been used to help confirm or exclude the diagnosis of acute appendicitis: plain abdominal films, abdominal ultrasound, radionuclide scans, and abdominal and pelvic computed tomography (CT).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree