Fig. 7.1
Patient setup. Patient is placed in the split-leg position for most cases. In cases requiring a synchronous perineal approach such as an intersphincteric dissection, the patient is placed in the modified lithotomy position
1.
Exposure to the anus/rectum for intraoperative colonoscopy if needed. This can be particularly useful for a tumor not preoperatively tattooed and localized or when colonoscopy and laparoscopy are used together as adjuncts for resection-sparing colonic polypectomy.
2.
In inflammatory disease processes such as Crohn’s, an occult fistula may not be appreciated despite preoperative imaging until intraoperative exploration. Operative intervention may then necessitate both right- and left-sided mobilization as well as possible utilization of per-anus anastomotic stapling device.
3.
Operator positioning between the legs during more difficult dissections.
Depending upon the surgeon’s robot docking schema, split-leg positioning may not be feasible. Familiarize yourself with side (parallel) and pelvic docking to ensure appropriate case-specific robot positioning. Both docking positions are utilized in pelvic dissection; however, for right or left colectomies, including low anterior resections, the side docking position is preferred. Room layout is crucial to provide adequate space for the entire operative team, which facilitates docking and undocking of the robot. Carefully planned operative layout and robot docking allow for efficient, effective docking. Although studies demonstrate increased operative times with robotics versus laparoscopy, most added time comes from docking the system. These times can be significantly reduced with appropriate team development, planning, and practice [5, 6].
Robotic-assisted surgery is an enhanced version of laparoscopy, and as such, port placement is vital. If ports are inappropriately placed, exposure and anatomic definition is inferior. Additionally, instrument collision due to poorly placed ports will significantly hinder progression of the case. The current Si da Vinci robot has excelled in urology and gynecologic surgery due to superiority when focused on single quadrant surgery, in particular the pelvis. Colorectal surgery differs from those specialties as it often requires multi-quadrant dissection. The current da Vinci models are somewhat bulky with arms that often collide when moving from one quadrant to another. Several schemata have been recommended for right and left colectomies as well as pelvic dissections; however, port placement will vary based on the surgeons’ preferred approach and technique.
After prepping and draping, diagram your proposed port placement on the abdomen as a guideline. Following insufflation, port placement is confirmed or adjusted based on pneumoperitoneum. Remember, if you have extra body surface area to space ports out, use it to avoid collisions. Entrance to the abdomen is completed via open (Hasson), optiview, or closed (Veress) technique per the operating surgeon’s preference. Our preference is to place a 12-mm camera port 2 cm cranial and 2 cm right lateral from the umbilicus for left-sided dissections or supraumbilical in right-sided dissections. A supraumbilical port can be used for left-sided dissections, as diagrammed in placement schema (Figs. 7.2, 7.3, 7.4, and 7.5). A 5-mm laparoscopic camera, 8-mm robotic camera, or 12-mm robotic camera can be used to complete intraperitoneal diagnostic exploration and guide robotic instruments into the peritoneal cavity. An initial laparoscopic overview is performed in every procedure. We argue its elevated importance in robotic-assisted colon surgery for several reasons. Firstly, the surgeon must inspect the abdomen and pelvis for evidence of (1) occult metastatic disease, (2) altered anatomy, or (3) inability to safely perform the procedure with robotic assistance. Secondly, the surgeon can evaluate port placement and anatomical markings and determine if robotic assistance will benefit or harm the operation. The larger robotic camera is quite cumbersome and heavy, not to mention costly to repair if dropped, so we discourage its use for this portion of the case. In contrast, the opening of a 5-mm laparoscope and other laparoscopic equipment may add unnecessary cost to the procedure. By avoiding the use of unnecessary equipment, expenses are lowered. We prefer to utilize the 5-mm laparoscopic camera as it is easier to maneuver, especially when visualizing ports in the upper quadrants. Once all ports are placed, the camera visualizes careful insertion of robotic instruments, all pointed toward the pelvis.
Fig. 7.2
Three-arm technique for robotic right colectomy. Extraction site is through the midline or surgeon preference
Fig. 7.3
Four-arm technique for robotic right colectomy. Extraction site is through the midline or surgeon preference
Fig. 7.4
Port placement for a robotic low anterior resection. When approaching the splenic flexure, arm #3 is moved from the left side of the abdomen to the right side. Arm #2 is undocked to avoid unnecessary collisions
Fig. 7.5
Port placement for a robotic sigmoidectomy. Notice that the camera port is slightly off midline. This allows dissection of the splenic flexure and upper pelvis utilizing arm #3 (which is also moved slightly more medial)
PEARL: As with all minimally invasive techniques, placement of ports and instruments into the peritoneal cavity is performed under direct vision in order to minimize unnecessary injury to the underlying viscera.
7.3 The Right Colon
7.3.1 Brief Anatomy Review
The right colon is supplied by the ileocolic artery branching off the superior mesenteric artery, which travels just infero-caudally to the third portion of the duodenum. The ileocolic artery is present in 100 % of patients, while the middle colic artery is present in 98 % of patients. In contrast, the typically depicted right colic artery branching off the superior mesenteric artery actually only occurs in 11 % of cases (Fig. 7.6). Often, the distal right colon is perfused by the middle colic vessel. The middle colic vessel is also the primary blood supply to the proximal two-thirds of the transverse colon. It branches off the superior mesentery artery just inferior to, and then overlies, the pancreas (Fig. 7.7a). The common middle colic artery is very short, quickly branching into a left and right vessel, giving it the classic “Y” appearance upon retraction of the transverse colon mesentery ventrally (Fig. 7.7b). When dissecting the right branch of the middle colic artery, one must also consider the right branch of the middle colic vein. The middle colic vein may give a communicating branch to the gastroepiploic vein which courses behind the transverse colon mesentery. When mobilizing the transverse colon mesentery, this communicating or bridging vein can be disrupted causing difficult to control hemorrhage.
Fig. 7.6
The ileocolic artery is present in 100 % of patients; the right colic artery most commonly arises from the ileocolic artery rather than the SMA. With permission from Landmann RG and Francone T. Surgical Anatomy. In: Minimally Invasive Approaches to Colon and Rectal Disease: Techniques and best practices. Ross HM, Lee SW, Mutch MG, Rivadeneira DE, Steele SR. Springer, New York, 2015: pp. 25–50
Fig. 7.7
(a) Superior mesenteric artery and its branches. (b) Note the typical “Y” appearance of the middle colics. With permission from Landmann RG and Francone T. Surgical Anatomy. In: Minimally Invasive Approaches to Colon and Rectal Disease: Techniques and best practices. Ross HM, Lee SW, Mutch MG, Rivadeneira DE, Steele SR. Springer, New York, 2015: pp. 25–50
After completion of diagnostic laparoscopy, the patient is placed in slight Trendelenburg position combined with left inclination. It is often beneficial to limit the amount of Trendelenburg incline with robotic surgery such that positioning does not favor exposure to one quadrant and limit it in another. This is particularly critical when performing a robotic splenic flexure mobilization, where too much Trendelenburg can prevent adequate exposure in the left upper quadrant but superb exposure in the pelvis. The camera port and the arm #1 port are typically placed first to position the patient and assess case feasibility. The surgeon retracts the omentum superiorly over the transverse colon, along with mobilizing the small bowel out of the pelvis and into the left upper quadrant. Once completed, additional ports are inserted under direct visual guidance. With the patient positioned in the split-leg position, the robot is docked over the patient’s right chest. A three- or four-arm technique can be used to perform the right colectomy (Figs. 7.2 and 7.3). In the four-arm technique, arm #3 is typically an assistant port used to hold up mesentery or omentum for facilitation of dissection. Arms #1 and #2 are utilized more frequently to perform dissection, either lateral to medial or vice versa.
7.3.2 Lateral to Medial Dissection
This approach is generally the easier dissection to learn and perform. There are several critical anatomic landmarks that once appreciated can lead to a safer, more expedient, and appropriate oncologic resection (sometimes termed total mesocolic excision). With the exclusion of a right colectomy for pathological enlargement of the appendix (i.e., mucocele, cystadenoma, cystadenocarcinoma, or carcinoid), grasping this tubular structure can help significantly in retraction. Otherwise, either the terminal ileum or cecum can be gently and carefully grasped to mobilize the enteral structures anteriorly and toward the left upper quadrant. Arm #3 is typically utilized to grasp and retract the mesentery leftward in a ventral and cephalad direction, exposing the lateral attachments of the colon and mesentery to the retroperitoneum (white line of Toldt). Division of this attachment allows entry into a loose alveolar plane, whereby dissection can proceed distally along the ascending colon to the hepatic flexure. Arm #1 or #2 may be used for this portion of the procedure depending on exposure and surgeon preference. At the ileocecal valve, care is taken to identify and preserve the ureter as it crosses the right iliac artery bifurcation (Fig. 7.8). Further care is taken to stay within the appropriate plane as straying laterally leads to dissection of Gerota’s fascia with subsequent medial mobilization of the kidney.
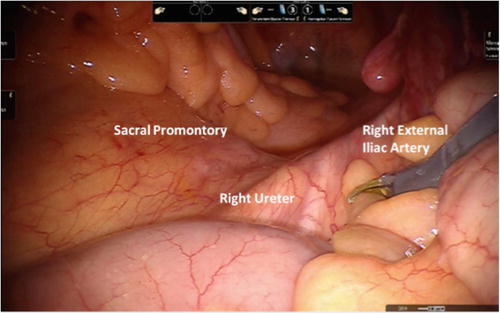
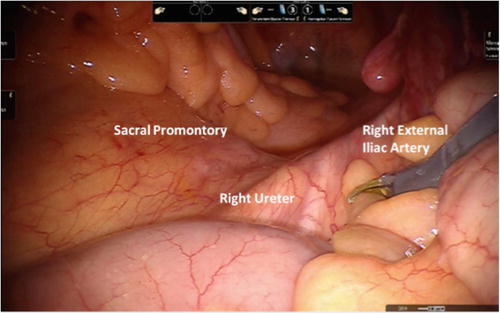
Fig. 7.8
The right ureter enters into the pelvis slightly more lateral crossing over the right external iliac artery
Mobilization within the correct plane of the mesocolon from the retroperitoneum centrally (or medially) toward the takeoff base of the ileocolic pedicle will expose the anterior surface of the duodenum and pancreas. The mesentery of the terminal ileum is then divided from the retroperitoneum to the level of the right iliac artery. At this point, the base of the ileocolic pedicle is easily visualized and divided using energy (vessel sealer), stapler, or clips. When using a vessel-sealing device, the authors suggest having an endoloop or clips readily available should bleeding ensue.
7.3.3 Medial to Lateral Dissection
The key to a proficient medial to lateral dissection, using either laparoscopic or robotic approach, is entry into the avascular plan between the colonic mesentery and the retroperitoneum. Before beginning, the surgeon should make an attempt to identify the pertinent anatomy (ileocolic pedicle, ureter, and duodenum) involved in dissection to prevent untoward events. This is often easier in thinner patients than the morbidly obese where identification of the duodenal sweep or C-curve can be observed with superoanterior retraction of the transverse colon. Carefully grasping the cecum, or its mesentery, close to the base and lifting toward the anterolateral abdominal wall display the ileocolic artery coursing infero-caudally to the duodenum (Fig. 7.9). This motion creates a tenting or “bowstring” effect with a distinct crease coursing parallel to the vessel (Fig. 7.10). Arm #3 can be used for cecal retraction, freeing arms #1 and #2 to develop the correct plane. Care is taken with the robot to not avulse vessels due to lack of haptic feedback. Once bowstringing is noted, the peritoneum is scored parallel to the vessel, allowing pneumoperitoneum to fill the avascular space and facilitate development of the appropriate plane. Some mobilization of the mesocolon from the retroperitoneal structures may be necessary and can be performed with gentle, blunt sweeping motions dorsally. Particular attention must be given medially and posteriorly where the C-loop of the duodenum lies and can be easily injured with the dissecting instrument or energy device (Fig. 7.11a, b). When in the correct plane, it is generally not necessary to identify the ureter or iliac vessels located in the inferolateral aspect of the dissection. However, in the presence of penetrating disease, either benign with perforating Crohn’s disease or malignant with penetrating neoplastic mass, the surgeon must be aware of the surrounding anatomy.
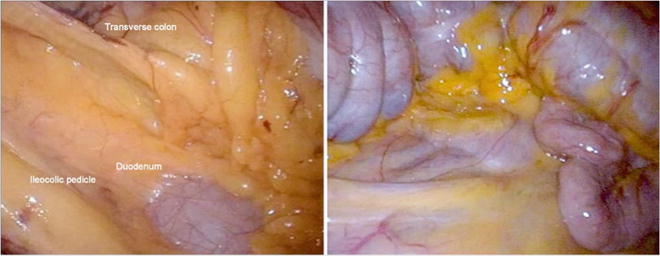
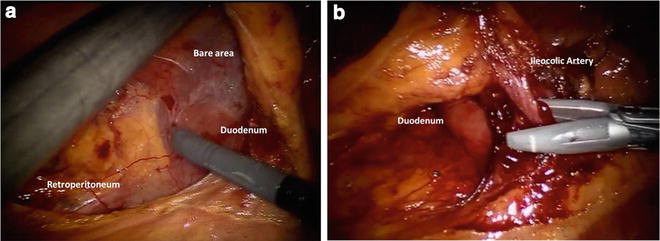
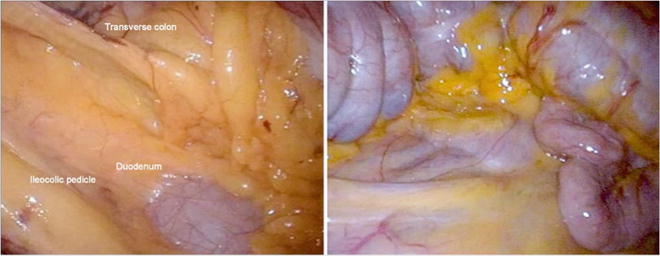
Fig. 7.9
The ileocolic artery courses infero-caudally to the duodenum; in thinner patients, the duodenal sweep can often be identified prior to the initiation of the dissection. With permission from Landmann RG and Francone T. Surgical Anatomy. In: Minimally Invasive Approaches to Colon and Rectal Disease: Techniques and best practices. Ross HM, Lee SW, Mutch MG, Rivadeneira DE, Steele SR. Springer, New York, 2015: pp. 25–50
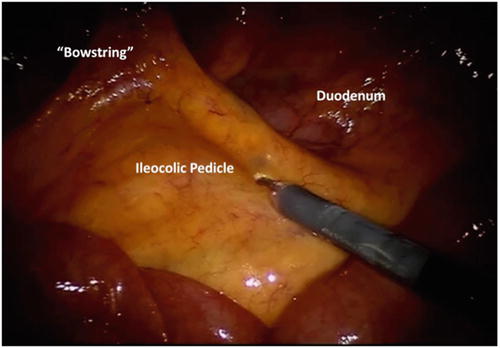
Fig. 7.10
Grasping the cecum or its mesentery and lifting anterolateral to the abdominal wall will create a tenting or “bowstring” effect with a distinct crease coursing parallel to the vessel
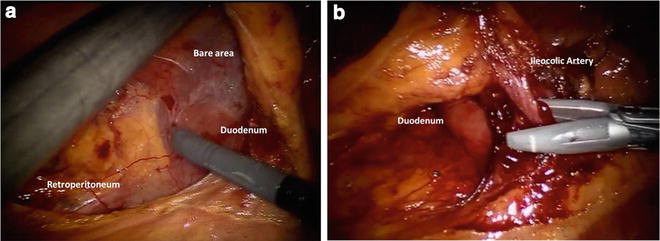
Fig. 7.11
(a) Medial dissection is initiated by sweeping the retroperitoneum down and away; immediate identification of the duodenum is critical in order to avoid injury. (b) When dividing the ileocolic artery, the surgeon must always be mindful of the duodenum
As the avascular plane is developed, there is a consistent thinning out or paucity of adiposity in the mesenteric fat on both sides of the ileocolic pedicle (Fig. 7.10). Careful dissection through this mesentery creates a window around the pedicle at which point the vessel can be divided (Fig. 7.11a). Once critical structures are well visualized and out of harm’s way, a high or central ligation is performed. Surgeon’s preference dictates method of ligation and division, with options including endoscopic stapling devices, energy devices, or application of clips with intermediary division. As noted previously, when using a vessel-sealing device, the authors suggest ready availability of endoloop or clips should bleeding ensue.
PEARL: When dissecting under the ileocolic pedicle, always beware of the duodenum coming into surgical view (Fig. 7.11 b).
Once ligation is completed, medial to lateral dissection continues by careful elevation of the mesentery followed by gentle, blunt sweeping of the retroperitoneum downward. A thin, white line of Toldt is visualized separating mesocolon from retroperitoneal structures (Fig. 7.12). A key point in performing this maneuver is to gently push or sweep the peritoneal reflection line down rather than pull other structures up. In general, arm #3 is stationary and used to retract the mesocolon up, while arms #1 and #2 continue the dissection. If the surgeon maintains the correct plane, risk of bleeding, elevation of the right kidney, and damage to the duodenum should not occur. Difficulty visualizing this plane is often attributable to incomplete maintenance of tension/counter-tension.
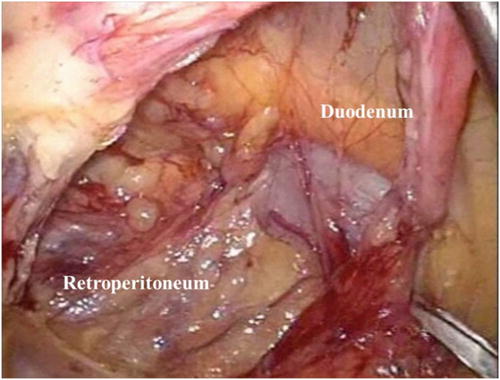
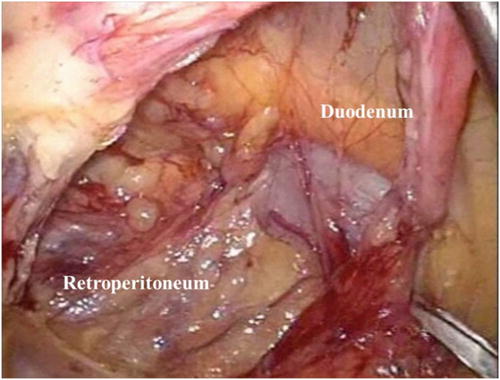
Fig. 7.12
Medial to lateral mobilization highlighting duodenum and white line of Toldt. With permission from Landmann RG and Francone T. Surgical Anatomy. In: Minimally Invasive Approaches to Colon and Rectal Disease: Techniques and best practices. Ross HM, Lee SW, Mutch MG, Rivadeneira DE, Steele SR. Springer, New York, 2015: pp. 25–50
Upon reaching the lateral sidewall, dissection is carried superiorly toward the hepatic flexure. Caution must again be taken as the right colic and the right branch of the middle colic artery may be encountered during this part of the operation. Identification of the middle colic vessels usually occurs with ventral retraction of the transverse colon mesentery. It is often first identified inferior to the pancreas but with further exploration is found to overlie the pancreas with its main branch coming off the superior mesenteric vessel (Fig. 7.13). In both laparoscopic and robotic-assisted procedures, the surgeon must beware of inadvertently disrupting these vessels, especially the pancreaticoduodenal and gastroepiploic branches, which lie close to this region and can result in troublesome bleeding that is difficult to control.
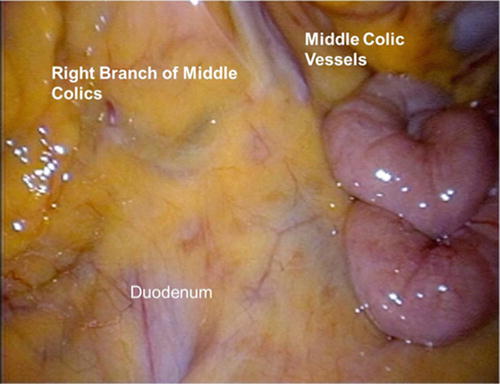
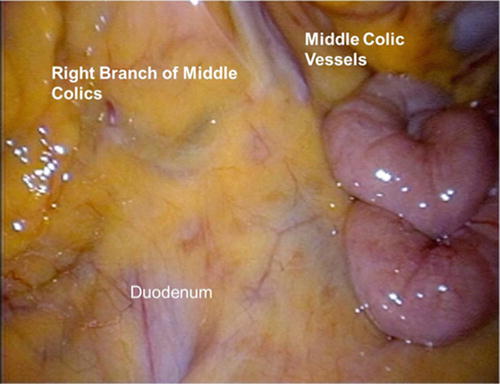
Fig. 7.13
Transverse colon anatomy and middle colic vessels. With permission from Landmann RG and Francone T. Surgical Anatomy. In: Minimally Invasive Approaches to Colon and Rectal Disease: Techniques and best practices. Ross HM, Lee SW, Mutch MG, Rivadeneira DE, Steele SR. Springer, New York, 2015: pp. 25–50
The right branch of the middle colic is often divided during a right colectomy (Fig. 7.14). As mentioned previously, anterosuperior retraction of the transverse colon mesentery often demonstrates the takeoff of the right and left branches from the main branch giving the classic “Y” pattern of the middle colic vessels (Fig. 7.7b). Similar to ligation of the ileocolic pedicle, the right branch of the middle colic is isolated then divided. In addition, the right colic vein may also be visualized in this area, lateral to the right branch of the middle colic and coursing from the pancreas toward the hepatic flexure. If encountered, this vessel should be carefully ligated to prevent bleeding during completion of right colon mobilization. Once both pedicles are safely controlled, dissection of the mesentery may proceed, ensuring that the terminal ileum and cecal mesentery, as well as the transverse colon mesentery, have been adequately mobilized.
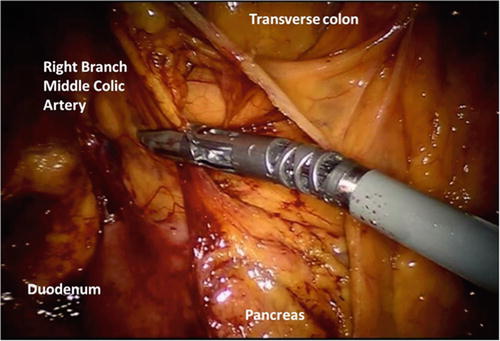
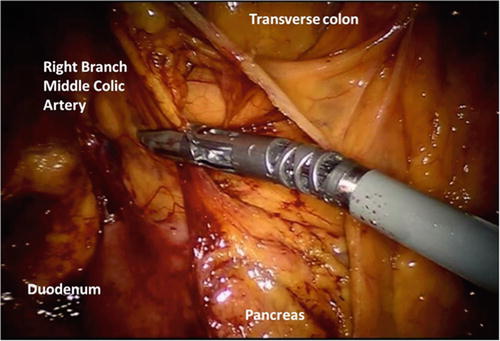
Fig. 7.14
The right branch of the middle colic vessels is often divided during a right colectomy
At this point, the right colon remains affixed by lateral avascular attachments to the abdominal sidewall, hepatic flexure attachments, and gastrocolic attachments of the omentum to the transverse colon. These can generally be easily divided by either a dissecting energy device (ultrasonic or bipolar type) or energized, monopolar cautery/Metzenbaum scissors. It is the authors’ preference to start the dissection at the pelvic brim. The cecum or terminal ileum is gently retracted anteromedially with arm #3, while arms #1 and #2 divide the lateral attachments. Dissection proceeds proximally toward the hepatic flexure. Inferiorly along the terminal ileal mesentery, there is a reflection noted at the attachment to the retroperitoneum (Fig. 7.15). This fold is medial to the ureter, overlies the right iliac vessels in the right pelvis, and is also superolateral to the sacral promontory. If performed appropriately with anterior retraction of the terminal ileum, the surgeon should enter into the previously dissected plane between the mesocolon and the retroperitoneum. Retract the ileum anteriorly, and dissect along this fold to further mobilize the terminal ileal mesentery toward the duodenum and pancreas. Proper mobilization along this plane will ensure adequate small bowel mobilization to reach the transverse colon and perform a tension-free anastomosis.
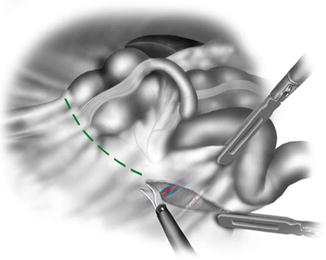
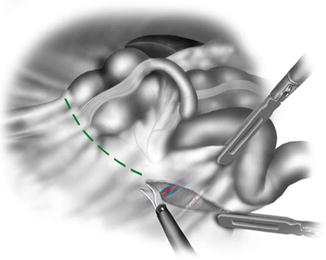
Fig. 7.15
Inferiorly along the terminal ileal mesentery, there is a reflection noted at the attachment to the retroperitoneum. This fold is medial to the ureter, overlies the right iliac vessels in the right pelvis, and is also superolateral to the sacral promontory. With permission from Landmann RG and Francone T. Surgical Anatomy. In: Minimally Invasive Approaches to Colon and Rectal Disease: Techniques and best practices. Ross HM, Lee SW, Mutch MG, Rivadeneira DE, Steele SR. Springer, New York, 2015: pp. 25–50
The hepatocolic and gastrocolic attachments are divided, rendering the right colon a midline structure. Specimen may then be extracted though a midline incision when performing an extraperitoneal anastomosis. For right colectomies, the distal extent of dissection is generally around the falciform ligament or in line with the middle colic vessels. It is often best to start at this point and work retrograde toward the hepatic flexure. With arm #3 retracting the omentum ventrally, arms #1 and #2 dissect into the lesser sac with visualization of the posterior wall of the stomach and colonic mesentery. The key to mobilizing the transverse colon is careful dissection of the omental layers one at a time. At a certain point, the omentum will then be fully mobilized, and attention is directed toward the hepatocolic ligament. An avascular plane is developed between this and the proximal transverse colon mesentery. Caution must be taken when developing the plane as one can easily injure the duodenal sweep lying posteriorly or inadvertently tear the right colic vein. At the level of the gallbladder, the surgeon should expect to enter the previous medial to lateral dissection plane. Where previously dissected planes meet, the surgeon should encounter purple-hued tissue. The lateral attachments can be easily divided with excellent exposure of the surrounding structures. This creates a fully mobilized right colon that easily approaches the midline.
PEARL: Prior to undocking the robot, the surgeon must ensure proper mobility of the specimen, including terminal ileum. If mobility is required, there exists a fold medial to the right ureter and superolateral to the sacral promontory, which signifies an attachment of the terminal ileal mesentery to the retroperitoneum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







