Adrenal Biopsy and Normal Histology
Debra L. Zynger
INDICATIONS
An adrenal biopsy is used for two main diagnostic indications: to characterize an adrenal mass with equivocal imaging findings or to rule-in or ruleout an adrenal metastasis detected in imaging performed for the purpose of staging a previously diagnosed malignancy. Additionally, an adrenal biopsy may be performed in patients with multiple metastases but an unknown primary source of the tumor (Table 9.1) (1). An adrenal mass incidentally identified during abdominal imaging is termed an adrenal incidentaloma (2). With more frequent use of imaging, the incidence of adrenal incidentalomas is increasing (1). Incidentalomas are seen in an estimated 4% of abdominal computerized tomography (CT) scans (3). At autopsy, less than 1% of people younger than the age of 30 years have an adrenal incidentaloma, with a frequency rising to 7% in those older than the age of 70 years (2). Although most of these lesions are benign, in patients with a prior history of malignancy, workup reveals that approximately 75% of adrenal masses are metastases (1,2,4). As imaging does not definitively provide a diagnosis of benign or malignant in some lesions, adrenal biopsy has an established role in the diagnostic approach to these masses (2).
PREBIOPSY STUDIES AND BIOPSY TECHNIQUE
Imaging to identify and characterize the adrenal gland includes CT, magnetic resonance imaging (MRI), nuclear medicine studies, and ultrasonography (eFig. 9.1). CT is the primary imaging modality for the adrenal. An adrenal CT protocol uses early and delayed contrast enhancement. As adrenal cortical adenomas have high lipid contents, the absolute and relative contrast washout can be calculated, yielding a very high sensitivity and specificity for the diagnosis of an adrenal cortical adenoma (1,5,6). Similarly, the lipid content in an adrenal cortical adenoma provides typical findings using MRI: adenomas are homogeneous, have a signal
intensity equal to or less than the liver, and they lose intensity on chemical shift imaging (1). Pheochromocytoma can also usually be reliably diagnosed on imaging with a hypervascular appearance on T2-weighted MRI (1). Nuclear medicine imaging is used in the workup of suspected adrenal metastases. Although the sensitivity and specificity of nuclear medicine imaging for the diagnosis of metastases are very high, biopsy confirmation may still be warranted (7). Regarding ultrasonography, this modality allows visualization of the adrenal gland and masses within, but poor ability to characterize the lesions that are seen (7,8). In addition to specific features noted via each imaging technique, size remains an important predictor of malignancy with incidental, nonfunctional nodules less than 4 cm unlikely to be malignant (9,10). The National Institute of Health Consensus Conference stated that adrenal incidentalomas less than 4 cm should be monitored, those greater than 6 cm should be resected, and masses between 4 and 6 cm can be watched or resected (11). However, considerable overlap is seen between size categories with large benign tumors and small malignancies observed (12). It should also be noted that autopsy findings document a mean of 2 cm for adrenal metastasis and therefore size alone is not a sufficient criteria to characterize adrenal lesions (13).
intensity equal to or less than the liver, and they lose intensity on chemical shift imaging (1). Pheochromocytoma can also usually be reliably diagnosed on imaging with a hypervascular appearance on T2-weighted MRI (1). Nuclear medicine imaging is used in the workup of suspected adrenal metastases. Although the sensitivity and specificity of nuclear medicine imaging for the diagnosis of metastases are very high, biopsy confirmation may still be warranted (7). Regarding ultrasonography, this modality allows visualization of the adrenal gland and masses within, but poor ability to characterize the lesions that are seen (7,8). In addition to specific features noted via each imaging technique, size remains an important predictor of malignancy with incidental, nonfunctional nodules less than 4 cm unlikely to be malignant (9,10). The National Institute of Health Consensus Conference stated that adrenal incidentalomas less than 4 cm should be monitored, those greater than 6 cm should be resected, and masses between 4 and 6 cm can be watched or resected (11). However, considerable overlap is seen between size categories with large benign tumors and small malignancies observed (12). It should also be noted that autopsy findings document a mean of 2 cm for adrenal metastasis and therefore size alone is not a sufficient criteria to characterize adrenal lesions (13).
TABLE 9.1 Indications to Perform an Adrenal Biopsy | |||
|---|---|---|---|
|
Prebiopsy blood work includes a complete blood count, comprehensive metabolic panel, and coagulation studies (1). Analysis of urine and serum catecholamines is performed in patients with suspected pheochromocytoma. Imaging and metabolic results are particularly important in patients with a pheochromocytoma because performing a biopsy can precipitate a hypertensive crisis due to excessive catecholamine secretion. Biopsy of a suspected pheochromocytoma is usually not performed, but if needed, should be done only with pharmacologic blockade.
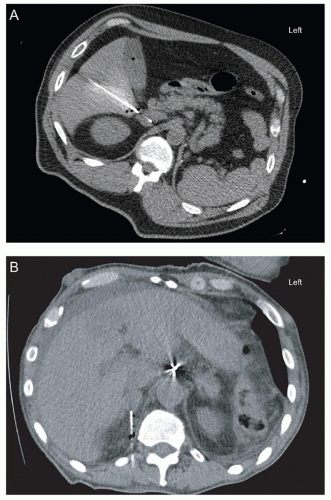
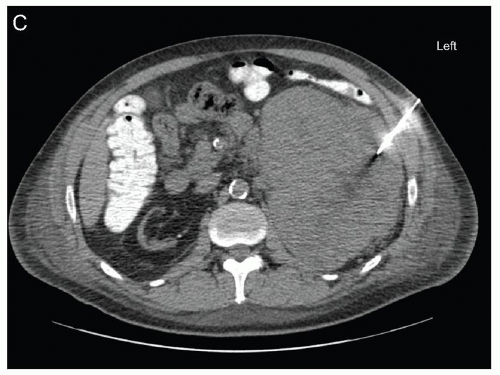
Most commonly, adrenal biopsies are obtained via a posterior, anterior, decubitus, or transhepatic percutaneous approach using CT guidance, ultrasound guidance, or a combination of the two modalities (Fig. 9.1, eFig. 9.2). Benefits of CT guidance include better visualization of internal structures and the possibility to use contrast, but is more costly, takes more time, uses radiation, and is not performed in real time (14). Ultrasound guidance is used in real time, does not use radiation, and is less costly, but provides poorer visualization (14). Adrenal biopsy
pathology specimens that may be collected include tissue cores, a fine needle aspiration, or both. A variety of needle types and sizes (18 to 23 gauge) may be used with larger needles reported to have better diagnostic yield (15,16).
pathology specimens that may be collected include tissue cores, a fine needle aspiration, or both. A variety of needle types and sizes (18 to 23 gauge) may be used with larger needles reported to have better diagnostic yield (15,16).
COMPLICATIONS
The complication rate of a percutaneous adrenal biopsy procedure is approximately 5% (15,17,18,19,20,21). The most common complications are self-limited pneumothorax and bleeding. Rare complications include pancreatitis, hypertensive crisis due to biopsying an unsuspected pheochromocytoma, and hemothorax. Needle tract seeding is exceedingly rare. The frequency of complications which require further medical management is less than 2% (15,19,20).
USAGE
Prior to dedicated adrenal imaging, the majority of adrenal biopsies were obtained for evaluation of adrenal masses that ultimately proved to be adrenal cortical adenomas (15,19,22). With improved imaging, the proportion of adrenal biopsies which detect adrenal cortical adenomas has decreased, with a higher percentage of biopsies containing metastatic carcinoma (15). The utility of biopsy is limited, as imaging has high sensitivity
and specificity; adrenal cortical adenoma cannot always be reliably histologically differentiated from adrenal cortical carcinoma and adrenal biopsy is an invasive technique with risk, cost, and discomfort to the patient, which requires a skilled operator in order to obtain sufficient representative lesional tissue. Therefore, in the last decade compared to prior years, the usage of adrenal biopsies may have decreased. However, adrenal biopsy is still described as a technique that is overutilized as many biopsies that are performed do not change patient management (10, 23). Our experience shows little change in usage in recent years (Fig. 9.2



and specificity; adrenal cortical adenoma cannot always be reliably histologically differentiated from adrenal cortical carcinoma and adrenal biopsy is an invasive technique with risk, cost, and discomfort to the patient, which requires a skilled operator in order to obtain sufficient representative lesional tissue. Therefore, in the last decade compared to prior years, the usage of adrenal biopsies may have decreased. However, adrenal biopsy is still described as a technique that is overutilized as many biopsies that are performed do not change patient management (10, 23). Our experience shows little change in usage in recent years (Fig. 9.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree