Type of incontinence
Never
Rarely
Sometimes
Usually
Always
Solid stools
0
1
2
3
4
Liquid stools
0
1
2
3
4
Gas
0
1
2
3
4
Wears pad
0
1
2
3
4
Altered lifestyle
0
1
2
3
4
Dr. Scaglia, who is well trained in the procedure, performed the acupuncture.
The sterile and disposable acupuncture needles were 40 mm long and 0.3 mm in diameter and had stainless wire at the tip and copper wire at the handle. After insertion in the acupoint, the needles were gently stimulated by rotation and then left in place for 20 min.
During the trial the selection and localization of these points were mainly based on traditional Chinese medicine (TCM), and the following points were used: RM 3 (Zhong ji) and RM 6 (Qi Hai), both located at the midline of the lower abdomen; DM 4 (Ming Men) and BL 23 (Shen Shu) in the lumbar region; BL 32 (Ci Liao) in the 2nd sacral foramen; LI 4 (He Gu) in the hand between the first and second metacarpal bones; ST 36 (Zu San Li) at outer side of the leg below the knee; and K (Tai Xi) at the inner side of the ankle.
The results were presented as a median and interquartile range. Data was analyzed with Student-Fisher t-test (p < 0.05).
The overall mean continence score of all patients changed from 10 (3–21) estimated before treatment to zero (0–7) (p < 0.05) at 10 weeks, reflecting a significant improvement in continence. The continence index available in 14 patients at 18 months from the start of the treatment was 1 (0–8) (p < 0.05) (Fig. 5.1).
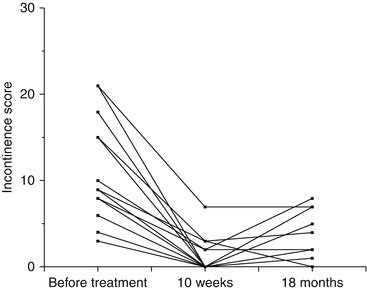
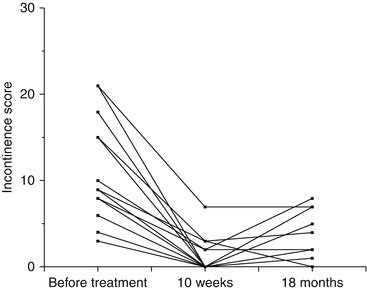
Fig. 5.1
Individual fecal incontinence score before and at intervals after acupuncture sessions
Before acupuncture fecal incontinence occurred in nine of the 15 patients, with a mean incontinence score of 17 (9–18). After 10 weeks of treatment, these showed a significant improvement, with a median score of 0 (0–3), and when assessed at a later stage (18 months), they still scored favorably, with a median score of 1 (0–6).
The six patients who did not have fecal incontinence before the treatment had less severe incontinence (flatus and/or soiling), with a mean score of 4 (3–5) before starting the sessions. At 10 weeks these improved considerably, as reflected in the mean score of 0 (0–0).
The improvement – observed after the third acupuncture treatment – remained persistent for a long time after cessation of treatment in some patients.
Sporadic episodes of soiling were observed, mainly associated with irregularity in bowel movements, in patients regularly checked for a 7-month period after the completion of acupuncture.
As shown in Fig. 5.2, the majority of patients that suffered irregularity in bowel habits when entering the study improved significantly at 10 weeks and quite a few experienced a prolonged favorable state even at longer follow-ups. At 18 months bowel habits still remained regular in eight out of 14 patients, and 12 had firm stools.
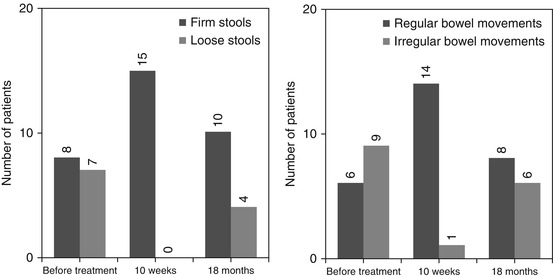
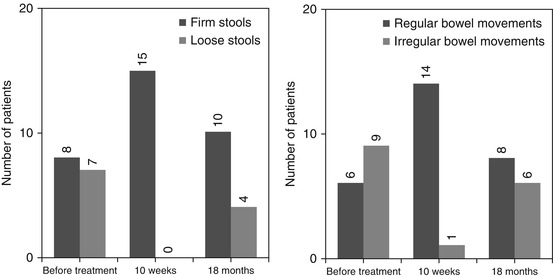
Fig. 5.2
Bowel habits (left panel) and stool consistency (right panel) before and after acupuncture
At 10 weeks after acupuncture, resting anal pressure had increased from 25 (17–35) mmHg to 36 (20–42) mmHg (p = 0.05). While maximal sphincter squeeze pressure remained uninfluenced, the ability to sustain the squeeze pressure increased from 41 (32–68) mmHg to 60 (40–100) mmHg (p < 0.05). Prior to the acupuncture sessions, the sensation of rectal filling was absent or blunt in six patients, and the defecation urge sensation was blunt or absent in two patients. These defects in rectal sensory function remained unchanged. The average rectal volume 348 (340–402) ml also remained unchanged (Table 5.2).
Table 5.2
Manometric results
Pre- | Post (10 weeks) | Post (18 weeks) | |
|---|---|---|---|
Anal pressures (mmHg) | |||
Resting press | 25 (17–35) | 36 (20–42) | 37 (18–48) |
Squeeze | 87 (58–117) | 87 (55–132) | 65 (54–118) |
Sustained squeeze (at 15 s) | 41 (32–68) | 60 (40–100) | 45 (30–59) |
Rectal sensibility (distension pressure cm H 2 O) | |||
Threshold | 15 (10–20) | 15 (11–20) | 10 (9–15) |
Urge | 20 (20–25) | 20 (20–25) | 20 (14–21) |
Rectal volume (ml) | |||
Rectal volume (40 cm H2O dist press) | 348 (340–402) | 334 (299–369) | 342 (311–358) |
At 18 months resting anal pressure was still well retained, whereas the ability to sustain the anal squeeze had returned to pretreatment levels. Rectal volume and the rectal sensory variables were unchanged.
An important concept in TCM is point specificity, which implies that stimulation of some acupoints is effective in treating certain clinical conditions, whereas other acupoints are less/not effective.
A systematic review designed to evaluate whether there are points specific to diseases concluded that approximately half of the trials produced evidence for point specificity and half did not [51].
This raises the interrogative: if point specificity does not exist, can appropriate controls on the inactive acupoints of certain conditions be developed for acupuncture? If rigorous studies that show clear point-specific responses were conducted, what was the underlying mechanism? In a study examining potential answers to these questions from a pelvic floor perspective, we collected data suggesting that point-specific responses to EA at different points exist. Stimulation of certain points (KI 3, 36 ST, DM 1, RM 1) results in a significant raise in anal pressure and in rectal contraction, while stimulating others (RM 3–6) causes more modest changes or no change at all (BL 32).
The stimulation of somatic nerves that project indirectly to regions of the brain concerned with regulation of sympathetic outflow underlies the capability of certain acupoint to raise the pelvic floor tonus effectively.
During a pilot study, we tried to investigate whether the electrical stimulation of sacral acupoints had any effect on the anorectal motility, recorded simultaneously to the treatment, since manual stimulation of BL 32 alone, located at the level of the second sacral foramen, was not producing any change.
Ten female patients, mean age 59, presenting various fecal continence defects were studied.
Eight acupuncture needles were placed bilaterally at the level of the sacral roots S1, S2, S3, and S4 and connected to an external neurostimulator delivering unipolar monophase rectangular impulses. Each couple of needles was consecutively electrostimulated with an increasing frequency and intensity up to the maximum amplitude the patient can tolerate. A anorectal mano-volumetry assessment was performed before and during the electrostimulation. The stimulation caused a significant rectal relaxation, ranging from 180 (137–231) ml before the experiment to 227 (188–254) ml (p < 0.05) during stimulation, corresponding to a 25 % increase of rectal volume. No effects were observed in anal resting pressure. When the second sacral root was stimulated, a rectal motility activation could be observed: in basal condition the maximum rectal volume displacement recorded was 5 (4–25) ml and during transcutaneous electrical stimulation at the second sacral foramen was 18 (13–38) ml (p 0.05).
The mechanism of action of electric acupuncture and its effects on the anorectal function remains unknown but could be similar to how sacral nerve stimulation achieves favorable results. The general rectal relaxation induced during the acute electrostimulation, for example, could be due to a parasympathetic effect.
Because the theory behind acupuncture as treatment of incontinence explains that it is intended to tackle the hypothetic subclinical adrenal dysfunction, we performed a pilot study on 12 patients to explore the effects of manual acupuncture on the endocrine function.
We are not the first to investigate this, as a recently published study on the beneficial effects of acupuncture in the irritable bowel syndrome (IBS) shows how the treatment is linked with a detectable change in salivary cortisol [5].
In our pilot study we utilized the same manual acupuncture schema and incontinence scoring system of the study on fecal incontinence previously described.
We observed an improvement in the incontinence mean score, with an initial value of 11.5 (sd 6.8) that significantly decreased to 5.8 (sd 4.9), and a significant reduction of salivary cortisol (h 8) changing from 8.6 (2.2) to 10.9 (5.9) μg/ml (Student t-test p < 0.05), after 10 sessions of acupuncture.
These results suggest that more than one mechanism might be involved in the beneficial influence of acupuncture.
An analysis of the urinary 8-isoprostanes was performed as well; these are specific products of lipid peroxidation, which is a consequence of oxidative stress and peroxynitrate formation, measurable by enzyme-linked immunosorbent assay (ELISA). Nitric oxide might influence the internal sphincter function, acting as a neurotransmitter. Although the antioxidant action of acupuncture was never reported in animal studies, this test aims to evaluate the possible anti-inflammatory effect of acupuncture in vivo and its relationship with cortisol levels.
Urinary isoprostane levels lowered from 1.8 (sd 0.6) to 1.5 (0.4); however, these changes were not statistically significant, supposedly due to an inverse relationship between isoprostane and cortisol levels.
Irritable bowel syndrome (IBS) comprises a group of functional bowel disorders in which abdominal discomfort or pain are associated with defecation or a change in bowel habit and with features of disordered defecation. A lowered sensory threshold to rectal distention is a hallmark of IBS patients. The effect of acupuncture on IBS is elusive. In an open-design pilot study, the 101 patients with IBS that received a 4-week course of acupuncture presented an improvement in overall well-being and in bloating but not in abdominal discomfort or defecation frequency. A double-blind trial in patients with IBS showed no significant difference in the improvement of IBS symptoms between acupuncture and sham acupuncture, although the improvement seemed more consistent with acupuncture.
Little effort was made to investigate the efficacy of acupuncture on constipation, and there is scarce information in the literature. One study of 17 children with chronic constipation demonstrated that acupuncture gradually increased the plasma opioid level as well as the frequency of bowel movement to a value similar the control during a 10-week treatment period [6]. However, his findings were not confirmed in adult patients with constipation [7].
An acupoint considered very important for the treatment of constipation is Tianshu (ST25) [52]; the effects of manual stimulation were significantly superior to those obtained with medication, increasing the number of patients whose defecation was up to four times per week together with the rise in constipation score and patients’ satisfaction. In another study on 100 patients with chronic functional constipation, the total positive results with moxibustion and acupuncture were 74 and 52 %, respectively [53].
The effect of electric acupuncture at “Tianshu” (ST 25) on colonic smooth muscle structure and interstitial nerve plexus was studied in rats with slow transit constipation [54]: the results showed that electrical stimulation of ST 25 improved the slow transit colon inducing structural changes too.
The efficacy of auricular therapy as treatment of constipation [55] was also reviewed, and 29 relevant studies, from 1994 to 2008, were considered. All articles reported positive results, but their findings cannot be generalized because of two significant methodological flaws: the uncertainty in acupoint identification and inconsistent protocols.
Our experience in this regard is summarized in a pilot study on ten patients with multiple sclerosis and bowel dysfunctions with prevalent constipation and, as a control group, ten patients with functional constipation. We investigated functional scores, quality of life, anorectal manometry scores, and bowel transit time after 2–4 weeks of acupuncture performed twice a week. The results were recapitulated as percentages of patients with up to four defecations per week after acupuncture: 70 % of severe functional constipation and 50 % of multiple sclerosis patients had normal bowel habits at the end of treatment; these results decreased respectively to 40 and 30 % at the 3-month follow-up, suggesting that a maintenance protocol of regular acupuncture session was needed.
5.3 Acupuncture for Urinary Tract Diseases
The use of acupuncture and electric acupuncture in the context of diseases of the urinary system has been and still is the subject of numerous experimental and clinical studies.
The efficacy of traditional Chinese acupuncture for nocturnal enuresis (NE) was reported to range from 76 to 98 %. Asian researchers identified the presence of nocturnal detrusor instability in up to one third of all “enuretic” children [56, 57], and NE failed to respond to standard treatment in 44 % of patients [58, 59] (the standard treatments include the bed-wetting alarm, used to facilitate waking up children with monosymptomatic enuresis, and the synthetic antidiuretic hormone that aims to reduce the volume of overnight urine or the antimuscarinic medication and urotherapy). Acupuncture therapy was reported to suppress uninhibited bladder contractions and to significantly improve wetting where there is urodynamic evidence of detrusor over activity.
The acupuncture points used to treat bladder dysfunction were located in areas innervated by spinal sacral segments S2 through S4 and were stated in the treatment protocols. The points BL 23, BL 28, BL 32, RN 3, RN 4, RN 6, and RN 12 were shown to influence the spinal micturition centers and parasympathetic innervation of the urinary tract [60], while the stimulation of scalp acupoints DU 20 and DU 14 modulated brain function via the inner temporal, thalamencephalon and prefrontal cortical systems [61]. The stimulation of the acupoints UB 20, UB 13, SP 6, ST 36, KI 3, and LU 9 was considered to invigorate the spleen, vital energy, and blood, thereby facilitating the normalization of the bladder function. The high concentration of neuroendocrine transmitters and hormones at acupuncture points was released and spread after needling and other stimulation [62, 63]. Functional magnetic resonance imaging (fMRI) and PET scan performed during natural or conventional bladder filling in healthy subjects showed activation of specific brain regions: the pons, midbrain periaqueductal gray, thalamus, hypothalamus, and frontal cortex [64]. During acupuncture at ST 36, fMRI indicated the activation of the hypothalamus and of the bilateral prefrontal cortex [65], suggesting that acupuncture utilized the neural brainstem–thalamus–cortex reticular system. The sustained activation of the hypothalamus was observed, as well as the increase in concentration of some neurotransmitters, such as 5-HT [65, 66].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






