CHAPTER 67 Acalculous Biliary Pain, Acalculous Cholecystitis, Cholesterolosis, Adenomyomatosis, and Polyps of the Gallbladder
This chapter is dedicated to the memory of Lyman E. Bilhartz, MD.
Although gallstones and their complications account for most cholecystectomies,1 a consistent 15% of these operations are performed in patients without gallstones.2 In these patients, the majority of cholecystectomies are performed as treatment for one of two distinct clinical syndromes: acalculous biliary pain and acalculous cholecystitis. As shown in Table 67-1, acalculous biliary pain is generally a disorder of young, predominantly female, ambulatory patients and mimics calculous biliary pain. Acute acalculous cholecystitis is typically a disease of immobilized and critically ill older men with coexisting vascular disease. Because the clinical features and prognosis of these two entities are quite different, they are considered separately in this chapter. Three typically asymptomatic conditions of the gallbladder—cholesterolosis, adenomyomatosis, and gallbladder polyps—are also reviewed.
Table 67-1 Comparison of Acalculous Biliary Pain and Acute Acalculous Cholecystitis
| ACALCULOUS BILIARY PAIN | ACUTE ACALCULOUS CHOLECYSTITIS | |
|---|---|---|
| Epidemiology | Female preponderance (80%) | Male preponderance (80%) |
| Young to middle-aged ambulatory patient | Critically ill elderly patient in intensive care unit | |
| Risk factors are similar to those for cholelithiasis (i.e., obesity and multiparity) | Risk factors are preexisting atherosclerosis, recent surgery, and hemodynamic instability | |
| Clinical features | Episodic right upper quadrant or epigastric pain identical to calculous biliary pain | Unexplained sepsis with few localizing signs; rapid progression to gangrene and perforation |
| Physical findings are usually normal | Physical examination may show fever; right upper quadrant tenderness is present in only 25% | |
| Laboratory findings are usually normal | ||
| Leukocytosis and hyperamylasemia may be present | ||
| Diagnostic tests | Ultrasonography shows no stones and usually a normal gallbladder | See Table 67-2 |
| Biliary drainage (Meltzer-Lyon test) typically demonstrates cholesterol crystals | ||
| Stimulated cholescintigraphy using cholecystokinin to measure the gallbladder ejection fraction may identify patients who are likely to improve after cholecystectomy | ||
| Treatment | Elective cholecystectomy for patients with classic biliary pain and either biliary cholesterol crystals or a gallbladder ejection fraction <35% | Urgent cholecystostomy or emergency cholecystectomy for gangrene or perforation |
| Prognosis | Good; attacks continue unless cholecystectomy is performed | Poor, with a mortality rate of 10%-50% |
ACALCULOUS BILIARY PAIN
DEFINITION AND CLINICAL FEATURES
Intense epigastric or right upper quadrant pain that starts suddenly, rises in intensity over a 15-minute period, and continues at a steady plateau for 30 minutes or more before slowly subsiding is characteristic of biliary pain. The localization of pain to the right hypochondrium or radiation to the right shoulder is the most specific finding for a biliary tract origin.3 The attacks of pain are frequently precipitated by ingestion of a meal and may be accompanied by restlessness, nausea, or vomiting. Between attacks, the physical findings are usually normal, with the possible exception of residual upper abdominal tenderness.
When a patient presents with such a history and ultrasonography confirms the presence of gallstones, the management is straightforward—namely, elective cholecystectomy (or perhaps an attempt at medical dissolution of the stones) (see Chapters 65 and 66). In comparison, the management of acalculous biliary pain represents a significant challenge. Patients with acalculous biliary pain have clinical features and biliary-type pain similar to those of patients with cholelithiasis, but a normal gallbladder on ultrasonography and normal serum levels of liver and pancreatic enzymes.4,5 Acalculous biliary pain may stem from a spectrum of overlapping disorders, including chronic acalculous cholecystitis, acalculous biliary disease, gallbladder dysmotility, and biliary dyskinesia, which share symptomatology but differ in the pathologic findings of the resected gallbladder. In patients with acalculous biliary pain, symptomatic improvement following cholecystectomy is more variable.
EPIDEMIOLOGY AND PATHOPHYSIOLOGY
Ultrasound-negative biliary pain is common in population studies, with reported prevalences of approximately 7% in men and 20% among women.6 Acalculous biliary pain is predominantly a disorder of young women. In one series of more than 100 patients, 83% were female, and the mean age was approximately 30 years.5
The cause of the acalculous biliary pain syndrome is not known, but indirect evidence suggests that several different etiologies may culminate in the same clinical presentation. Stimulated duodenal bile from patients with acalculous biliary pain is more dilute with respect to both bile acids and phospholipids than bile from patients with gallstones or from control women without biliary symptoms.7 The low bile acid concentration may be related to the sluggish or incomplete gallbladder contraction that has been observed in patients with acalculous biliary pain. The lower molar percentage of phospholipids is consistent with the hypothesis that biliary phospholipids are hydrolyzed to free fatty acids, which incite inflammation.
The striking preponderance of young, fertile women among patients with acalculous biliary pain closely parallels the epidemiology of cholelithiasis, suggesting that the two conditions have similar risk factors. Some studies have shown that up to half of patients with acalculous biliary pain actually have microscopic cholelithiasis in resected gallbladder specimens,8 indicating that the original ultrasonogram was falsely negative. Examination of a bile specimen for microlithiasis (Meltzer-Lyon test, discussed later) can be helpful in identifying these patients.
Several studies have shown that a subset of patients with acalculous biliary pain have histologic evidence of cholesterolosis in their resected gallbladders (see later).9–11 Although usually an incidental pathologic finding, cholesterolosis of the gallbladder may, in some patients, disrupt normal gallbladder contraction and result in biliary pain. In other patients, the resected gallbladder demonstrates significant inflammation, characteristic of chronic acalculous cholecystitis.12
Finally, acalculous biliary pain is listed as a functional gastrointestinal disorder by a multinational working committee of gastrointestinal investigators (Rome III classification [see Chapter 118]), with the implication that a pathologic lesion is not required for the diagnosis.4 In patients with a histologically normal gallbladder, a lack of coordination between gallbladder contraction and sphincter of Oddi relaxation, or gallbladder dyskinesia, may cause biliary pain (see Chapter 63). Alternatively, the strong link between acalculous biliary pain and other functional bowel disorders suggests that visceral hypersensitivity may also contribute to biliary pain in patients with a normal gallbladder.6
DIAGNOSIS AND TREATMENT
As described earlier, the symptoms of acalculous biliary pain may be indistinguishable from those of cholelithiasis. A careful review of the patient’s complaints should confirm that the symptoms are genuinely suggestive of biliary pain rather than dyspepsia, heartburn, cramping abdominal pain, or flatulence.3 If the symptoms are consistent with biliary pain, a detailed review of the ultrasonogram with a radiologist is warranted. Although gallstones larger than 2 mm are unlikely to be missed (the sensitivity of ultrasound for detecting stones exceeds 95%), other ultrasonographic evidence of gallbladder disease may be overlooked if the primary focus is to exclude stones. Patients with adenomyomatosis of the gallbladder or small cholesterol polyps may have biliary pain that is relieved by cholecystectomy (see later). Determining in whom and when to pursue cholecystectomy for patients with biliary pain and a normal ultrasound result presents a challenge.
Examination of the Bile for Cholesterol Crystals (Meltzer-Lyon Test)
If the ultrasonogram is normal, the bile may be examined for evidence of cholesterol crystals. Long before the advent of ultrasonography, biliary drainage was used to identify patients who were likely to have gallstones. The test has been modified so that the bile is now aspirated during an upper endoscopy after stimulation of gallbladder contraction with intravenous cholecystokinin (CCK).13 The bile should be kept at room temperature and examined immediately (after completion of the endoscopy) under a microscope for the presence of characteristic birefringent, notched rhomboid cholesterol crystals or calcium bilirubinate granules.
Limited clinical studies in patients with acalculous biliary pain have shown that approximately one third have crystals in their bile.9,10 At the time of surgery, most of these patients have documented microlithiasis and pathologically confirmed cholecystitis, and their symptoms resolve following cholecystectomy. The remaining two thirds of patients who do not have crystals in their bile generally have a benign course and rarely return with evidence of significant biliary tract disease.
Stimulated Cholescintigraphy
A second approach to determining which patients with acalculous biliary pain are likely to benefit from cholecystectomy involves calculation of a gallbladder ejection fraction (GBEF) using cholescintigraphy (see Chapter 63). An intravenously administered radiolabeled hepatobiliary agent (e.g., 99mTc-diisopropyl iminodiacetic acid) is concentrated in the gallbladder, and a computer-assisted gamma camera measures activity before and after stimulation of gallbladder contraction with a slow intravenous infusion of CCK over 30 minutes. The GBEF is defined as the change in activity divided by the baseline activity. Studies in healthy volunteers have shown that normal GBEF averages 75% and virtually always exceeds 35%.5 Fatty meal cholescintigraphy is a less costly alternative to the CCK-stimulated test and uses oral fat intake (typically half-and-half milk) to stimulate gallbladder contraction physiologically; normal values for GBEF tend to be lower than those for CCK-stimulated cholescintigraphy.14
Ironically, as stimulated cholescintigraphy gains clinical acceptance, its positive predictive value is expected to fall. When the test was first developed, most patients referred for testing had been experiencing biliary pain for years, thereby allowing ample time for other causes of pain to become evident; therefore, the pretest probability of having a primary gallbladder motility derangement was high, and the specificity of the test was excellent. Now, the test is employed earlier in the evaluation of patients with biliary pain (sometimes immediately after ultrasonography fails to demonstrate gallstones), and patients with nonbiliary or self-limiting diseases have not been weeded out. The earlier that cholescintigraphy is employed, the lower the pretest probability of acalculous biliary pain and, unfortunately, the lower the predictive value of a positive result.15
Fewer than half of patients with acalculous biliary pain have a depressed GBEF, but most of those who do have a depressed GBEF continue to have symptoms when followed for as long as 3 years. If cholecystectomy is performed in these patients, histologic evidence of chronic cholecystitis is found in approximately 90%, cystic duct narrowing in 80%, and cholesterolosis in 30%.11 Long-term symptom relief following cholecystectomy typically occurs in 65% to 80% of patients with an abnormal GBEF5,16,17; however, up to 50% of patients managed without surgery also experience symptom relief.18
ACUTE ACALCULOUS CHOLECYSTITIS
DEFINITION
Acute acalculous cholecystitis is acute inflammation of the gallbladder in the absence of stones. Acute cholecystitis resulting from calculi is discussed in Chapter 65. The designation acalculous cholecystitis has been questioned as incorrectly suggesting that the disease is simply cholecystitis without stones. Instead, the term necrotizing cholecystitis has been proposed to reflect the distinct etiology, pathology, and prognosis of the disease.19
EPIDEMIOLOGY
Acute acalculous cholecystitis accounts for 5% to 10% of cholecystectomies performed in the United States. In fact, of the cholecystectomies performed in postoperative or hospitalized patients recovering from trauma or burns, more than half are for acalculous disease.20
Less commonly, acute acalculous cholecystitis may occur in the absence of antecedent trauma or stress, especially in children,21 elderly patients with coexisting vascular disease,22 bone marrow transplant recipients, patients who receive cytotoxic drugs via the hepatic artery,23 and patients with the acquired immunodeficiency syndrome.24 In some cases, specific infectious causes can be identified, such as Salmonella,25 Staphylococcus aureus,26 cytomegalovirus in immunocompromised patients,27 and Epstein-Barr virus in children.21 Systemic vasculitides such as polyarteritis nodosa and systemic lupus erythematosus may manifest as acute acalculous cholecystitis caused by ischemic injury to the gallbladder.28 Finally, acute acalculous cholecystitis is being recognized increasingly in otherwise healthy people without any risk factors.29,30 As a group, patients with acute acalculous cholecystitis are more likely to be men and old than are patients with cholecystitis caused by calculi, cases of which cluster in younger women.31
PATHOGENESIS
Most cases of acute acalculous cholecystitis occur in the setting of prolonged fasting, immobility, and hemodynamic instability. The gallbladder epithelium, although normally a robust tissue, is exposed continuously to one of the most noxious agents in the body: a concentrated solution of bile acid detergents. In the course of a normal day, the gallbladder empties the concentrated bile several times and is replenished with dilute (and presumably less noxious) hepatic bile. With prolonged fasting, the gallbladder is not stimulated by CCK to empty, and concentrated bile stagnates in the gallbladder lumen.32 In addition, the gallbladder epithelium has relatively high metabolic energy requirements in order to absorb electrolytes and water from the bile. Therefore, in an immobile, fasting patient with splanchnic vasoconstriction (often resulting from septic shock in a patient in the intensive care unit), ischemic and chemical injury to the gallbladder epithelium may occur.33 A study that compared the microcirculation of gallbladders removed for gallstone disease or acute acalculous cholecystitis showed that the capillaries barely filled in acalculous cholecystitis, indicating that disturbed microcirculation may play an important role in its pathogenesis.34
Inappropriate activation of factor XII (demonstrated to initiate gallbladder inflammation in animals)35 and local release of prostaglandins in the gallbladder wall36,37 have also been implicated in the tissue injury associated with acalculous cholecystitis. In animal models, tissue destruction can be attenuated by inhibiting prostaglandin synthesis with indomethacin. Expression of tight junction proteins in the gallbladder epithelium of patients with acute acalculous cholecystitis differs from calculous cholecystitis, perhaps reflecting the role of increased gallbladder wall permeability in the systemic inflammatory response.38 Infection of the gallbladder mucosa with bacteria, usually gram-negative enteric organisms and anaerobes,39 is thought to be a secondary event in acute acalculous cholecystitis, following rather than causing the initial injury.
One postulated explanation for the rising incidence of acute acalculous cholecystitis, particularly in younger patients, is obesity and the accompanying increase in gallbladder wall fat, which has been demonstrated to interfere with gallbladder emptying in animal models. In one study, sixteen patients with acute acalculous cholecystitis had significantly more gallbladder wall fat than normal subjects without cholecystitis.40
CLINICAL FEATURES
The clinical features of acute acalculous cholecystitis often differ from those of acute cholecystitis caused by stone disease. Although right upper quadrant pain, fever, localized tenderness overlying the gallbladder, and leukocytosis may be evident in classic presentations, such as those of younger outpatients, some or all of these features are commonly lacking in elderly postoperative patients.41 Symptoms or signs referable to the right upper quadrant are initially absent in 75% of cases. Unexplained fever or hyperamylasemia may be the only clues that something is amiss.
Compared with the clinical course of typical calculous cholecystitis, that of acute acalculous cholecystitis is more fulminant. By the time the diagnosis has been made, at least half of the patients have experienced a complication of cholecystitis, such as gangrene or a confined perforation of the gallbladder.42 Empyema of the gallbladder and ascending cholangitis may further complicate cases in which bacterial superinfection of the gallbladder has occurred. Because the disease often occurs in debilitated patients and complications occur rapidly, the mortality rate of acute acalculous cholecystitis is high, ranging from 10% to 50%, as compared with a 1% mortality rate in patients with calculous cholecystitis. Such high mortality rates have led some investigators to propose that empirical cholecystostomy be considered in gravely ill patients in the intensive care unit in whom no source of sepsis can be found.43
DIAGNOSIS
The rapid development of complications in acute acalculous cholecystitis makes early diagnosis critical for avoiding excessive mortality. Unfortunately, the lack of specific clinical findings pointing to the gallbladder, combined with a confusing clinical picture related to antecedent surgery or trauma, makes early diagnosis difficult. For elderly patients at risk, a high index of suspicion for biliary tract sepsis is the best hope for early recognition and treatment. Table 67-2 delineates several diagnostic criteria for acute acalculous cholecystitis.
Table 67-2 Diagnostic Criteria for Acute Acalculous Cholecystitis
| TECHNIQUE | FINDINGS |
|---|---|
| Clinical examination | Right upper quadrant tenderness is helpful, if present, but is lacking in three quarters of cases |
| Unexplained fever, leukocytosis, or hyperamylasemia is frequently the only finding | |
| Ultrasonography | Thickened gallbladder wall (defined as >4 mm) in the absence of ascites and hypoalbuminemia (defined as serum albumin <3.2 g/dL) |
| Presence of sonographic Murphy’s sign (maximum tenderness over the ultrasonographically localized gallbladder) | |
| Pericholecystic fluid collection | |
| Bedside availability is a major advantage | |
| Computed tomography | Thickened gallbladder wall (defined as >4 mm) in the absence of ascites and hypoalbuminemia |
| Pericholecystic fluid, subserosal edema (in the absence of ascites), intramural gas, or sloughed mucosa | |
| Best test for excluding other intra-abdominal diseases but requires moving the patient to a scanner | |
| Hepatobiliary scintigraphy | Nonvisualization of the gallbladder with normal excretion of radionuclide into the bile duct and duodenum indicates a positive result for acute cholecystitis |
| Results in critically ill, immobilized patients may be falsely positive because of viscous bile | |
| Morphine augmentation may reduce the number of false-positive results (see text) | |
| Better at excluding than confirming acute cholecystitis |
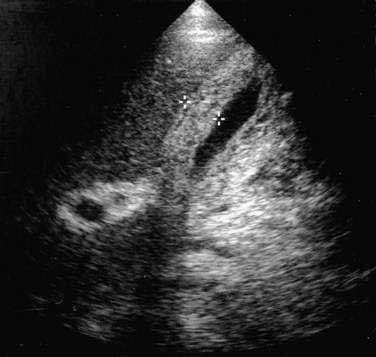
Ultrasonography
In the evaluation of patients with suspected acute acalculous cholecystitis, ultrasonography offers the distinct advantages of being widely available and easily transportable to the bedside.44 Three ultrasonographic findings indicative of gallbladder disease are a (1) thickened gallbladder wall (defined as >4 mm) in the absence of ascites or hypoalbuminemia, (2) sonographic Murphy’s sign (defined as maximum tenderness over the ultrasonographically localized gallbladder), and (3) pericholecystic fluid collection. A thickened gallbladder wall (Fig. 67-1) is not specific for cholecystitis but in the proper clinical setting is suggestive of gallbladder involvement and should prompt further evaluation. A sonographic Murphy’s sign is operator dependent and requires a cooperative patient but, when present, is a reliable indicator of gallbladder inflammation.45 A pericholecystic fluid collection indicates advanced disease. Sensitivity rates of ultrasonography for detecting acute acalculous cholecystitis have been reported to range from 67% to 92%, with specificity rates of more than 90%.44 Investigators have proposed an ultrasonographic scoring system to improve the diagnostic accuracy of ultrasonography in critically ill patients.46 Two points are given for distention of the gallbladder or thickening of the gallbladder wall, and 1 point each is given for “striated” thickening (alternating hypoechoic and hyperechoic layers) of the gallbladder wall, sludge, or pericholecystic fluid. Scores of 6 or higher accurately predict acalculous cholecystitis.
Computed Tomography
Computed tomography (CT) findings suggestive of cholecystitis include gallbladder wall thickening (>4 mm), pericholecystic fluid, subserosal edema (in the absence of ascites), intramural gas, and sloughed gallbladder mucosa. Sensitivity and specificity rates of these findings for predicting acute acalculous cholecystitis at surgery have been reported to exceed 95%. CT is also superior to ultrasonography in detecting disease elsewhere in the abdomen that could be the cause of a patient’s fever or abdominal pain.47 An obvious disadvantage of CT is that it cannot be performed at the bedside, which is necessary in many critically ill patients. Several investigators have emphasized that CT is complementary to ultrasonography and often detects gallbladder disease in high-risk patients with normal ultrasonographic findings.
Hepatobiliary Scintigraphy
Hepatobiliary scintigraphy may be useful for excluding cystic duct obstruction in patients with clinical features suggestive of acute cholecystitis. Under normal conditions, intravenously administered radionuclide is taken up by the liver, secreted into bile, concentrated in the gallbladder (where it produces a “hot spot” on a scan), and emptied into the duodenum. A positive scan result for cystic duct obstruction is defined as failure of filling of the gallbladder despite the normal passage of radionuclide into the duodenum. In suspected calculous cholecystitis, the pathogenesis of which involves obstruction of the cystic duct by a stone, filling of the gallbladder on scintigraphy virtually excludes cholecystitis as the cause of the patient’s symptoms.48
Hepatobiliary scintigraphy is less precise in acute acalculous cholecystitis. Gallbladder and cystic wall edema can cause an obstructive picture similar to calculous cholecystitis on scintigraphy. Patients with acute acalculous cholecystitis have often fasted for prolonged periods, a state that can result in concentrated, viscous bile that flows poorly through the cystic duct and causes a false-positive hepatobiliary scan result. Most patients with acute acalculous cholecystitis (in contrast to those with calculi) do not have an obstructed cystic duct; hence, hepatobiliary scans can be falsely negative as well.49 The sensitivity of the test may exceed 90%, but the lack of specificity in fasted, critically ill patients limits the usefulness of the test primarily to excluding acute acalculous cholecystitis rather than confirming the diagnosis. A study in which ultrasonography and cholescintigraphy were performed in critically ill patients found cholescintigraphy to be useful for the early diagnosis of acute acalculous cholecystitis, whereas ultrasonography alone did not permit an early decision regarding the need for surgery.50
In an effort to improve the accuracy of biliary scintigraphy, investigators have proposed the use of morphine-augmented cholescintigraphy, in which morphine sulfate is administered intravenously (0.05 to 0.1 mg/kg) to patients in whom the gallbladder has not been visualized on standard cholescintigraphy.51 The rationale for this procedure is that morphine increases resistance to the flow of bile through the sphincter of Oddi and thus forces filling of the gallbladder if the cystic duct is patent, thereby reducing the likelihood of a false-positive result. In approximately 60% of critically ill patients with possible biliary tract sepsis and a nonvisualized gallbladder on standard cholescintigraphy, the gallbladder is visualized after morphine augmentation, and, therefore, acute cholecystitis can be excluded as the source of sepsis.