Abdominal masses
Juan A. Tovar MD, PhD
Masses of gastrointestinal origin
Tumours and cysts of the liver
The liver is accessible to palpation when enlarged and therefore masses in the liver are easily detected.
Hydatic cysts
These are the result of accidental ingestion of scolices of Echinoccocus granulosus, a worm that parasitizes the intestine of the dog. When the scolices are ingested by lambs or humans, they pass the intestinal barrier and are transported by the blood stream to the first or second tissular filters, respectively the liver and the lung, where a form of resistance develops forming a cyst that grows slowly. The inside of the cyst contains a white gelatinous membrane lined by a fertile proligerous layer that frees live scolices into the clear hydatic fluid. The surrounding liver parenchyma undergoes an inflammatory and fibrotic reaction (pericystic layer). Hydatic cysts are often scarcely symptomatic in children, except when they fissure causing anaphylactic reactions. They are detected by abdominal palpation and the diagnosis is confirmed by ultrasound or computed tomography (CT) scan. Specific antigenic and blood tests help to confirm the diagnosis.
Treatment consists of albendazol and surgical emptying, sterilization and removal of the membrane of the cyst/s, accompanied by partial resection of the pericystic layer. Surgical removal may be performed laparoscopically.
Choledocal cysts
These usually originate in a defective bilio-pancreatic junction in which both ducts are confluent within the pancreas, allowing the bile and the pancreatic juice to mix and subsequently damage the choledocal wall. There are several anatomical varieties of choledocal cysts, but the most common is fusiform, in which the entire extrahepatic-biliary tract is enlarged (8.1). If not detected prenatally, this condition may become symptomatic later on as a painful mass occasionally accompanied by jaundice. CT scan and bilio-pancreatic magnetic resonance imaging (MRI) allow preoperative depiction of the anatomy of the cyst. Treatment is surgical and consists of the excision of the choledocal duct together with the gallbladder, the cystic and common hepatic duct, and of the replacement of the biliary tract by a Roux-en-Y hepaticjejunostomy performed in an open or laparoscopic operation1.
Vascular tumours of the liver (haemangioma)
These are the most frequent benign liver tumours in the newborn. They may be focal, multifocal, or diffuse and each one has a different pathologic pattern2. The focal variety is
a rapidly involuting congenital haemangioma and, as well as multifocal, often creates cardiovascular compromise due to large intratumoural arteriovenous shunts. Platelet trapping and consequently coagulation disorders may occur. In contrast, the most clinically relevant feature of diffuse tumours is their large volume that creates a compartment syndrome and eventually liver failure.
a rapidly involuting congenital haemangioma and, as well as multifocal, often creates cardiovascular compromise due to large intratumoural arteriovenous shunts. Platelet trapping and consequently coagulation disorders may occur. In contrast, the most clinically relevant feature of diffuse tumours is their large volume that creates a compartment syndrome and eventually liver failure.
Ultrasonography and MRI help to delimitate the extent. Biopsy is sometimes necessary particularly in cases with unusual features. Treatment is based on the awareness of the potential regression and of their responsiveness to corticosteroids and interferon (8.2). Most of these patients, except those in whom heart failure cannot be managed, improve over a few months and have their tumours reduced to residual, partially calcified masses. Surgical removal is seldom indicated and in some rare instances of diffuse tumours, liver transplantation is unavoidable.
Mesenchymal hamartomas of the liver
These are usually multicystic with solid mesenchymal components and may locate anywhere in the organ. They are asymptomatic except when they enlarge and are detected as liver masses. Modern imaging allows accurate preoperative assessment that is helped by the near-normal levels of tumoural markers. Treatment is always surgical (8.3). When removal is complete, there is no risk of recurrence3.
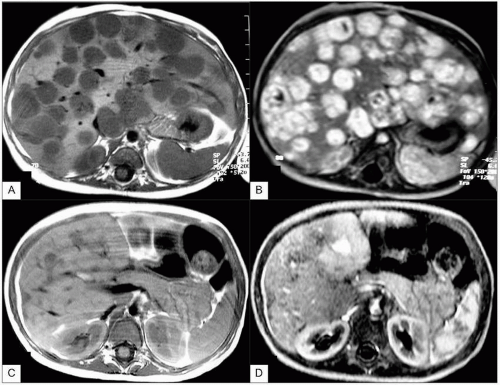 8.2 Multifocal liver haemangioma in a baby with hyperdynamic heart failure. MRI without (A) and with (B) gadolinium contrast depicts the huge vascular spaces in both lobes. He was treated with corticosteroids and interferon. Two years later (C, D), only residual vascular areas are visible and the child is healthy. |
Hepatoblastoma
Although it is the more frequent malignant liver tumour in children, hepatoblastoma remains rare. It grows rapidly and is occasionally multicentric. It can invade the vessels and also metastasize in the regional lymph nodes or, through the liver outflow, to the lungs and elsewhere. Most cases manifest as abdominal masses detected upon palpation. Alpha-fetoprotein (AFP) is a useful marker for diagnosis and follow-up.
CT scan and MRI are the cornerstones of pretreatment staging that allows selection of management protocols. We adhere to the staging of the Societé Internationale d’Oncologie Pédiatrique (SIOP). The liver is divided into two lobes by the falciform ligament and both lobes are subdivided in turn into two, to yield four segments. When
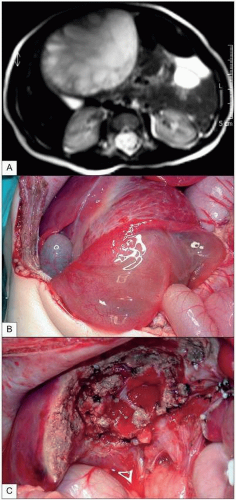
the tumour involves one (Stage 1) or two (Stage 2) of these segments (8.4), segmentectomy or lobectomy are usually required. When three segments are involved (Stage 3), more extensive operations are necessary (8.5) and when the four segments are affected (Stage 4), liver transplantation may be the only treatment option (8.6). Complete surgical removal is always necessary for cure and preoperative chemotherapy with platinum derivatives and doxorubicin greatly helps to reduce the original extent of the tumour. More than 80% of these children are cured, including Stage 4 cases4, 5.
the tumour involves one (Stage 1) or two (Stage 2) of these segments (8.4), segmentectomy or lobectomy are usually required. When three segments are involved (Stage 3), more extensive operations are necessary (8.5) and when the four segments are affected (Stage 4), liver transplantation may be the only treatment option (8.6). Complete surgical removal is always necessary for cure and preoperative chemotherapy with platinum derivatives and doxorubicin greatly helps to reduce the original extent of the tumour. More than 80% of these children are cured, including Stage 4 cases4, 5.
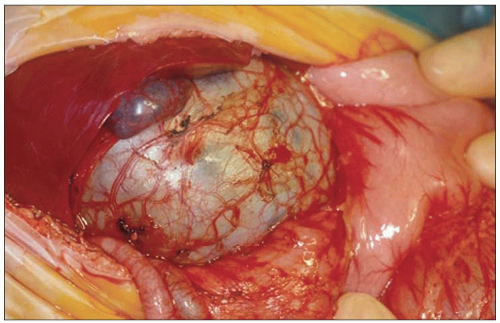
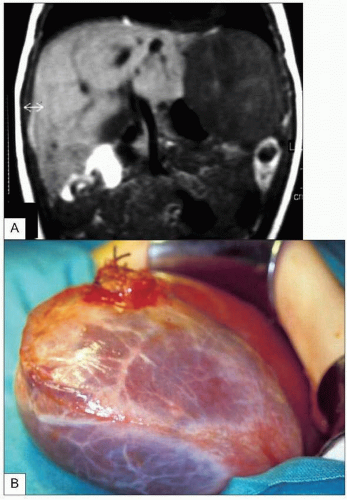
 8.3 A 1-year-old female with a palpable mass in the right hypochondrium and normal liver function and AFP. MRI showed a fluid-filled mass originating between the gallbladder and the falciform ligament (A). Surgical removal could be performed removing the gallbladder and a rim of liver tissue, but respecting the main vascular and biliary conduits (B, C). |
Hepatocarcinoma
This is very rare in children. They are generally seen either in children with metabolic cirrhosis or sporadically in older
children and adolescents. The tumour is often multicentric and secretes AFP. It metastasizes early, often to the lungs, and responds poorly to chemotherapy. This tumour has limited surgical possibilities and the prognosis is therefore poor except in patients with metabolic cirrhosis, in whom liver transplantation for the original disease allows total removal before metastases develop6.
children and adolescents. The tumour is often multicentric and secretes AFP. It metastasizes early, often to the lungs, and responds poorly to chemotherapy. This tumour has limited surgical possibilities and the prognosis is therefore poor except in patients with metabolic cirrhosis, in whom liver transplantation for the original disease allows total removal before metastases develop6.
Gastric tumours and masses
Bezoars
This condition always involves a psychopathological background. These children swallow either indigestible material (seeds, vegetal fibres that produce phytobezoar) or hair (trichobezoar). The entire gastric lumen and sometimes proximal small bowel are filled with this material, interfering with normal feeds. The bezoar is palpable as an epigastric mass. Diagnosis is confirmed by ultrasonography and sometimes by other imaging procedures.
The bezoar has to be surgically removed and the patient should be provided with adequate psychological support.
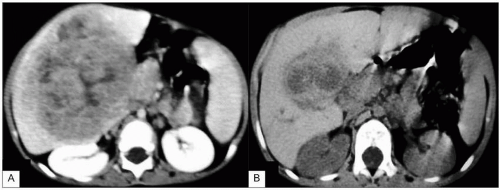 8.5 Stage 3 HB before (A) and after (B) 4 cycles of platinum and doxorubicin chemotherapy. At that time right trisegmentectomy could be successfully performed. |
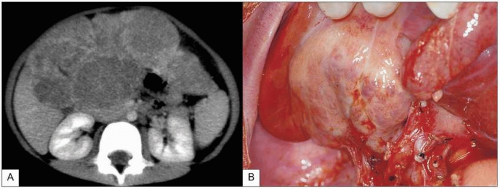 8.6 Stage 4 HB with several nodules on both lobes (A). During liver removal for transplantation, the bilateral, inextirpable nature of the tumour could be verified (B). After transplantation, the patient is doing well. |
Gastric tumours and cysts
Duplications of this part of the gastrointestinal tract may produce palpable epigastric masses. Leiomyosarcomas, rhabdomyosarcomas, teratomas, or gastrointestinal stromal tumours (GIST) formed by C-Kit-positive cells (interstitial Cajal cells) may be occasionally observed at this level where they cause ulceration and haemorrhage7.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree