10. THE COLON
After studying this chapter you should be able to:
1. Understand the functioning of the large intestine.
2. Understand the consequences of disease of the large intestine.
Introduction
The colon is the last 150cm or so of the gastrointestinal tract. It is a tube of approximately 6cm in diameter that extends from the ileum to the anus. Its main function is to store faecal material, and regulate its release into the external environment. It also absorbs water and electrolytes from the chyme, with the result that the faecal material becomes more solid as it passes through the colon. In addition it produces a thick mucinous secretion, which lubricates the passage of the faecal material through it. It also provides an environment for bacteria, some of which synthesize an important part of the vitamin requirement of the body.
Disease of the colon can result in diarrhoea, or constipation, or both. In this chapter, Hirschsprung’s disease will be used to illustrate the importance of the motor function of the colon. It is a condition in which there is an absence of intramural ganglion cells from the wall of the colon, usually in a distal region (Case 10.1: 1).
Case 10.1
A newborn infant was observed to have a distended abdomen. He had passed very little meconium in the 2 days since he had been born. The doctor examined the infant’s rectum by inserting a finger. The examination revealed that the rectum was empty. However, when the doctor withdrew her finger, there was a gush of meconium, and decompression of the abdomen. The obstruction reoccurred within a day or so. By this time, the child had started to vomit excessively. The symptoms were relieved by an enema. A biopsy of the rectum was performed and Hirschsprung’s disease was diagnosed. An abdominal operation was arranged. The surgeon removed the distal large bowel and sutured the remaining colon to the lower rectum. The child made a good recovery, and his symptoms disappeared.
After examining the details of this case, the following questions arise:
• Why was the infant’s abdomen distended, and why had he passed no meconium since he was born?
• What is the defect in this condition, and what causes it? What did the biopsy reveal?
• Why was it necessary to resect a segment of the infant’s intestine?
• How does this abnormality affect motility in the colon?
• How does the abnormality affect defecation?
Anatomy
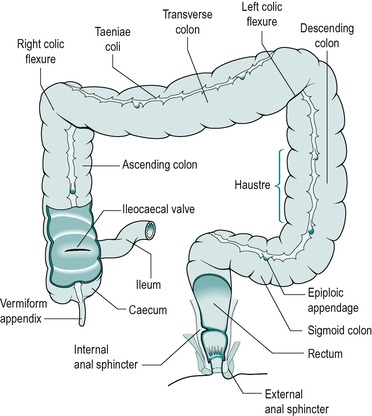
The arrangement of the large intestine and its associated structures is shown in Figure 10.1. It can be divided into various regions: the caecum, the ascending colon, the transverse colon, the descending colon, the sigmoid colon and the rectum. The rectum is the portion beyond the sigmoid colon. The lumen of the colon becomes narrower towards the rectum. The lumen of the rectum, which is wider, provides a reservoir for faecal material, prior to defecation.
The caecum forms a blind-ended pouch below the junctions of the small intestine and the large intestine. The appendix is a small finger-like projection from the end of the caecum. It has no known function in the human. It has a thick wall, and a very narrow lumen that often collects debris.
In the large intestine, the outer longitudinal smooth muscle layer is arranged in three prominent bands, known as taeniae coli. These bands are shorter than the other coats of the colon. There is also a segmental thickening of the circular smooth muscle. Together these features impart a sacculated appearance to the organ. It has no villi (only projections). Its coat is therefore smoother than that of the small intestine, and the consequence of this is that the surface area of the colon is only one-thirtieth that of the small intestine.
The anal canal is the terminal portion of the rectum. It begins at a region where the rectum suddenly becomes narrower. The surface of the upper portion of the anal canal exhibits a number of vertical folds, known as anal (or rectal) columns (Fig. 10.2). These folds are relatively more pronounced in children than in adults. The depressions between the anal columns are known as anal sinuses. The sinuses end abruptly at the lower ends of the columns (the dentate line) where there are small crescent-shaped folds of mucosa oriented around the wall. These folds are termed anal valves. The anal canal is surrounded by sphincter muscle that controls the release of faecal material. The internal sphincter is a thickening of the circular layer of the muscularis externa. The external sphincter, which consists of several parts, is composed of striated muscle. The arrangement of the sphincters is shown in Figure 10.2.
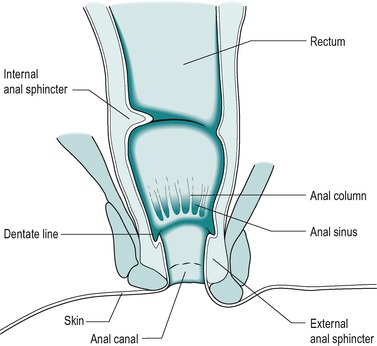 |
| Fig. 10.2 |
Innervation
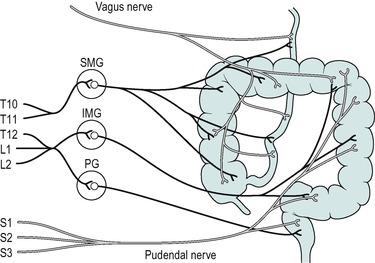
The ascending colon and most of the transverse colon are innervated by the parasympathetic vagus nerve. Beyond that the pelvic nerves innervate the colon. These are the sacral outflow of the parasympathetic nervous system. Figure 10.3 illustrates the extrinsic innervation of the large intestine. The cholinergic parasympathetic nerves synapse with neurones in the intramural plexi. They also synapse directly on the smooth muscle of the colon and the internal anal sphincter. Excitatory cholinergic neurones are also present in the ganglia of the submucosal and myenteric intramural plexi. In Hirschsprung’s disease intramural ganglion cells are absent from the myenteric and submucosal plexi (Case 10.1: 2).
Case 10.1
Defect, diagnosis and treatment
Defect
Hirschsprung’s disease, also known as congenital megacolon (enlarged abdomen), is a familial disease that affects one in 5000 live births. It is more common in males. There is an association with Down’s syndrome. The genetic mechanism is not fully understood, but it involves multiple chromosomal deletions. A similar condition (acquired megacolon) can arise later in life, from a variety of causes (Fig. 10.4).
In Hirschsprung’s disease, intramural ganglion cells are absent from the myenteric and submucosal plexi, usually in a segment of the distal colon. This is due to a defect in embryonic development, involving the arrest of the caudal migration from the neural crest, of the cells that are destined to become ganglion cells of the intramural plexi. Examination of biopsy specimens reveals an absence of ganglion cells from the affected segment. Excitatory and inhibitory neurones are missing. The segment involved is of variable length, in a region extending from the anal canal proximally up the colon. The lumen becomes narrowed in the aganglionic segment, due to tonic contraction of the smooth muscle. The passage of faecal material is obstructed at this narrowed segment and it accumulates in the region proximal to the aganglionic segment. Usually the normal reflex relaxation of the internal anal sphincter in response to distension of the rectum cannot be elicited in this condition. Because the aganglionic segment creates an obstruction to faecal flow, the proximal large bowel becomes chronically distended, giving rise to the name ‘megacolon’.
Diagnosis
The normal reflex relaxation of the internal anal sphincter in response to distension of the rectum usually cannot be elicited in this condition.
A well-known finding in Hirschsprung’s disease is an elevated level of acetylcholinesterase in the narrowed segment. This is indicative of an abnormality of the cholinergic innervation. Diagnosis of Hirschsprung’s disease is by barium enema and biopsy showing an absence of ganglion cells. In cases where the diagnosis is unclear, a histological frozen section of the region can be stained for the enzyme to see if the levels are elevated, to aid the diagnosis.
Treatment
Surgery is effective in correcting the disturbance of motility. Various procedures can be performed, depending on the extent of involvement of the colon. They all involve removal of the aganglionic segment.
The colon is also innervated by adrenergic sympathetic nerves from the lower thoracic and upper lumbar segments of the spinal cord. These nerves synapse with inhibitory nerves in the intramural plexi. They also synapse directly with the smooth muscle of the colon and internal anal sphincter. The external anal sphincter is innervated by somatic motor fibres in the pudendal nerves. It is controlled both reflexly and voluntarily.
Contraction of the levator ani, an external skeletal muscle, constricts the lower end of the rectum. Contraction of another external skeletal muscle, the puborectal muscle that is attached to the external side of the wall of the anal canal, pulls the upper canal forward. This produces a sharp angle between the rectum and the anal canal, and prevents faeces from entering the anal canal, until defecation is initiated. The levator ani and the puborectal muscles are innervated by somatic motor fibres in the pudendal nerve.
Terminals of afferent sensory nerve fibres are present in the mucosa, submucosa and muscle layers of the colon. The colon is fairly insensitive to painful stimuli but it is very sensitive to changes in pressure. Stretching of the colon as a consequence of overdistension results in abdominal pain, but removal of lesions, such as polyps, from the lining of the colon can be achieved painlessly without anaesthetic. There is a profusion of sensory nerve fibres in the wall of the anal canal. Some of these are sensitive to touch, some to cold, some to pressure, and some to friction.
Histology
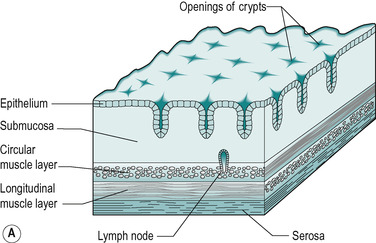
As in other regions of the gastrointestinal tract, the wall of the large intestine is composed of four layers: the mucosa, the muscularis externa, the submucosa and the serosa (Fig. 10.5A).
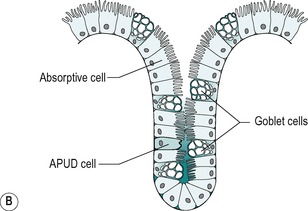
The mucosa contains numerous straight tubular glands that extend through the full thickness of the mucosa (Fig. 10.5B). The surface epithelium of the mucosa and glands consists of simple columnar epithelial cells. The predominant cell type is the columnar absorptive cell. This cell has a thin striated border on its apical surface. In many respects, it resembles the enterocytes of the small intestine. Its main function is to absorb ions and water. However, some nutrients are also absorbed, especially in the proximal colon. There are also goblet cells. These are more numerous in the colon than in the small intestine. They produce mucus, which lubricates the intestine and coats the faecal material, which becomes increasingly more solid as it passes through the colon. This enables it to move along easily. There are also undifferentiated cells, and sparsely distributed APUD cells of various types that secrete hormones into the blood (see Ch. 1). The lamina propria, muscularis mucosa of the colon, and submucosa are similar in the small and large intestines. Nodules of lymphatic tissue are present in the mucosa, and these usually extend into the submucosa. In the region of the junction between the rectum and the anal canal, the muscularis mucosa breaks up into bundles, and further down the anal canal it disappears.
The muscularis externa consists of circular and longitudinal layers of smooth muscle, as elsewhere in the gastrointestinal tract. However, in the large intestine (except for the rectum) the outer longitudinal layer appears to be incomplete. It is arranged in three bands, known as taeniae coli. However, between these bands there is actually a very thin sheet of longitudinal muscle. In the rectum, the outer longitudinal muscle is a uniformly thick layer (as in the small intestine) and this presumably aids defecation. The inner layer of the muscularis externa consists of circular rings of smooth muscle, which allow effective peristalsis as is the case in the small intestine.
The submucosa is similar to that present elsewhere in the gastrointestinal tract. The outer layer is a typical serosa, except where it is in direct contact with other structures (as on much of its posterior surface), when its outer layer is an adventitia.
Ulcerative colitis is a fairly common disease of the large intestine which usually starts in the rectum, and may extend proximally. It is an inflammatory condition where the mucosa becomes ulcerated (Case 10.2 and Case 10.2).
Case 10.2




A 22-year-old woman, who had, for the past 2 years, been experiencing intermittent attacks of diarrhoea and rectal bleeding, visited her general practitioner. She said each attack lasted for several weeks, but there was complete remission of the symptoms between attacks. During the attacks she experienced lower abdominal cramps and sometimes felt feverish. The general practitioner thought the symptoms could be explained by the presence of a number of different conditions, including infection, irritable bowel syndrome and ulcerative colitis, and she decided to send the patient to see a specialist. The patient was referred to an outpatient clinic, and subjected to sigmoidoscopy (direct visual examination of the rectum and distal sigmoid colon) and a radiographic examination of her abdomen. The provisional diagnosis of ulcerative colitis was made on the basis of the finding of inflamed and bleeding mucosa. A rectal biopsy specimen was taken during the procedure, and sent to the pathology laboratory to confirm the diagnosis. A blood sample was taken for determination of plasma electrolytes, blood haemoglobin and plasma albumen. The patient was prescribed aminosalicylate and corticosteroids, and these drugs ameliorated the symptoms of the disease within a week or so.
After studying this case history, we should consider the following questions:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree