Abdominal Pain in Children
Keywords
• Abdominal pain • Pediatric • Children
Abdominal pain is one of the most common reasons pediatric patients seek emergency medical care.1–3 In the emergency department (ED), physicians must distinguish between emergent diagnoses that require immediate intervention, such as appendicitis, intussusception, and ovarian torsion, and self-limiting processes that are amenable to outpatient management and parental/guardian education, such as viral gastroenteritis and constipation. Abdominal pain also may be a presentation of extraabdominal processes, such as pneumonia and asthma.
Physical examination
The physical examination should begin with review of the vital signs. It is important to have knowledge of pediatric normal values for heart rate, respiratory rate, and blood pressure. Rather than memorizing ranges for each age group, it may be helpful to have a reference to which the clinician can refer when caring for a pediatric patient (Table 1).
It is important to focus not only on the abdominal portion of the physical examination of the child with abdominal pain, because extraabdominal causes may also present with abdominal pain. For example, the physician should perform a complete oropharyngeal, lung, back, skin, external genital, and possibly internal genital examination as part of the evaluation as well. When the physician is ready to examine the abdomen, the accuracy of the examination may be improved by using a toy as a distraction tool before auscultation or palpation.2 If the child is already sitting in the lap of their caregiver, it may be useful to perform as much of the examination as possible with the child remaining there. The physician may initially palpate the caregiver’s or a stuffed animal’s abdomen in an effort to show the benign nature of the examination to the child. A school-age child may feel more comfortable if they are allowed to place their hand over or under the physician’s hand as the abdomen is being palpated. Asking the older child questions about school, friends, and activities that they enjoy may serve as a distraction tool and facilitate examination.
Differential diagnosis
It is helpful to consider the differential diagnosis of the child with abdominal pain in terms of the age of the child, because many diagnoses are seen more commonly in children of certain age groups (Table 2).
Diagnoses
Surgical
Appendicitis
Appendicitis is the most frequent surgical cause of abdominal pain in children presenting to EDs or outpatient clinics.4,5 In one-third of children with appendicitis, the appendix ruptures before operative treatment.6,7 This situation is particularly of concern in children less than 4 years of age. In this age group, despite not being a common diagnosis, the prevalence of perforation is high, with rates reported to be as high as 80% to 100%.8–10 Moreover, because the omentum is less developed, perforations are less likely to be localized, leading to generalized peritonitis.2
The pathophysiology of appendicitis in children is different from that of adults because of the changing anatomic location and susceptibility of the appendix throughout childhood.11 For example, neonatal appendicitis is infrequent because of their funnel-shaped appendix, soft diet, recumbent posture, and infrequent gastrointestinal and upper respiratory infections.12,13 Around 1 to 2 years of age, the appendix becomes more susceptible to appendicitis as it assumes the adult shape. As the child ages, lymphoid follicle hyperplasia and size of the appendix gradually increase throughout childhood and peak in adolescence, which represents the highest incidence of appendicitis.8,14
The classic presentation of appendicitis (periumbilical abdominal pain migrating to the right lower quadrant associated with nausea, vomiting, and fever) is seen less often in pediatric patients compared with adults,15 and its presence in children is not so strong a predictor for appendicitis as it is in adult patients.11 Children often present earlier in the clinical process than adults, when only mild or nonspecific signs and symptoms are present. Furthermore, there are limited data indicating that signs such as rebound tenderness and Rovsing sign are accurate in children.16 More common findings of appendicitis in children are right lower quadrant pain, vomiting, abdominal tenderness, and guarding.16 In addition, the appendix may be located deep in the pelvis or rectocecally, which gives rise to back or pelvic pain, rather than the abdominal pain seen with the more common anterior appendix. Although difficult to elicit from caregivers, a history of abdominal pain preceding any emesis can be helpful to distinguish appendicitis from acute gastroenteritis (AGE).2
Laboratory testing can aid in the diagnosis of appendicitis; however, no test is 100% sensitive and specific for the diagnosis. The white blood cell count (WBC),17–19 C-reactive protein (CRP) test,17,18,20–22 and urinalysis (UA) may be useful; however, the WBC count and CRP level may be increased in other conditions and normal in appendicitis. Furthermore, if the inflamed appendix is located adjacent to the ureter, the UA may reveal sterile pyuria or hematuria.23
Many scoring systems using a combination of signs, symptoms, and laboratory results to predict which patients have acute appendicitis have been developed and validated in children. These scoring systems have varying sensitivities (65%–98%) and specificities (32%–92%)24–28 and are rarely used as definitive confirmation of the diagnosis.
Radiologic diagnosis of acute appendicitis before appendectomy has become increasingly more common as its availability in the ED has improved. Plain abdominal radiographs should not be routinely used in evaluating the patient with appendicitis, because only half of patients with surgically proved disease have abnormal findings, most of which are nonspecific.29 Appendicoliths, which are believed to be the most specific finding of acute appendicitis, are visualized in only 5% to 15% of patients.2,30,31 If a radiograph is obtained in the evaluation of the child with abdominal pain, Box 1 lists findings that may be associated with acute appendicitis. Ultrasound has been increasingly used as the modality of choice in pediatric patients because of the lack of radiation exposure and need for contrast agents. As with ultrasound examinations for other indications, the test characteristics of ultrasound for diagnosing acute appendicitis depend on the experience and comfort level of the operator. In experienced hands, ultrasound can achieve sensitivities of 85% to 90% and specificities of 95% to 100%.32–40 Using a graded compression technique, acute appendicitis is defined as an aperistaltic, noncompressible appendix larger than 6 mm in diameter. The presence of periappendiceal fluid may indicate inflammation or an early perforation. If present, an appendicolith may also be visualized by ultrasound. If ultrasound is unavailable, or is obtained and fails to visualize the appendix, a computed tomography (CT) scan becomes the test of choice. Sensitivity has been shown to be 88% to 97%, with specificities of 94% to 97% in pediatric studies,41–43 and it also offers the advantage of identifying complications of appendicitis as well as alternative diagnoses. However, it is slower, may require oral or rectal contrast, which may be difficult to administer to a young child, and carries the risk of significant radiation exposure.
Children are at greater risk than adults from a given dose of radiation because they are inherently more radiosensitive and because they have more remaining years of life during which a radiation-induced cancer could develop.44 Although no large-scale epidemiologic studies of the cancer risks associated with abdominal CT have been reported,44 the cancer risks associated with the radiation exposure from CT scans have been estimated (Fig. 1). By adjusting for current CT usage, it can be estimated that about 1.5% to 2.0% of all cancers in the United States may be attributable to the radiation from CT studies.44 If a CT is determined necessary, the question of which contrast agent or combination of agents to use (oral, intravenous, rectal) is a matter of debate in the radiology literature, is institutional-dependent, and should be decided on in concert with the radiologist or technician performing the study.
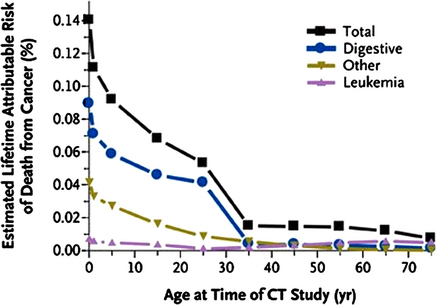
Fig. 1 Estimated lifetime cancer risk from single CT scan of the abdomen.
(From Brenner DJ, Hall EJ. Computed tomography–an increasing source of radiation exposure. N Engl J Med 2007;357(22):2281; with permission.)
Intussusception
Intussusception is second to appendicitis as the most common cause of an acute abdominal emergency in children.45 It is the most common cause of intestinal obstruction in children between 3 months and 6 years of age.45 Although intussusception can occur at any age, the peak incidence occurs between 5 and 9 months of age,46 and about half of patients are less than 1 year of age.47
Intussusception occurs when a segment of bowel (intussusceptum) invaginates into the distal bowel (intussuscipiens) (Fig. 2). This situation results in venous congestion and bowel wall edema initially; however, if unrecognized and untreated, this may lead to arterial obstruction with bowel necrosis and perforation.48,49 Most intussusceptions in children (90%) are ileocolic and idiopathic in nature.50 Presumably, idiopathic intussusception is caused by lymphoid hyperplasia, which has been suggested as the lead point.51 Viral infections caused by adenovirus, rotavirus, and human herpesvirus 6 have been reported to be associated with intussusception.52,53
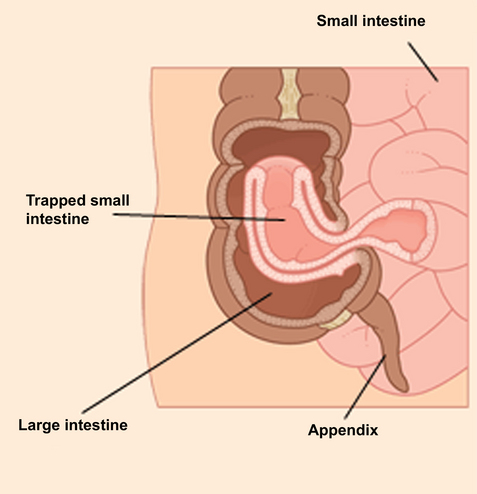
Fig. 2 The mechanism of intussusception.
(From Del Mar, C. Royal Australian College of General Practitioners Complete Home Medical Guide, 2nd ed. Dorling Kindersley Australia; 2006; with permission.)
The clinician should have a high index of suspicion for intussusception in a young child with paroxysmal, colicky abdominal pain and vomiting. The classic triad of intermittent abdominal pain, red currant jelly stool (caused by venous congestion from obstruction), and a palpable mass occurs in a minority of patients (up to 40% of children with intussusception).54,55 More common than grossly bloody stools is the presence of fecal occult blood, which is seen in approximately 50% of patients.45 Therefore, the suspicion of intussusception should prompt the clinician to perform a rectal examination with testing for occult blood. Although it is an unusual presentation, some children with intussusception may present with lethargy or altered mental status, a feature that is postulated to be caused by the release of endogenous opioids secondary to the paroxysms of pain.56,57 In addition, many children present with nonspecific signs and symptoms, which may lead to a delay or missed diagnosis in up to 60% of cases.45 Specifically, infants younger than 4 months have a higher incidence of painless intussusception.55 Also, up to 30% of patients with intussusception have diarrhea,58 and therefore viral gastroenteritis is frequently entertained as the initial diagnosis. Intermittent intussusception is another entity that may prove challenging for the clinician, because these children may have resolution of their symptoms between episodes of obstruction.
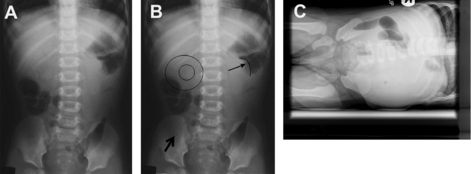
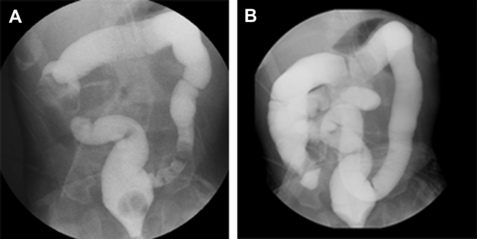
When evaluating a child with suspected intussusception, the first step in diagnosis is obtaining 2 or 3 radiographic views of the abdomen. Left lateral decubitus radiographs are particularly helpful for this diagnosis, because the presence of air in the right lower quadrant makes the diagnosis of intussusception less likely. This situation is because most idiopathic intussusceptions occur at the level of the right upper quadrant, resulting in a paucity or absence of gas in the right lower quadrant, which can be confirmed in the decubitus position. However, plain abdominal films are neither sensitive nor specific for intussusception and may be completely normal in 25% of patients.59 Fig. 3 is an example of the plain radiographs in a patient with intussusception. Table 3 lists other characteristic signs on plain radiograph and ultrasound that may be seen in patients with intussusception.
Table 3 Radiologic findings of intussusception
| Finding | Description | Radiograph or US |
|---|---|---|
| Soft-tissue mass in upper abdomen | Radiograph | |
| Paucity/absence of air in right lower quadrant | Radiograph | |
| Small bowel obstruction | Radiograph or US | |
| Target sign | 2 concentric, circular, radiolucent lines to the right of the spine superimposed on the kidney; caused by right upper quadrant mass with mesenteric fat of intussusceptum | Radiograph |
| Crescent/meniscus sign | Crescent of gas within the colonic lumen that outlines the apex of the intussusception | Radiograph |
| Pseudokidney sign | Hyperechoic tubular center with a hypoechoic rim on both sides, producing a kidneylike appearance in longitudinal plane | US |
| Donut sign | Hypoechoic outer rim of homogeneous thickness (intussuscipiens) with a central hyperechoic core (intussusceptum) representing layers of the intestine within the intestine in transverse plane | US |
Abbreviation: US, ultrasound.
Data from Waseem M, Rosenberg HK. Intussusception. Pediatr Emerg Care 2008; 24(11):794.
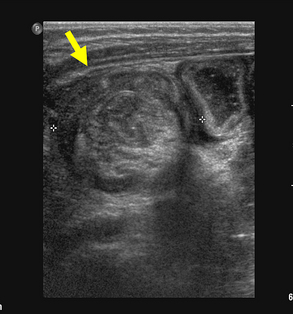
Ultrasound (Fig. 4) has recently emerged as a sensitive (98%–100%) and specific (88%–100%) diagnostic tool for the evaluation of children with suspected intussusception.60–63 However, because ultrasound is operator dependent, its test characteristics for this indication vary depending on the institution. Ultrasound is a noninvasive, rapid, and nonionizing modality, making it an attractive diagnostic option in children. In addition, a lack of perfusion in the intussusceptum detected with color duplex imaging may indicate the development of ischemia. Ultrasound also has the advantage of providing information regarding a pathologic lead point mass, the presence of a small bowel intussusception, information regarding reducibility based on bowel wall findings, and in the identification of alternative diagnoses.60,61,64,65 If ultrasound is unavailable or if an intussusception is identified by ultrasound, the patient should undergo a fluoroscopic barium or air enema, which is both diagnostic and therapeutic.
Treatment of confirmed intussusception begins with fluid resuscitation and maintenance of intravenous fluids, because most patients are dehydrated secondary to vomiting, poor oral intake, and third spacing.45 Because intussusception may become a surgical condition, if radiographic barium or air enema reduction is unsuccessful, it is important that a pediatric surgeon be available before attempted reduction with enema. Nonoperative reduction of intussusception includes air, barium, or aqueous enema, typically under fluoroscopic guidance (Fig. 5). The decision about which agent to use is typically based on the comfort and preference of the radiologist performing the procedure. Success ranges up to 70% for barium66 and 84% for air,67,68 and is influenced by the duration of symptoms, with enema reduction being less successful the longer the delay in diagnosis.69 Some pediatric radiologists have begun to incorporate the use of ultrasound-guided enema reduction as a treatment modality instead of traditional fluoroscopy-guided reduction, which carries the risk of ionizing radiation. This method has been used in other countries and has been shown to be safe and effective.70–72
Operative reduction is required when radiographic enema reduction is either contraindicated, as in peritonitis, perforation, or profound shock,73 or if reduction is unsuccessful.
The risk of recurrent intussusception after reduction is rare but more likely with nonoperative reduction. It has been reported in up to 15% of patients after undergoing hydrostatic reduction and up to 3% after operative reduction.74 The risk is greatest in the first 24 hours after reduction, and therefore some institutions routinely admit these patients during this time for observation.
Volvulus
Midgut volvulus is a surgical emergency in which a loop of bowel twists about its mesenteric attachment. It results from abnormal embryologic rotation of the midgut, known as malrotation. Malrotation occurs during the fifth to eighth week in embryonic life, when the intestine projects out of the abdominal cavity, rotates 270°, then returns into the abdomen. If the rotation does not occur correctly, the intestine does not develop a normal mesenteric attachment and is at risk for later twisting (Fig. 6). In addition, malrotated intestine is prone to obstruction by congenital bands of fibrous tissue (Ladd bands), which develop as a result of abnormal fixation of the colon to the right side of the retroperitoneum. Up to 75% of volvulus cases occur within the first month of life, and most (up to 90%) occur within the first year of life.75,76
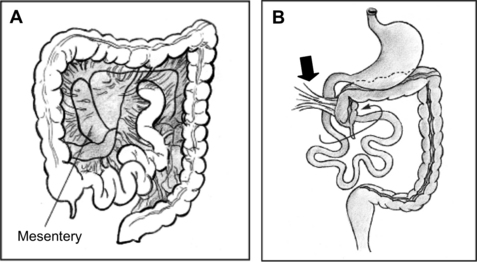
(From National Digestive Diseases Information Clearinghouse. Anatomic problems of the colon. NIH Publication No. 05–5120, February 2005. Available at: http://digestive.niddk.nih.gov/ddiseases/pubs/anatomiccolon/#Volvulus. Accessed January 3, 2009.)
Volvulus requires early detection in order to prevent irreversible loss of bowel. It should be suspected particularly in young infants with bilious emesis, and any infant with bilious vomiting should be considered to have a volvulus until proved otherwise. Volvulus may also present as failure to thrive, with severe feeding intolerance.77 Pain and irritability are not prominent features in the neonate.78 The abdomen is usually soft and nontender to palpation until strangulation of the bowel has developed, when it becomes distended and tender and the infant begins to have hematochezia.79 In addition, an infant with already ischemic or necrotic bowel may present in shock and rapidly deteriorate clinically if the diagnosis is not recognized and surgically corrected.
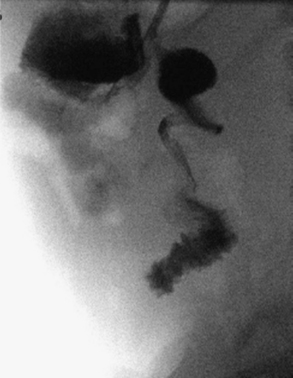
The evaluation of a child with suspected volvulus should begin with abdominal plain films. These films may show a classic double-bubble sign (air bubbles located in the stomach and duodenum), other signs consistent with intestinal obstruction such as a paucity of gas, air-fluid levels, and dilated loops of bowel, or the radiograph most commonly may be entirely normal. Definitive diagnosis is made with an upper gastrointestinal (UGI) series to assess for the position of the ligament of Treitz. Normally the ligament of Treitz should be located at the level of the pylorus and just to the left of midline, with the second portion of the duodenum coursing posteriorly on a lateral view.80 The classic finding is that of the small intestine rotated to the right side of the abdomen (indicating malrotation), with contrast narrowing at the site of obstruction causing corkscrewing (indicating a volvulus) (Fig. 7). When the diagnosis is still in question, a contrast enema may provide additional information by showing an abnormal cecal position in association with malrotation.81
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree