(1)
Department of Gastrointestinal Surgery, Kameda Medical Center, Kamogawa, Japan
Keywords
Laparoscopic left colectomyFascial compositionFusion fasciaSubperitoneal fascia7.1 Introduction
In laparoscopic left colectomy (LapLC), the mobilization of the sigmoid colon and the splenic flexure of the colon are necessary. Although the surgical technique in the splenic flexure of the colon is not easy due to the thickened omentum, it is ensured with an understanding of the fascial configuration. With regards to lymph node dissection, the region of the inferior mesenteric artery (IMA) is a dissection region and it is important to dissect around the left colic artery (LCA).
7.2 Resection Range and Degree of the Lymph Node Dissection
LapLC is similar to open left colectomy in terms of resection range and degree of lymph node dissection, except for the approach to the abdominal cavity. In the left colon including the splenic flexure of the colon, lymph flow is mostly to the IMA due to its embryological hindgut origin. Therefore, it is necessary to dissect from the LCA [1–3].
7.3 Fascial Composition and Fusion Fascia of the Left Colon and the Splenic Flexure of the Colon
The root of the transverse mesocolon is on the caudal edge of the pancreatic body and tail, and the mesocolon spreads out from there in a characteristic fan-shape (Fig. 7.1). The dorsal mesentery consists of two sheets originally and then becomes four sheets, forming the omentum between the stomach and the transverse colon. A third sheet of the dorsal mesentery becomes the dorsal wall of the omental bursa, while the fourth sheet of the dorsal mesentery and the ventral leaf of the transverse colon are fused (Fig. 7.2). To understand the fascial composition, it is easier if one considers the relationship between the omentum (i.e. dorsal mesentery) and the transverse mesocolon in two stages during the intestinal rotation. In the longitudinal section as shown in Fig. 7.3a, the omentum and the mesocolon have no relation; however, they subsequently form a fusion fascia as shown in Fig. 7.3b.
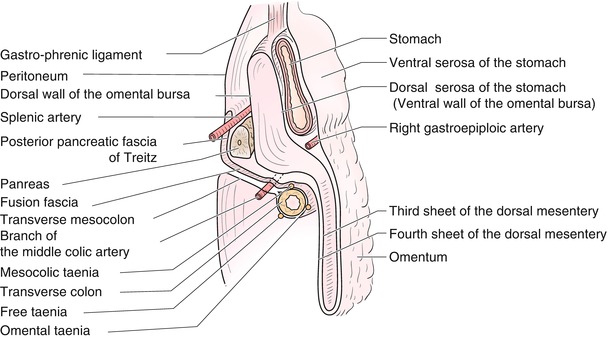
Fig. 7.1
Relationship between the transverse colon and the descending colon. The root of the transverse colon is on the caudal edge of the pancreatic body and tail. The fourth sheet of the dorsal mesentery and the ventral leaf of the transverse colon are fused
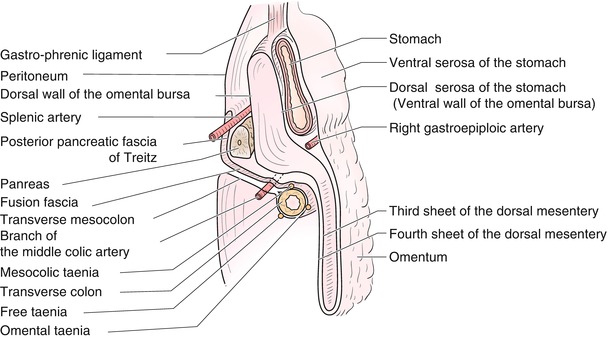
Fig. 7.2
Relationship between the stomach and the transverse colon. The third sheet of the dorsal mesentery becomes the dorsal wall of the omental bursa, and the fourth sheet of the dorsal mesentery and the ventral leaf of the transverse colon are fused
Fig. 7.3
Relationship between intestinal rotation and the transverse mesocolon. In the longitudinal section during the intestinal rotation, the omentum (dorsal mesentery), and the mesocolon have no relation (a); however, they form a fusion fascia when the intestinal rotation is completed (b)
The splenic flexure of the colon is defined as the terminal one-third of the anal side of the transverse colon leading to the first portion of the descending colon [4]. It is the site of transition between the transverse colon having a certain degree of mobilisation and the descending colon with fixation to the retroperitoneum by fusion (Fig. 7.1).
The left mesocolon forms the left fascia of Toldt in fusion with the peritoneum of the dorsal abdominal wall (Fig. 7.4). However, in the sigmoid colon the fan-shaped sigmoid fossa is typically formed behind the sigmoid mesocolon due to incomplete fusion of the dorsal mesentery and retroperitoneum (Fig. 7.4b). Thus, the mobilisation of the left colon requires dissection between the left fusion fascia of Toldt and the deep subperitoneal fascia. The only anatomical landmarks for this dissection are the spermatic vessels and the ureter (Fig. 7.4 dotted line).
Fig. 7.4
Fascial composition of the left colon. The only anatomical landmarks for dissection between the fusion fascia of Toldt and the deep subperitoneal fascia are the spermatic vessels and the ureter [5, with permission]
In addition to the fusion between the transverse colon and the omentum and the fusion between the descending colon and the retroperitoneum, it is also necessary to further consider the relationships between the omentum and the diaphragm and between the omentum and the spleen.
In the fixation of the splenic flexure of the colon, there are two fixing ligaments to consider. The first is the left colo-phrenic ligament, which connects the splenic flexure of the colon and the diaphragm. The colo-phrenic ligament is considered to be formed upon closure of the left protrusion of the bursa omentalis (Figs. 7.5 and 7.6c, d). The second is the colo-splenic ligament. It is a secondary vertical ligament formed by the parietal peritoneum between the splenic flexure of the colon and the spleen or by the leftmost part of the transverse mesocolon (Figs. 7.5 and 7.6d).
Fig. 7.5
Relationship between the omentum and the colo-phrenic ligament/colo-splenic ligament. The colo-phrenic ligament is considered to be formed from the left protrusion of the bursa omentalis that has been closed. The colo-splenic ligament is a secondary vertical ligament formed by the parietal peritoneum between the splenic flexure of the colon and the spleen or by the leftmost part of the transverse mesocolon
Fig. 7.6
(a–d) Fascial configuration of the transverse colon, descending colon and the splenic flexure of the colon. There is a variation in the fascial configuration of this part determined by the degree of entry of the omentum between the spleen and the transverse colon. Two hanging bends called the colo-phrenic ligament and the colo-splenic ligament are visible (d)
From the above, it is important to understand that the clinical anatomy of the splenic flexure of the colon is a three-way relationship including the transverse colon and the omentum (dorsal mesentery), the descending mesocolon and the deep subperitoneal fascia, and two fixing ligaments – the left colo-phrenic ligament and the colo-splenic ligament.
After dividing the omentum from the omental taenia, the dissection of the omentum is initiated by entering the layer between the third sheet of the dorsal mesentery and the fusion fascia (i.e., between the fourth sheet of the dorsal mesentery and the ventral leaf of the transverse colon) at the taenia coli. This layer can continue to be dissected towards the left side, so the splenic flexure of the colon can be pulled away caudally (Figs. 7.3c and 7.6a, b). To continue these manoeuvres to the ventral side of the deep subperitoneal fascia in the descending colon, the left fusion fascia of Toldt is divided (Fig. 7.6c). Thus, along this course, the hanging band – the left colo-phrenic ligament and the colo-splenic ligament – can be cut unknowingly in the splenic flexure of the colon (Fig. 7.6d).
However, there are notable differences in the amount of omentum located at the splenic flexure of the colon, and in some cases, a large amount of omentum is interposed. Therefore, the principle of dissection and dividing is to maintain a dissecting surface that is as close as possible to the serosa of the colon.
If the procedure through the omental bursa is performed, it is necessary to enter the dorsal side of the third sheet of the dorsal mesentery at the leftmost side of the omental bursa and to divide the left fusion fascia of Toldt (Fig. 7.7a–d).
Fig. 7.7




(a–d) Procedure through the bursa omentalis. If the procedure through the omental bursa is performed (a), it is necessary to enter the dorsal side of the third sheet of the dorsal mesentery at the leftmost side of the omental bursa (b) and to divide the left fusion fascia of Toldt (c). The procedure through the omental bursa requires more omentum to be separated in order to continue to the dissection layer of the descending colon, and thus is more complicated
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








