Inflammatory Bowel Disease
Chronic idiopathic inflammatory bowel disease (IBD) includes two chronic gastrointestinal disorders of unknown etiology: Ulcerative colitis (UC) and Crohn disease (CD). The natural history of IBD differs from patient to patient. Disease severity at its onset, disease extent, and patient age at the time of diagnosis, along with other variables, determine overall disease severity and the likelihood of subsequent morbidity and mortality. Once established, IBD patients suffer episodic acute attacks that become superimposed on chronic disease. As a result, the patient is likely to suffer from disabling disease for decades.
General Clinical and Epidemiologic Features of Inflammatory Bowel Disease
The annual incidence of IBD in the United States is approximately 6 cases per 100,000 persons (1). Both CD and UC are predominantly diseases of young adults, with a peak incidence occurring between 15 and 30 years of age. Age-specific incidence rates by sex are slightly greater for males with UC and for females with CD (2). At age 10, both diseases rapidly increase in incidence. Overall, both UC and CD show three peaks in incidence rates. The first and highest peak occurs between ages 20 and 24, the second at ages 40 to 44, and the third at ages 60 to 64 years. In females, the first peak appears at ages 15 to 19, 5 years younger than in males (3). By age 60, the incidence of UC exceeds that of CD.
Ethnicity
Epidemiologic studies show that the incidence and prevalence of IBD vary significantly depending on geographic location and patients’ racial or ethnic backgrounds. IBD occurs worldwide and exhibits a relatively low incidence in Asian, Mediterranean, and Middle Eastern countries and a higher incidence in European countries, the United States, Canada, Australia, and New Zealand. This may reflect racial, ethnic, and genetic factors. Prevalence rates for IBD among non-Caucasians in the United States are lower than rates for Caucasians. In one study, the prevalence of Crohn disease was 43.6 per 100,000 population for Caucasians, 29.8 per 100,000 for African Americans, 5.6 per 100,000 for Asians, and 4.1 per 100,000 for Hispanics (4). A study of African-American children reported a Crohn disease incidence of 7 to 12 cases per 100,000 (5). However, recent data indicate that the incidence of IBD among African Americans and second-generation South Asians is increasing (6). Among ethnic groups, Jews in the United States have the greatest risk for developing IBD compared with non-Jewish Caucasians. The incidence rate is two to four times greater and the prevalence two to nine times greater in this group. Ashkenazi Jews exhibit a particularly high IBD risk, especially those originating in Middle Europe, Poland, or Russia.
Etiology
Chronic IBD is a common inflammatory disorder of unknown etiology. The intrinsic complexity of IBD and its variable manifestations hampers progress in understanding its pathogenesis. However, currently favored theories implicate genetically determined, immunologically mediated mechanisms of injury. The fundamental pathogenic question could be: Does the chronic recurring inflammatory activity in IBD reflect an appropriate response to a persistently abnormal stimulus (a structural alteration of the intestine or causative agent in the environment) or an abnormally prolonged response to a normal stimulus (aberrant regulation of immune responses) (Fig. 11.1)? It is conceivable that some factors initiate the disease, whereas others sustain the inflammatory process or possibly even reactivate it.
Genetic Factors
There is considerable evidence that the development of both CD and UC is determined, at least in part, by genetic factors. Overwhelming evidence exists that both ulcerative colitis and Crohn disease cluster within families. In population-based studies, 5% to 10% of individuals with IBD report having an affected family member (7). In fact, having a family member with IBD represents the greatest risk factor for developing the disease. Individuals with a first-degree relative with IBD have a 10- to 15-fold increased risk of also developing the disease compared with those without an affected family member (8). Approximately 75% of families
with multiple affected members show concordance for disease type (i.e., all affected family members have CD disease or all have UC). In the remaining 25%, some members have CD while others have UC (9). This finding suggests that UC and CD may have some common, as well as distinct, susceptibility genes. Twin studies show that monozygotic twin concordance for CD ranges from 42% to 58% (10). In contrast, concordance in dizygotic twins is only 4% (11). Monozygotic twin concordances are significantly lower for UC (10). These findings suggest that although there is a strong genetic component that determines susceptibility to inflammatory bowel disease, there are also environmental factors that play an important role in disease development.
with multiple affected members show concordance for disease type (i.e., all affected family members have CD disease or all have UC). In the remaining 25%, some members have CD while others have UC (9). This finding suggests that UC and CD may have some common, as well as distinct, susceptibility genes. Twin studies show that monozygotic twin concordance for CD ranges from 42% to 58% (10). In contrast, concordance in dizygotic twins is only 4% (11). Monozygotic twin concordances are significantly lower for UC (10). These findings suggest that although there is a strong genetic component that determines susceptibility to inflammatory bowel disease, there are also environmental factors that play an important role in disease development.
Susceptibility Genes
Genetic linkage studies have identified a number of potential genetic susceptibility loci for inflammatory bowel disease. Some of these genes appear to confer a general risk for development of IBD, while others confer specific risk for either UC or CD. These are listed in Table 11-1.
IBD1
The IBD1 locus is located in the pericentromeric region of chromosome 16 and shows disease linkage only for CD, not for UC. This locus contains the gene NOD2/CARD15 that has now been definitively identified as the gene responsible for disease linkage to this chromosomal region. The family of Nod proteins includes NOD2/CARD15 as well as several additional regulatory proteins. The Nod proteins contain a central nucleotide-binding domain and an N-terminal caspase recruitment domain (12). In addition, they possess a C-terminal leucine-rich repeat (LRR) region that bears a high degree of homology with plant genes known to be involved in disease resistance. This finding suggests that Nod proteins may play a similar role in mammals (12).
NOD2 is expressed in monocytes, intestinal epithelial cells, and intestinal Paneth cells. This protein recognizes and binds muramyl dipeptide, the biologically active moiety of bacterial peptidoglycan, resulting in activation of the proinflammatory cytokine NF-κB (13). It is the leucine-rich repeat region of the protein that functions in peptidoglycan recognition. Human mutations in NOD2 occur in both the LLR and in the central nucleotide-binding domain. Three major mutations have been described in the LRR, all of which are associated with Crohn disease (14,15). Interestingly, these mutations occur predominantly in Caucasian populations and are extremely rare in Asian and African-American populations (16,17). Mutations in the nucleotide-binding domain result in Blau syndrome, a rare disease characterized by early-onset granulomatous arthritis, uveitis, and skin rash.
Patients who have one defective copy of NOD2 demonstrate a two- to fourfold increased risk for the development of Crohn disease, while homozygous mutants show a 20- to
40-fold increased risk (15,18). Approximately 8% to 17% of CD patients carry two mutant NOD2 alleles. NOD2 mutations are associated with disease onset at a young age, disease located in the small intestine, and stricturing and fistulizing forms of the disease (14,15,19,20). The Crohn disease–associated mutations in the LRR of NOD2 all result in inactivation of the protein with a resultant defect in the cellular response to peptidoglycan (16). This abnormality on monocytes could result in an inability of the innate immune system to recognize bacterial products and a subsequent overreaction to bacteria by the adaptive immune system. In addition, defective NOD2 function in intestinal epithelial and Paneth cells may result in an abnormal immunologic response to normal commensal bacteria within the gut (21).
40-fold increased risk (15,18). Approximately 8% to 17% of CD patients carry two mutant NOD2 alleles. NOD2 mutations are associated with disease onset at a young age, disease located in the small intestine, and stricturing and fistulizing forms of the disease (14,15,19,20). The Crohn disease–associated mutations in the LRR of NOD2 all result in inactivation of the protein with a resultant defect in the cellular response to peptidoglycan (16). This abnormality on monocytes could result in an inability of the innate immune system to recognize bacterial products and a subsequent overreaction to bacteria by the adaptive immune system. In addition, defective NOD2 function in intestinal epithelial and Paneth cells may result in an abnormal immunologic response to normal commensal bacteria within the gut (21).
TABLE 11.1 Major Susceptibility Loci for Inflammatory Bowel Disease (IBD) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
IBD2
The IBD2 gene locus lies on chromosome 12 and appears to be more closely linked to the development of UC than CD (22). A number of possible candidate genes are located in this region, but investigation of several of these has yielded negative results.
IBD3
Several studies have linked the IBD3 locus, located on chromosome 6, to both ulcerative colitis and Crohn disease (22,23). Recent data suggest that this region may be specific to men (24). This region contains the major histocompatability complex (MHC), as well as the tumor necrosis factor (TNF) gene. Several human leukocyte antigen (HLA) associations with IBD are well known. Among Caucasians, susceptibility to ulcerative colitis has been convincingly linked to the HLADRB1*0103 allele. In addition, this allele is associated with severe colitis and extraintestinal manifestations of UC. In Japanese and Jewish populations, susceptibility to UC has been linked to the HLADRB1*1052 allele. Polymorphisms in TNF-α and their relationship to Crohn disease risk are also under current investigation.
IBD5
The IBD5 locus resides on chromosome 5q31-q33. It was identified by a genomewide scan of Canadian families with early-onset CD. Heterozygous carriage of the risk alleles increased the risk for developing CD twofold, while homozygous carriage increases this risk by sixfold (25). IBD5 may also be associated with risk for development of UC (25). The specific causative gene has not yet been identified. Candidate genes include organic cation transporter genes 1 and 2, interferon regulatory factor isoform 1, PDZ and LIM domain protein (PDLIM4), and prolyl 4-hydroxylase (P4HA2).
Immunologic Factors
Both CD and UC represent, at least in part, disorders of both innate (macrophage, neutrophil) and acquired (T and B cell) immunity. It is currently believed that the main abnormality responsible for the development of inflammation in these disorders is a loss of tolerance to enteric commensal bacteria or other pathogens (26). In normal individuals, tolerance is mediated by regulatory T cells, B cells, natural killer T cells, and dendritic cells that produce transforming growth factor beta (TGF-β), interleukin (IL)-10, interferons, and prostaglandin J2. In IBD, lamina propria macrophages and dendritic cells are increased in number, demonstrate an activated phenotype, and express many proinflammatory cytokines and chemokines. In addition, expression of costimulatory molecules and adhesion molecules, vital to the extravasation of macrophages
and neutrophils from the vasculature, is also increased in both CD and UC (27).
and neutrophils from the vasculature, is also increased in both CD and UC (27).
TABLE 11.2 Cytokine Production in Inflammatory Bowel Disease | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Crohn disease is associated predominantly with TH1 cytokine production (28). Ulcerative colitis, on the other hand, does not fit clearly into either the TH1 or TH2 category, although an atypical or modified TH2 response seems to occur in established UC (26). Although the types of cytokines produced in UC and CD differ somewhat (Table 11.2), both diseases are associated with abnormal immune responses to nonpathogenic commensal bacteria within the gut. Cross-reactivity of peripheral blood and colonic lamina propria CD4+ T cells with indigenous flora in patients with UC and CD suggests that abnormal T cell–specific immune responses to the normal flora of the host are important in the pathogenesis of both diseases (29).
In normal individuals, pathogens are recognized by germline encoded pattern recognition receptors on epithelial cells, neutrophils, macrophages, and dendritic cells. These pattern recognition receptors include lectins, mannose receptors, complement receptors, scavenger receptors, Nod proteins, and toll-like receptors (TLRs). At least ten different TLRs have been described, each of which recognizes a different bacterial factor. Activation of TLRs ultimately results in expression and activation of NF-κB (30). NF-κB is activated in the tissues of IBD patients, where it is thought to have proinflammatory activity. NF-κB stimulates expression of many molecules that likely play a role in IBD including IL-1β, TNF, IL-6, IL-8 and other chemokines, ICAM1 and other adhesion molecules, CD40, CD80, CD86, and the T-cell stimulator ICOS (31). NF-κB also stimulates expression of protective molecules including TNF-induced protein 3, CARD15, cyclo-oxygenase 2, β defensins, and peroxisome proliferator-activated receptor (PPAR)-γ(31).
Activated T lymphocytes are regulated by both effector and regulator T-cell subpopulations in healthy gut mucosa. Effector T cells are capable of inducing intestinal inflammation, while regulator T cells are able to control or prevent inflammation. The immunosuppressive function of the regulator cells is mediated through production of IL-10 and TGF-β. These regulator cells are thought to play pivotal roles in mediating tolerance toward luminal antigens. Genetically engineered IL-10–deficient mice develop severe transmural inflammation of the small and large intestine reminiscent of CD (32). In addition, studies suggest that defects in the IL-10 and TGF-β regulatory signaling pathway may exist in humans with UC (33).
Activation of effector cytotoxic T cells and cytokine release result in generation of activated matrix metalloproteinases, enzymes that are mediators of tissue destruction. In addition, cytokines act directly on the microvasculature, up-regulate adhesion molecules, and enhance recruitment of additional effector cells including neutrophils and macrophages, which amplify and perpetuate the inflammatory response and contribute to additional tissue injury.
As a result of these immunologic events, the mucosa becomes heavily infiltrated by inflammatory cells. Soluble inflammatory mediators produced by neutrophils, lymphocytes, monocytes, fibroblasts, mast cells, neuroendocrine cells, and nerves generate many of the functional and histologic changes that characterize the disease (Fig. 11.2). One sees a large number of activated T and B cells, increased immunoglobulin secretion, the presence of anticolon antibodies (34), and aberrant expression of class II HLA molecules (35).
T-cell profiles differ between patients with Crohn disease and those with ulcerative colitis. As previously mentioned, CD is characterized primarily by a TH1 response. TH1 responses are mediated by IFN-γ, the production of which is stimulated by IL-12. Patients with CD also exhibit a TH17 response, associated with IL-17 production. IL-17 expression is stimulated by IL-6, TGF-β, and IL-23. In patients with ulcerative colitis, the T-cell profile has been more difficult to characterize, but may represent an atypical TH2-type response. This atypical TH2 response may be mediated by natural killer T cells that secrete IL-13 (36).
Autoantibodies
Populations of mucosal B cells and plasma cells increase in UC, a finding that initially suggested that the disease was antibody mediated and complement dependent. In addition, patients with UC demonstrate circulating autoantibodies including those directed against human intestinal tropomyosin isoform as well as anticolonocyte antibodies (34,37). This production of antiself antibodies is now thought to represent a phenomenon that is a secondary protective response aimed at clearing apoptotic cells.
Patients with UC also commonly demonstrate the presence of circulating antineutrophil cytoplasmic antibodies (ANCAs) (38,39). Antineutrophil cytoplasmic antibodies were initially described as sensitive and specific markers for active Wegener granulomatosis but are now known to occur in a wide range of diseases. The antigens recognized by ANCAs are by definition cytoplasmic, predominantly localizing to the primary granules of neutrophils. ANCAs exhibit two distinct patterns on ethanol-fixed human neutrophils: (a) a coarse granular cytoplasmic staining (C-ANCA) or (b) a perinuclear staining pattern (P-ANCA). The perinuclear staining pattern results from redistribution of the cytoplasmic antigen to the nucleus. Serine proteinase 3, cathepsin G, and elastase are the antigens to which C-ANCAs react and myeloperoxidase is the usual antigen to which P-ANCAs react in patients with vasculitis. In contrast, a unique subset of P-ANCAs characterizes UC patients. The identity of the antigen is unclear.
The prevalence of a positive P-ANCA in UC patients ranges from 49% to 86% (40,41). The perinuclear ANCA pattern is 93% to 97% specific (39), but only 46% to 60% sensitive for the diagnosis (42). P-ANCAs are also found in up to 25% of patients with CD (40,43). Titers of these antibodies, however, do not correlate with the degree of severity of the associated colitis, and although they may serve as a convenient clinical marker for UC, their role in the pathogenesis of the disease is unclear. Interestingly, a recent report suggests that P-ANCA in UC may represent a cross-reacting antibody to an antigenic target on Escherichia coli and Bacteroides bacterial strains (44).
The absence of P-ANCAs in the serum defines one population of CD patients, whereas a smaller number of patients are positive for P-ANCA. CD patients with serum P-ANCA expression exhibit a UC-like clinical phenotype (45). One hundred percent of CD patients with P-ANCA have symptoms of left-sided colitis with clinical and histopathologic features of UC. The patients also express a rare allele (R241) of the intercellular adhesion molecule-1 (ICAM1) gene, suggesting the possibility that R241 is a marker for a CD–UC overlap syndrome (46).
Apoptosis
In normal mucosa, the inflammatory response is terminated by induction of apoptosis in activated T cells once the pathogen has been eliminated. However, in CD, mucosal T lymphocytes are resistant to apoptosis, leading to their accumulation and persistence of the inflammatory response (19,47). In UC patients, T cells are more susceptible to Fas-mediated apoptosis. In addition, Fas ligand is strongly expressed by T cells in active UC, but not in CD, suggesting the Fas-Fas ligand-induced apoptosis contributes to mucosal damage in UC (48).
Exogenous Agents
Numerous data suggest that environmental factors play a role in the development and progression of both forms of IBD. Susceptibility genes for both UC and CD are known to demonstrate incomplete penetrance. As noted earlier, concordance rates for monozygotic twins are >50% for Crohn disease and <10% for UC. This finding suggests that factors other than genotype must be involved in the pathogenesis of IBD. In addition, the incidence of IBD has increased in the
developed parts of the world over the last 50 years, and is now becoming increasingly common in less developed countries as they become more industrialized and the standard of living improves. Environmental changes that might affect development of the mucosal immune system or the indigenous enteric flora include improved hygiene, consumption of sterile or at least noncontaminated foods, childhood vaccinations, and increased age at first exposure to a variety of intestinal pathogens.
developed parts of the world over the last 50 years, and is now becoming increasingly common in less developed countries as they become more industrialized and the standard of living improves. Environmental changes that might affect development of the mucosal immune system or the indigenous enteric flora include improved hygiene, consumption of sterile or at least noncontaminated foods, childhood vaccinations, and increased age at first exposure to a variety of intestinal pathogens.
Exogenous agents, including diet, infections, smoking, and other environmental factors, all may play an etiologic role in IBD. Environmental influences related to certain forms of industrial pollution may also account for the recent increase in CD incidence in certain countries.
Food Antigens
Numerous studies have demonstrated that exposure to food-associated antigens plays an important role in the gastrointestinal inflammation that occurs in patients with CD. In addition, patients treated with simplified or elemental diets containing proteins in the form of amino acids or small peptide fragments improve symptomatically and show decreased endoscopic or serologic evidence of inflammation (49). Rectal exposure of CD patients to a series of food antigens resulted in increased rectal blood flow and lymphocyte proliferation in comparison to non-CD control patients (50), a finding that suggests that patients with CD show gut-specific sensitization to food antigens. Reactions were seen with yeast and citrus antigens, although individual patients reacted also to other antigen groups. Although it is possible that this sensitivity to food antigens is merely a reflection of exposure to antigens through mucosal defects, the absence of similar sensitivities in patients with UC makes this possibility unlikely (50). It is not likely, however, that exposure to food-associated antigens represents the primary abnormality in patients with CD. Instead, exposure to food in the proximal gastrointestinal tract may lead to sensitization and stimulation of the immune system in genetically susceptible individuals.
Infectious Agents
For many years investigators have been suspicious that IBD may have an infectious etiology. These suspicions are based on several observations. First, CD patients have an increased incidence of childhood infections including pharyngitis, tonsillitis, and rhinitis (51). In addition, gastroenteritis in early infancy has been linked to later development of CD (52). Furthermore, studies have shown that patients with CD tend to have increased serum levels of antibodies directed against nonpathogenic as well as pathogenic enteric organisms (53). Many studies have attempted to link IBD to infections with Mycobacteria, Yersinia, and several viruses. However, no definitive link with any one infectious agent has ever been made.
Current evidence, instead, suggests that the resident bacterial flora of the gut may be a factor in initiating and propagating the inflammation in IBD. In CD patients, T lymphocytes are hyperreactive to bacterial antigens, a factor that suggests that local bacterial tolerance mechanisms may be abnormal in these individuals (54). Patients with both UC and CD show higher numbers of bacteria attached to their intestinal mucosa than do unaffected individuals (55). In addition, bacterial invasion of the mucosa has been reported in both UC and CD patients (56). IBD patients also have increased mucosal production of IgG antibodies directed against a wide range of commensal organisms (57). The clinical observation that, in some patients, disease flares may be ameliorated by antibiotic administration is supportive of a bacterial role. Finally, recent evidence suggests that the NOD2 CD susceptibility gene is involved in regulation of host responses to bacterial organisms (12). Overall, many view inflammatory bowel disease as a disease initiated by a general loss of tolerance for the commensal bacteria of the gut.
Tobacco Use and Exposure
The association between tobacco use and development of IBD is well established. Smoking decreases the risk for the development of UC, but exacerbates and aggravates Crohn disease (58,59). Former smokers have a lower risk of UC than do those who never smoked. In addition, exposure to passive smoke also appears to confer a lessened risk of developing UC relative to nonexposed nonsmokers (60). Overall, the effect of smoking appears to be dose dependent (61). Interestingly, nicotine has been shown to have an inhibitory effect on TH2 lymphocyte function, the type of cells most implicated in UC (62). Indeed, nicotine-based enemas have been demonstrated to be beneficial in patients with milder forms of distal colitis. Nicotine has no effect on TH1 cells characteristic of the Crohn inflammatory response. Tobacco use is also associated with protection against sclerosing cholangitis and pouchitis in UC patients (61,63).
Intestinal Permeability
Increased intestinal permeability may play a role in the pathogenesis of CD. Increased permeability not only occurs in the intestines of patients affected by the disease, but also in their unaffected first-degree relatives (64). It has been suggested that this increased permeability may represent a predisposing factor to the development of CD because a leaky intestinal barrier may intensify antigen absorption, leading to exaggerated systemic immune stimulation.
Appendectomy
Appendectomy early in life (before the age of 20) has been shown in several studies to decrease the risk of developing UC (65,66). Interestingly, the risk for UC is reduced only in patients who undergo appendectomy for acute appendicitis,
and not in those whose appendices are removed because of nonspecific abdominal pain or incidentally during surgery for other causes. This finding suggests that the appendicitis that results in appendectomy, rather than appendectomy itself, is protective. Alternatively, there may be other factors among patients destined to develop UC that prevent those individuals from developing appendicitis. A recent report suggests that the risk for Crohn disease may also be decreased in patients who have undergone appendectomy (67).
and not in those whose appendices are removed because of nonspecific abdominal pain or incidentally during surgery for other causes. This finding suggests that the appendicitis that results in appendectomy, rather than appendectomy itself, is protective. Alternatively, there may be other factors among patients destined to develop UC that prevent those individuals from developing appendicitis. A recent report suggests that the risk for Crohn disease may also be decreased in patients who have undergone appendectomy (67).
Other Environmental Factors
Epidemiologic data suggest that use of nonsteroidal anti-inflammatory drugs (NSAIDs) can exacerbate existing UC, and may even induce it de novo (68). This effect was initially attributed to the cyclooxygenase (COX)-1 inhibitory effect of the drugs, but recent reports suggest that even COX-2–specific inhibitors also demonstrate this effect (69). Possible mechanisms by which NSAIDs exert these effects include inhibition of protective mucosal prostaglandin production and increased leukocyte migration and adherence. It has been estimated that NSAID use increases the risk of IBD exacerbation by as much as 30%.
As many as 40% of UC patients report that psychological stress represents a trigger for their disease (70). There is evidence to link psychological stress with increased susceptibility to infection and illness through stress-related impairment of the immune system. Some animal models suggest that stress may play a role in the development of colitis. Cotton-top tamarinds, primates that spontaneously develop colitis and serve as a model for human IBD, develop colitis only in long-term captivity (71).
Occupation
Differences in IBD incidence exist among individuals with different occupations. Occupations involving work in the open air and physical exercise appear to protect against development of IBD, whereas exposure to air-conditioned, artificial working conditions or extended and irregular shifts can confer an increased IBD risk (72).
Crohn Disease
Incidence
As noted previously, there has been a steady rise in the incidence and prevalence of CD in Western Europe, Canada, and the United States over the past several decades. The incidence of CD ranges from 3.4 to as many as 14.6 per 100,000 in differing Western countries (1,73). CD affects all ages and both sexes, but its incidence peaks in the 2nd and 3rd decades of life. A second minor peak in incidence occurs in patients aged 50 to 70 years. Crohn disease is more common among Caucasians than among other racial groups, and is more frequent in Jewish than non-Jewish populations (4,5).
Multiple Forms of Crohn Disease
Recent epidemiologic evidence suggests that there are two forms of CD: One inherently indolent (nonperforating), which tends to recur slowly, and another inherently aggressive (perforating), which tends to evolve more rapidly. Patients with the relatively aggressive “perforating” type of CD are more prone to develop fistulae and abscesses, whereas the more indolent “nonperforating” type tends to lead to stenotic obstruction. The latter associates with an exaggerated inflammatory response and an exaggerated proinflammatory cytokine response (74). Host responses determine which form of CD becomes manifest in any individual, and differences in cytokine expression between the two forms of CD might have diagnostic, investigative, and therapeutic implications (74).
Clinical Features
The signs and symptoms of CD are often subtle, frequently resulting in a delay in diagnosis until months, or sometimes years, after symptom onset. However, the diagnosis can usually be made on the basis of a careful clinical history, physical examination, and diagnostic testing. The presentation of a patient with CD depends in large part on the location, extent, and severity of gastrointestinal involvement. Crohn disease most frequently affects the ileocecal region, followed (in decreasing order of frequency) by the terminal ileum alone, diffuse involvement of the small bowel, and isolated colonic disease (75). Because the clinical manifestations of CD are very diverse, both in the sites of tissue involvement and in the severity of the inflammation, a wide spectrum of clinical manifestations results (Table 11.3).
TABLE 11.3 Clinical Features of Crohn Disease Related to Site of Bowel Involvement | |
|---|---|
|
Patients with ileocolonic disease experience intermittent episodes of crampy, often postprandial, abdominal pain. Pain may be referred to the periumbilical region, especially in children (75). The abdominal discomfort may be accompanied by loose stools. Stools are small, frequent at night, loose to watery, but not usually overtly bloody. Such symptoms are often attributed to dietary factors or irritable bowel disease. The past history commonly includes perirectal or perianal abscesses and fistulae. Physical examination may localize tenderness to the right lower quadrant. Occasionally, an inflammatory mass may be palpable. Patients with diffuse small intestinal Crohn disease present with diffuse abdominal pain, diarrhea, anorexia, and weight loss. Malabsorption may also occur. These patients demonstrate diffuse abdominal tenderness on physical examination. Colonic CD may mimic ulcerative colitis. Patients complain of diarrhea often containing blood and/or mucus and crampy lower abdominal pain that may be relieved with defecation. Crohn colitis is characterized by more extensive bleeding, more perianal disease, and less pain than Crohn ileitis.
Growth retardation occurs in many pediatric patients with CD, and may occur before other disease signs or symptoms develop. The growth failure and malnutrition result from inadequate dietary intake, malabsorption, and increased nutritional requirements, and, in treated patients, from drug therapy, particularly corticosteroids.
Progressive transmural inflammation with scarring and deep ulceration may ultimately lead to symptoms associated with intestinal obstruction, perforation, bleeding, or fistula formation. When obstruction develops, it usually does so in the distal ileum. Extensive mucosal ulceration predisposes the patient to bacterial translocation with all of its complications, including a predisposition to bacterial endocarditis (76). Patients also demonstrate altered small intestinal motility with abnormal receptor-mediated small intestinal contraction (77). Deep linear ulcers or fistulae may sometimes give rise to profound lower GI bleeding.
A sudden worsening of clinical symptoms and/or an unusual disease presentation should alert one to the possibility of ischemia or viral infection superimposed on pre-existing CD. Ischemia may develop secondary to vasculitis, or may occur because of endothelialitis resulting from infection with cytomegalovirus (CMV), particularly if immunosuppressive therapy has been utilized.
Anorectal Disease
Anorectal complications are common in patients with CD. In some patients, these anorectal symptoms may be the most troubling aspect of their disease. Approximately one quarter of patients with CD involving the small bowel and three quarters of individuals with colonic CD will have an anal lesion sometime during the course of their disease (78). Anorectal complications are more likely to occur during severe attacks when the colon is extensively involved. Perianal involvement may predate, postdate, or develop concurrently with primary intestinal CD.
Perianal disease consists of thickened, indurated, perianal skin with tags, scarring, erosions, superficial ulcers, cavitating ulcers, excoriation, fissures, fistulae, abscesses, and blind sinus tracts (79). Perianal abscesses affect about 25% of patients with CD. Persistence or healing of perianal lesions does not correlate with intestinal activity. Of the various perianal lesions, those that tend to persist are the anal skin tags. Persistent fistulae may remain asymptomatic but many also heal spontaneously. New fistulae may also form (79).
Jejunal Disease
The term regional jejunitis is used to describe a variant of CD that manifests initially or predominantly as jejunal disease. It rarely coexists with duodenal CD. More often it occurs as part of diffuse jejunoileitis. It also manifests as a particularly devastating and sometimes fatal pattern of CD recurrence following surgery for ileitis. The lesion may be confused with ulcerating jejunitis.
Appendiceal Disease
Sometimes CD initially presents in the appendix (Fig. 11.3), making it very difficult to differentiate from ordinary appendicitis because of the similarity of the clinical symptoms. The distinction between these two entities is most easily made if granulomas are found in the appendix.
Esophageal Disease
Esophageal CD occurs, although it is rarer than oral, pharyngeal, or laryngeal involvement. Esophageal disease affects 6% of CD patients (80). Esophageal lesions include aphthous ulcers measuring 2 to 3 mm in size, strictures, esophagitis,
esophageal ulcers, and granulomas. The diagnosis should not be made unless typical lesions are found elsewhere in the gut.
esophageal ulcers, and granulomas. The diagnosis should not be made unless typical lesions are found elsewhere in the gut.
Gastric Disease
Gastric CD typically involves the distal stomach producing thickening and granulomatous inflammation of the gastric wall, which results in pyloric obstruction and vomiting. Patients often have concomitant duodenal disease. Gastric CD may antedate small bowel involvement, and some of the reported cases of isolated granulomatous gastritis may actually represent early gastric CD. The diagnosis can only be made with certainty if there is associated CD in the small bowel or colon.
Endoscopy exhibits antral stenosis and rigidity; aphthous ulcers; nodules; thickening and blunting of the gastric folds associated with mucosal cobblestoning and denudation; fibrosis; and ultimately stricture formation. Antral stenosis is the most characteristic feature of gastric involvement. Gastric fistulae usually originate from the intestine with direct extension to the stomach (81). Features of gastric CD grossly and radiologically mimic gastric carcinoma or other inflammatory conditions.
Duodenal Disease
CD produces pathologically and radiologically typical lesions in the duodenum in approximately 0.5% to 4% of patients (81). Duodenocolic or duodenoileal fistulae develop, originating in the diseased duodenum or from previous ileocolic anastomoses. Duodenal–enteric fistulae also complicate CD arising in other parts of the gastrointestinal (GI) tract. Usually, but not invariably, duodenal CD coexists with ileal involvement and the duodenal lesions frequently extend proximally to involve the gastric antrum or distally into the jejunum (Fig. 11.4). The clinical features include symptoms of duodenal obstruction and/or ulceration. Duodenal CD predisposes patients to develop pancreatitis. Rare patients with duodenal disease develop massive upper GI hemorrhage.
Crohn Disease in the Elderly
About 5% of patients develop CD after age 60 (82). Older patients range in age from 64 to 85, tend to have a longer delay in diagnosis, have more hematochezia, and have a higher incidence of coexisting diverticular and vascular disease. Elderly patients often have less pain, a palpable abdominal mass, less
small bowel disease, less drug treatment, and no family history of IBD; elderly patients are also less likely to have small intestinal disease. In some series, nearly all patients presenting with CD after age 60 have large bowel involvement (83). Older individuals may have more distal Crohn colitis (Fig. 11.5) than younger patients, who tend to have more extensive colonic involvement. Coexisting anorectal disease may clinically masquerade as diverticulitis. The most reliable hallmarks of CD in older persons include the presence of anorectal disease, rectal bleeding, and fistulae. The anal area may show edematous skin tags, ulcers, fissures, and fistulae. Elderly patients require total colectomy more frequently than those in the younger age groups (84).
small bowel disease, less drug treatment, and no family history of IBD; elderly patients are also less likely to have small intestinal disease. In some series, nearly all patients presenting with CD after age 60 have large bowel involvement (83). Older individuals may have more distal Crohn colitis (Fig. 11.5) than younger patients, who tend to have more extensive colonic involvement. Coexisting anorectal disease may clinically masquerade as diverticulitis. The most reliable hallmarks of CD in older persons include the presence of anorectal disease, rectal bleeding, and fistulae. The anal area may show edematous skin tags, ulcers, fissures, and fistulae. Elderly patients require total colectomy more frequently than those in the younger age groups (84).
Patient Misdiagnosis
Some patients are diagnosed with CD who do not have the disease. Two major reasons account for such a mistaken diagnosis: (a) diseases in organs adjacent to the ileocecum produce a clinical syndrome of acute right lower quadrant pain and inflammation, which could suggest the diagnosis; and (b) neoplastic, vascular, infectious, or other small intestinal diseases mimic CD. Table 11.4 lists diseases that can mimic CD clinically.
Association with Other Diseases
CD associates with extraintestinal diseases that represent part of the inherent disease process (see Extraintestinal Manifestations). Additionally, CD associates with other diseases as listed in Table 11.5.
Extraintestinal Manifestations
Approximately 25% of patients with known CD have a history of at least one extraintestinal manifestation. Multiple
extraintestinal manifestations occur in the same patient more frequently than would be expected by chance. Large bowel involvement and longer disease duration predispose the patient to extraintestinal manifestations.
extraintestinal manifestations occur in the same patient more frequently than would be expected by chance. Large bowel involvement and longer disease duration predispose the patient to extraintestinal manifestations.
TABLE 11.4 Diseases Clinically Mimicking Crohn Disease | |
|---|---|
|
TABLE 11.5 Crohn Disease: Associations | |
|---|---|
|
Need for Surgical Intervention
The majority of patients with CD undergo surgery at some time during their lives. Approximately 42% of children with CD require surgical intervention as compared with only 5% of those with UC (85), and approximately 20% require surgical intervention within the first year of diagnosis (86). The remainder undergo surgery at a rate of 5% per year (87). CD patients typically require repeated operations, with 63% of patients undergoing a repeat operation by the 15th postoperative year.
In general, radical resection does not decrease the recurrence rate of the disease, and repeated resections place patients at risk for the development of short bowel syndrome. Therefore, conservative surgical techniques have evolved in recent times to treat patients with CD-associated complications not amenable or responsive to medical therapy. Surgery in CD patients is indicated for treatment of abdominal abscesses, internal or external fistulae, bleeding, and bowel obstruction secondary to strictures, and in patients with medically intractable disease. Many patients experience recurrence of their disease, but many also report an overall improvement in their quality of life following surgery.
Recurrence of Crohn Disease
CD is a recurring chronic illness, with 94% of patients experiencing recurrent disease. Nearly all patients have a recurrence within 10 years of their initial diagnosis. Recurrence occurs most commonly in patients with ileocecal disease (53%) compared with isolated colonic disease (45%) or isolated small bowel disease (44%) (88). Patients who have undergone surgical procedures are particularly prone to recurrent disease. Ileal recurrence is determined in part by the retrograde reflux of the colonic fecal stream, microvascular injury, and ischemia (89,90). Additionally, increased use of acetaminophen and other nonnarcotic analgesics and increased consumption of simple sugars sometimes heralds the development of recurrent disease. For patients whose original disease was ileitis, recurrent disease almost invariably appears just proximal to the ileocolonic anastomosis. For those with an initial colitis or ileocolitis, recurrence develops on either side or both sides of the anastomosis.
Patient Survival
Patients with Crohn disease develop a large number of complications, some of which impact patient survival. Patient survival is not influenced by disease extent at the time of diagnosis. Patients die both from their underlying IBD as well as from associated diseases, including GI cancer, respiratory diseases, and other GI diseases.
Gross Features
The gross features of the bowel reflect the stage of the disease, with the most severe lesions being seen in advanced transmural disease. Patients with severe disease are those most likely to come to resection. Thus, the pathologist is only likely to see the gross pathology of advanced disease.
Lesion Distribution
CD classically involves the distal 15 to 25 cm of the terminal ileum, often in association with disease involving the right colon, but any part of the GI tract may become involved (Table 11.6). Thus, CD can involve the mouth, esophagus, stomach, duodenum, proximal jejunum, ileum, large intestine, and anus. Ileocolic, small intestinal, and upper gastrointestinal CD occurs in approximately 30% to 50%, 25% to 50%, and 5% to 30% of all cases, respectively. Disease limited
to the colon affects 15% to 30% of patients (91,92). The terminal ileum is involved in about 5% of Crohn colitis patients. The involved segments of small intestine vary from 5 to 76 cm in length with an average of 20 cm. Transition from involved to uninvolved areas is usually abrupt in the small bowel, but is less well defined in the large intestine.
to the colon affects 15% to 30% of patients (91,92). The terminal ileum is involved in about 5% of Crohn colitis patients. The involved segments of small intestine vary from 5 to 76 cm in length with an average of 20 cm. Transition from involved to uninvolved areas is usually abrupt in the small bowel, but is less well defined in the large intestine.
TABLE 11.6 Gastrointestinal Forms of Crohn Disease | |
|---|---|
|
Grossly, colonic CD shows three major patterns: (a) diffuse (almost total involvement), (b) stricture formation, and (c) disease mainly confined to the rectum. Any of these forms can exist in isolation or can coexist with other gastrointestinal lesions, especially those involving the terminal ileum. In the colon, diffuse mucosal disease with relatively less involvement of deeper structures can produce an inflammatory pseudopolypoid mucosal pattern indistinguishable from UC, except for its patchy distribution. Patients with CD have a normal rectum in approximately 50% of cases.
External Gross Features
The external surface of the bowel appears reddened, hyperemic, and covered with serosal exudates producing serositis (Fig. 11.6). Areas of serositis appear rough and nodular, often coexisting with dense fibrous adhesions between bowel loops or fixation of the bowel to other abdominal organs, pelvic organs, or the abdominal wall. Fat encircles the antimesenteric serosal surface, producing a pattern known as “creeping fat” (Figs. 11.7 and 11.8). Miliary serosal lesions, the macroscopic equivalent of granulomas, may be seen. The miliary lesions appear as multiple, minute, white nodules resembling peritoneal seeding by carcinoma or the serosal tubercles characteristic of tuberculosis. They are usually distributed along the serosal lymphatics and may be seen on the surface of the adjacent mesentery and peritoneum. These may represent an early stage of the disease. Initially, the
intestinal wall remains pliable, even though it may appear slightly thickened (Figs. 11.7 and 11.8). With disease progression, the bowel becomes increasingly fibrotic and rigid (Fig. 11.8). Eventually, strictures may develop, usually in the area of the distal ileum at the area of the ileocecal valve (Fig. 11.6). Large inflammatory pseudotumors may form at this site, simulating a carcinoma (Fig. 11.6). Granulomata within the lymph nodes are grossly visible as tiny gray-white specks (Fig. 11.9).
intestinal wall remains pliable, even though it may appear slightly thickened (Figs. 11.7 and 11.8). With disease progression, the bowel becomes increasingly fibrotic and rigid (Fig. 11.8). Eventually, strictures may develop, usually in the area of the distal ileum at the area of the ileocecal valve (Fig. 11.6). Large inflammatory pseudotumors may form at this site, simulating a carcinoma (Fig. 11.6). Granulomata within the lymph nodes are grossly visible as tiny gray-white specks (Fig. 11.9).
Internal Gross Features
The earliest grossly visible mucosal change consists of the formation of an aphthous ulcer overlying lymphoid tissue. As these ulcers enlarge, they may develop a hemorrhagic rim that makes them visible. In their early stages, aphthous ulcers are most easily seen in the colon (Fig. 11.10) because villi tend to obscure their presence in the small intestine. It is important to note that aphthous ulcers are not specific for CD, but may also occur in infectious enterocolitis (see Chapters 6 and 13). In some patients, these tiny ulcers are the only or predominant sign of the disease, whereas in other patients they associate with more severe changes elsewhere in the bowel. Recognition of discrete ulcers in areas of otherwise normal mucosa may precede the development of more flagrant changes of CD by weeks or years.
The small, stellate, aphthous ulcers enlarge into discontinuous, serpiginous, or linear ulcers that then enlarge to form wide-based ulcers (Fig. 11.11). At this stage the mucosa appears reddened and swollen. The ulcers ultimately coalesce longitudinally and transversely. Grossly, the disorder is characterized by segmentally or diffusely arranged serpiginous or longitudinal furrowed ulcers with areas of intervening normal-appearing mucosa. The deep fissuring ulcers of CD differ from the superficial ulcers present in UC. The mucosa demonstrates islands of nonulcerated mucosa interspersed among ulcerated areas (Fig. 11.11), producing a cobblestoned appearance. This feature is also not specific for CD because it occurs in other conditions, such as ischemia.
When the linear ulcers heal, long railroad track–like scars remain (Fig. 11.12). Ulcers often lie close to the resection margins of the specimen and, if left in the patient, may form the basis of recurrent disease. Transmural inflammation predisposes the longitudinal ulcerations to become fissures or fistulae secondarily involving adjacent organs or the abdominal wall. Eventually, dense adhesions form.
When the linear ulcers heal, long railroad track–like scars remain (Fig. 11.12). Ulcers often lie close to the resection margins of the specimen and, if left in the patient, may form the basis of recurrent disease. Transmural inflammation predisposes the longitudinal ulcerations to become fissures or fistulae secondarily involving adjacent organs or the abdominal wall. Eventually, dense adhesions form.
 FIG. 11.10. Endoscopic view of aphthous ulcers. Aphthous ulcers appear as erythematous “pimplelike” mucosal lesions. The aphthous ulcers are outlined by the arrows. |
With disease progression, the cut surface of the bowel demonstrates full-thickness inflammation, scarring, and fibrosis of the submucosa, muscularis propria, and serosa. The fibrosis is superimposed on other macroscopic features. Intervening normal bowel separates diseased bowel segments, creating skip areas. This patchy pattern of inflammation contrasts with the continuous pattern of inflammation and prominent rectal involvement seen in UC. The mucosa may even become atrophic in longstanding disease.
Abscesses, Fissures, and Fistulae
Fistulae and adhesions (see Figs. 11.9 and 11.13) occur less commonly in patients with colonic involvement than in those with small intestinal disease. Internal and external fistulae form in up to 60% of patients (93). Fistulae occur spontaneously, and are more frequent in patients who have
had previous surgery and who had residual diseased bowel. If the process remains localized, an abscess forms (Fig. 11.14). Vaginal fistulae commonly occur because of the anatomic proximity of the diseased rectal mucosa to the vagina. They may also result from extension of perirectal abscesses.
had previous surgery and who had residual diseased bowel. If the process remains localized, an abscess forms (Fig. 11.14). Vaginal fistulae commonly occur because of the anatomic proximity of the diseased rectal mucosa to the vagina. They may also result from extension of perirectal abscesses.
Intra-abdominal abscesses develop in patients with CD. These abscesses may be intraperitoneal or, less commonly, retroperitoneal. There is marked preponderance of males in the retroperitoneal abscess group (93).
Perforation only affects 1.5% of CD patients (see Fig. 11.13) (94) because the inflammatory process penetrates the tissues slowly, causing loops of inflamed bowel to adhere to one another, thereby walling off any free perforation that might occur. Perforations result from deep penetration of fissures or fistulae through the bowel wall, from ingestion of some medicines, or from complicating ischemia (Fig. 11.15) or superimposed infection. Patients may also undergo spontaneous free rupture of an abscess into the peritoneal cavity.
Strictures
CD is characterized by strictures in the small and large intestine and in the anorectum. These strictures commonly lead to partial, intermittent obstruction. Strictures and fistulae are more common with ileitis, ileocolitis, and perianal disease than with disease predominating in the colon. The nature of the obstructive symptoms depends on the part of the bowel that is affected. The most severe stenosis usually affects the ileocecal valve. Multiple strictures may be present (Fig. 11.16). The strictures result
from transmural inflammation, fibrosis, scarring, and fibromuscular proliferation. Rectal strictures are not unique to CD because they also complicate other disorders (Table 11.7).
from transmural inflammation, fibrosis, scarring, and fibromuscular proliferation. Rectal strictures are not unique to CD because they also complicate other disorders (Table 11.7).
Pseudopolyps
Pseudopolyps develop in CD. Many of these are inflammatory in nature, whereas others represent residual mucosal islands (Fig. 11.17). Giant pseudopolyps sometimes form in the colon. These large polyps measure up to 5 cm in height and 2 cm in diameter, and project into the colonic lumen. The lesions have a predilection to involve the transverse colon and splenic flexure, but they occur anywhere in the large intestine. The surfaces exhibit a cribriform appearance and may contain inspissated feces. In addition to the presence of bulky, lobulated polyps, one may also see narrow, tall, filiform polyps.
 FIG. 11.15. Crohn disease complicated by ischemic colitis. The ischemic area is in the upper right-hand portion of the mucosa and is covered by a fibrinous pseudomembranous exudate. |
Histologic Features
General Comments
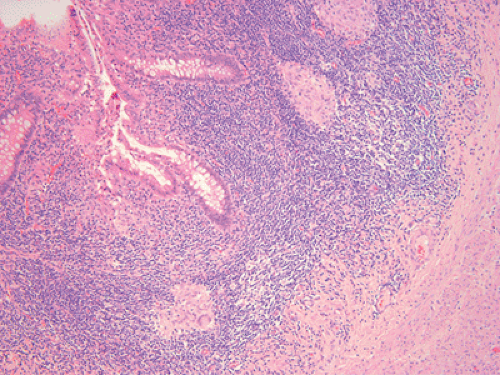
The ease of making the diagnosis of CD depends on whether one examines biopsy or resection specimens. Resection specimens are more likely to exhibit all of the classic changes of CD, especially those that typically affect the deeper layers of the bowel wall (Table 11.8). The features of CD were originally described in the landmark article published by Crohn and Ginsberg in 1932 (95). Irregularly distributed aphthous-type ulcers, nodular lymphoid aggregates, irregular hypertrophy of the muscularis mucosae, proliferation of submucosal nerves, and loosely organized granulomas occur in various combinations within the mucosa and the submucosa (Fig. 11.18). The biopsy diagnosis of CD remains more problematic because only the mucosa and superficial submucosa are available for examination. In addition, many of the histologic features, including the presence of granulomas, are relatively nonspecific. The pattern and distribution of changes in biopsies are frequently characteristic enough to allow one to suggest that CD is present and/or enable one to exclude other diagnoses that might be in the differential diagnosis.
TABLE 11.7 Rectal Strictures: Etiology | |
|---|---|
|
Epithelial and Mucosal Changes
The patchy distribution of CD results in an epithelium that exhibits a range of changes, depending on whether or not the tissues are examined early or late in the course of the disease and whether the tissues come from more normal or more diseased parts of the bowel. The epithelium ranges in appearance from completely normal, to acutely damaged, to regenerative
(Fig. 11.19). In longstanding CD, the crypts and villi show marked distortion of the normal architecture. Distorted glandular architecture is characterized by areas of glandular irregularity and branching (Figs. 11.20 and 11.21). This feature is best appreciated in sections of crypts cut in a plane perpendicular to the muscularis mucosae. In sections cut parallel to the muscularis mucosae, regenerated crypts can be recognized by the presence of cross sections of glands that show variable diameters (Fig. 11.22) and an uneven distribution.
(Fig. 11.19). In longstanding CD, the crypts and villi show marked distortion of the normal architecture. Distorted glandular architecture is characterized by areas of glandular irregularity and branching (Figs. 11.20 and 11.21). This feature is best appreciated in sections of crypts cut in a plane perpendicular to the muscularis mucosae. In sections cut parallel to the muscularis mucosae, regenerated crypts can be recognized by the presence of cross sections of glands that show variable diameters (Fig. 11.22) and an uneven distribution.
 FIG. 11.17. Mucosal polyposis. Irregularly sized cobblestonelike structures are present. They represent residual islands of mucosa. The clefts between them represent linear ulcers. |
TABLE 11.8 Resection Features That Suggest a Diagnosis of Crohn Disease | |
|---|---|
|
Distorted glands often show epithelial hyperplasia (Fig. 11.23), crypt abscesses, epithelial cell degeneration, and ulceration (Figs. 11.24 and 11.25). In the small intestine, villi become distorted or atrophic and one commonly sees pyloric metaplasia, especially in the ileum. The presence of distorted villi and/or crypts and areas of pyloric metaplasia or increased numbers of Paneth cells, especially in the left colon, indicates that the disease is chronic in nature.
The mucosa often appears cobblestoned and mildly polypoid, but not to the extent seen in UC. Although focal crypt abscesses affect patients with CD, they are often not as numerous as in UC. Regenerative changes occur at ulcer margins, but the mucosa away from ulcers may appear normal except for a lymphoplasmacytic infiltrate in the basal part of the lamina propria. Goblet cell depletion and reactive epithelial cells are present only in areas of severe inflammation. Active apoptosis affects the deeper parts of the glands. Areas of mucosal fibrosis may be predictive for CD. In patients with chronic disease, the mucosa may exhibit localized areas of hyperplasia lined by prominent and hyperplastic goblet cells (Fig. 11.23).
Aphthous and Other Ulcers
Two distinctive types of ulceration affect both the small and large intestines. The first is the histologic equivalent of the grossly evident aphthous ulcer. This lesion develops even before inflammatory cells diffusely infiltrate the lamina propria.
Antigen entry into M cells might lead to the proliferation of antigen-sensitized cells and granuloma formation. The underlying lymphoid nodule may contain giant cells or granulomas. As the lesion progresses, it superficially ulcerates, obliterating its associated lymphoid follicle (Figs. 11.24 and 11.25). A thin stream of mucus, neutrophils, and inflammatory debris exudes from the ulcer mouth and empties into the bowel lumen (Figs. 11.24 and 11.25). The ulcers progressively enlarge, forming a continuum with the larger ulcers normally seen in CD (Fig. 11.26). Larger ulcers may eventually become lined by a single layer of atrophic cuboidal epithelial cells. There is an associated reduction in the number of crypts and loss of villi in the small bowel.
The second type of ulcer is the knifelike fissure, which occurs at right angles to the long axis of the bowel (Fig. 11.27). These may extend through the bowel wall and are likely the basis for fistula formation. Fissures branch and penetrate deeply into the underlying bowel wall, producing adhesions, fistulae, abscesses, and peri-intestinal inflammatory pseudotumors (Fig. 11.28). Fissures contain acute inflammatory cells and a granulation tissue lining with conspicuous pale, plump histiocytic cells. The latter resemble the epithelioid histiocytes seen in granulomas. Giant cells may also be present.
Healed ulcers result in architectural distortion, pyloric metaplasia (Fig. 11.29), and a thickened or duplicated muscularis mucosae often associated with a marked dense
submucosal fibrosis. As a result, it is often impossible to distinguish the muscularis mucosae from the submucosa or underlying muscularis propria. Fibroblasts and myofibroblasts proliferate in these areas of fibrosis, usually with accompanying chronic inflammatory cells. Fibrosis extends from the bowel wall to involve adjacent structures and traps within it lobules of fat that may demonstrate variable degrees of fat necrosis.
submucosal fibrosis. As a result, it is often impossible to distinguish the muscularis mucosae from the submucosa or underlying muscularis propria. Fibroblasts and myofibroblasts proliferate in these areas of fibrosis, usually with accompanying chronic inflammatory cells. Fibrosis extends from the bowel wall to involve adjacent structures and traps within it lobules of fat that may demonstrate variable degrees of fat necrosis.
Mucosal Metaplasia
Patients with chronic disease often develop pyloric metaplasia (Fig. 11.29), especially in the ileum. The large intestine often develops Paneth cell metaplasia. In the small bowel, the number of Paneth cells may increase, although they are normally present in this location.
The cells in pyloric metaplasia, also known as aberrant pyloric glands, have also come to be known as ulcer-associated cell lineage (UACL) cells (96). This distinctive cell lineage typically arises in sites of enteric ulceration, most notably in the ulcerated gut in CD. The pyloric glands usually occur singly or in clusters in the mucosa adjacent to ulcer margins. They are also found near single discrete ulcers in the edematous segments away from involved mucosal areas.
These cells share many features of pyloric and Brunner glands, although they do not extend deeper than the muscularis mucosae, a feature that distinguishes them from Brunner glands. The regular acinar glands have a coiled tubular neck and therefore the entire neck is rarely seen in a single section. They extend down to, but usually not through, the muscularis mucosae and have a number of terminal branches that are given off at right angles to the neck,
so that they are usually seen in cross section. The glands are lined by clear or pale-staining columnar cells containing indistinct neutral mucin granules. The nuclei appear oval or round and are located near the base of the cell. The glandular structures have a looser architectural pattern than either pyloric or Brunner glands (96).
so that they are usually seen in cross section. The glands are lined by clear or pale-staining columnar cells containing indistinct neutral mucin granules. The nuclei appear oval or round and are located near the base of the cell. The glandular structures have a looser architectural pattern than either pyloric or Brunner glands (96).
Lymphatic Dilation (Lymphangiectasia)
Another notable feature of CD is submucosal lymphatic dilation (Fig. 11.30), which commonly coexists with edema and lymphoid hyperplasia. Plasma cells, eosinophils, and neutrophils may infiltrate along the dilated vessels. In more advanced stages of the disease, fibrous tissue replaces the edema.
Nature of the Inflammatory Infiltrate
Early morphologic lesions include increased numbers of mucosal plasma cells, lymphocytes, macrophages, mast cells, eosinophils, and neutrophils in all layers of the bowel wall. A basal lymphocytic–plasmacytic infiltrate occupies the lower part of the mucosa (Fig. 11.31). In active IBD, one sees a constant emigration of neutrophils and monocytes from the circulation into the inflamed mucosa and through the epithelium into the intestinal lumen. Neutrophils infiltrate the intestinal epithelium, forming the lesion known as cryptitis.
Collections of granulocytes within the crypt lumens are called crypt abscesses (Fig. 11.32). Variable edema and/or fibrosis are present, depending on the stage of the disease (see Fig. 11.18). The inflammatory infiltrate often also surrounds submucosal and serosal lymphatics and blood vessels, where they penetrate the muscularis propria. Denser lymphocytic aggregates also lie in the submucosa away from the lymphatics or they may appear scattered throughout all layers of the bowel wall (see Fig. 11.18).
Collections of granulocytes within the crypt lumens are called crypt abscesses (Fig. 11.32). Variable edema and/or fibrosis are present, depending on the stage of the disease (see Fig. 11.18). The inflammatory infiltrate often also surrounds submucosal and serosal lymphatics and blood vessels, where they penetrate the muscularis propria. Denser lymphocytic aggregates also lie in the submucosa away from the lymphatics or they may appear scattered throughout all layers of the bowel wall (see Fig. 11.18).
 FIG. 11.25. Crohn disease. Further extension of the aphthous ulcer. There is more extensive inflammation and wider area of ulceration extending from the aphthous ulcer than one sees in Figure 11.24. |
An early but nonspecific finding of CD is an increased number of eosinophils and macrophages (Fig. 11.33) in the lamina propria beneath the surface epithelium. Eosinophils degranulate in ulcerated areas, leading to deposition of eosinophil cationic protein and cathepsin G. These proteins contribute to the inflammatory process (97).
Mucosal and submucosal mast cell hyperplasia and degranulation also represent constant features of both UC and CD. Mucosal mast cells maintain a direct association with substance
P (SP)-containing nerves, as well as with capillaries, blood vessels, Schwann cells, nerve fibers, myofibroblasts, and collagen fibers. They also lie along epithelial cells, providing an anatomic basis for communication between nerves and the immune system. Inflammatory mediators released from mast cells contribute to the pathophysiology of CD due to the release of preformed and newly generated inflammatory mediators (98). The bowel develops focal edema and inflammation in the lamina propria, submucosa, and deeper layers, even in the presence of a more or less normal-appearing mucosa.
P (SP)-containing nerves, as well as with capillaries, blood vessels, Schwann cells, nerve fibers, myofibroblasts, and collagen fibers. They also lie along epithelial cells, providing an anatomic basis for communication between nerves and the immune system. Inflammatory mediators released from mast cells contribute to the pathophysiology of CD due to the release of preformed and newly generated inflammatory mediators (98). The bowel develops focal edema and inflammation in the lamina propria, submucosa, and deeper layers, even in the presence of a more or less normal-appearing mucosa.
Dendritic cells lie adjacent to granulomas and fissures. The number of macrophages in the lamina propria increases. They are arranged in bandlike zones at the bottom of ulcers or fissures, perhaps playing a scavenging role directed against microbial agents or dietary substances penetrating the GI wall through the mucosal defects. Aggregates of macrophages lead to the formation of noncaseating granulomas.
Lymphoid Aggregates
Lymphoid aggregates, which may contain germinal centers, generally lie at the mucosal–submucosal junction. Lymphoid aggregates form even in the absence of granulomas, and they may be more helpful than granulomas in establishing the diagnosis of CD (Figs. 11.18 and 11.34). Lymphoid aggregates occur in both CD and UC; however, when they lie in the submucosa or deeper in the bowel and are separated from the muscularis mucosae, and when the lymphoid aggregates coexist with submucosal edema or fibrosis in the presence of an intact mucosa, the diagnosis is more likely to be CD than UC. Prominent lymphoid aggregates also commonly affect the serosal fat in CD. Finally, the lymphoid tissue of the terminal ileum may become hyperplastic, forming multiple lymphoid polyps.
Granulomas
Compact sarcoidlike granulomas are the sine qua non for the diagnosis of CD (Figs. 11.35 and 11.36) and, when present, are a reliable histopathologic criterion for differentiating CD from UC. Granulomas assume particular diagnostic significance when seen in tissues remote from areas of ulceration in situations where foreign body granulomas are unlikely. Although the presence of granulomas represents a useful diagnostic feature for CD, they can be seen in various other
conditions (see Table 11.9).
conditions (see Table 11.9).
TABLE 11.9 Differential Diagnosis of Granulomas in the Intestine | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Pathologists should be cautious when diagnosing a granuloma in biopsy material. Ruptured crypts release mucin into the lamina propria, stimulating the formation of mucin granulomas (Fig. 11.37). Such mucin granulomas may include mature macrophages and foreign body–type giant cells. They can be recognized because of the predominance of giant cells, their association with and orientation around perforated crypts (Fig. 11.37), and their positivity for mucin stains. Mucin granulomas are not specific for CD because they occur in any situation that results in crypt destruction with epithelial cell loss, including UC.
 FIG. 11.30. Lymphangiectasia in Crohn disease. This section from the ileum of a patient with Crohn disease shows prominent dilation of the lymphatics in the submucosa and deep mucosa. |
 FIG. 11.31. Basal plasmacytosis in inflammatory bowel disease. The lamina propria of the deep mucosa contains numerous plasma cells. Scattered lymphocytes and eosinophils are also present. |
The reported frequency with which granulomas are identified in CD varies markedly between studies. Possible explanations for this include the criteria used to diagnose granulomas; whether or not isolated giant cells are included among granulomas; the number of biopsies obtained; and the number of sections examined. Granulomas are found in the bowel wall in 50% to 87% of colectomy specimens, in 15% to 36% of colonoscopic biopsies, and in 20% to 38% of regional lymph nodes (87,99,100). CD granulomas do not usually affect the regional lymph nodes when they are absent in the bowel wall.
Sometimes the granulomas are quite small (microgranulomas). Microgranulomas consist of only a few histiocytes, and are easily overlooked (Fig. 11.36). In one study, 16% of granulomas were so small as to be seen in only 6 of 90 serial sections. Isolated mucosal or submucosal giant cells are seen in 13% of patients (99).
Fewer granulomas occur in the ileum than in the colon. Granulomas progressively increase in number from the ileum to a maximum number in the rectum (101). The granulomas also occur in various other tissues and organs, including the lymph nodes, pancreas, mesentery,
peritoneum, liver, lung, kidney, and, occasionally, bones, joints, and skeletal muscle. The presence of granulomas does not indicate disease activity, nor does it affect the postoperative recurrence rate.
peritoneum, liver, lung, kidney, and, occasionally, bones, joints, and skeletal muscle. The presence of granulomas does not indicate disease activity, nor does it affect the postoperative recurrence rate.
 FIG. 11.34. Crohn disease. Inflammation extends through the full thickness of the bowel wall. Prominent lymphoid aggregates are present within the submucosa and muscularis propria. |
The granulomas consist of small, localized, well-formed, loose or more compact aggregates of epithelioid histiocytes with or without Langerhans giant cells, often with a surrounding cuff of lymphocytes (see Figs. 11.35 and 11.36). Nodal granulomas also contain centrally located T lymphocytes and dendritic cells. Older lesions may show varying degrees of hyalinization and fibrosis. The granulomas may be numerous or very difficult to find. Granulomas that have definite foci of necrosis or suppuration, or are restricted to the edges of ruptured crypts, are not specific for CD.
Granulomas may be observed anywhere within the intestinal wall and along blood vessels or nerves, especially in the submucosa (Fig. 11.35), mucosa (Fig. 11.36), and subserosa, and in the regional lymph nodes (Fig. 11.38). Granulomas may lie adjacent to dilated lymphatics, causing compression of the lymphatic wall or projecting within the lumen of lymphatic spaces (Fig. 11.39). Sometimes granulomas are present in the lamina propria or in the wall of microabscesses of aphthoid ulcers.
On those rare occasions when microorganisms are found within the granulomas, they probably represent secondary invaders.
Vascular Lesions
Some postulate that CD results from an underlying vascular disease. The changes appear primarily degenerative or inflammatory in nature. Obliterating endarteritis, chronic phlebitis, and other vascular lesions affect approximately 5% of patients (Figs. 11.40 and 11.41). Obliterative changes include intimal proliferation, subintimal fibrosis, medial hypertrophy, medial fibrosis, and adventitial fibrosis, all without a significant inflammatory cell component. Degenerative arterial lesions may narrow the vascular lumen due to duplication of the internal elastic lamina with medial hypertrophy. Venous lesions feature an irregular vascular sclerosis with thickening of the wall due to hyperplasia of fibrous, elastic, and muscular tissues.
The inflammatory lesions consist of perivascular inflammation and chronic inflammatory and/or granulomatous cell infiltrates associated with an obliterative vasculopathy. Lymphocytes and plasma cells infiltrate one or more layers of small arteries or arterioles, leading to interruption of the internal elastic fibers. Areas of thrombosis are rare.
The vascular changes seen in CD must be distinguished from a primary systemic vasculitis involving the GI tract. When a primary vasculitis affects a patient with CD, extraintestinal manifestations of the disorder are usually evident.
 FIG. 11.37. Early mucin granuloma in a mucosal biopsy from a patient with ulcerative colitis. This specimen shows evidence of basal plasmacytosis, which is most evident in B. A: One sees several crypt abscesses. The right one has ruptured and herniated with extension into the surrounding lamina propria. Histiocytic cells collect at the area of herniation. B: A crypt that has ruptured and is associated with two giant cells intermingling with apoptotic cell fragments and with extravasating inflammatory cells. These lesions have a completely different appearance than the microgranulomas associated with Crohn disease. Compare this photograph with Figure 11.36. |
Neural Changes
The autonomic neural plexuses often appear hypertrophic in CD. Large, abnormal, irregular, fusiform nerve bundles and nerve trunks are present throughout the mucosa, submucosa, and muscularis propria (Figs. 11.42 and 11.43). These often contain increased numbers of ganglion cells. Occasionally, striking plexiform neuromatous proliferations associate with tortuous thick-walled arterioles. The nerve fibers contain increased amounts of vasoactive intestinal peptide (VIP) and substance P (102). They express MHC class I antigens (103) and thus the abnormal nerves become infiltrated with mast cells, lymphocytes, and plasma cells (Figs. 11.42 and 11.43). The nerves also show evidence of extensive axonal and dendritic swelling and degeneration.
Strictures
Stricture formation characterizes CD, especially in the small bowel. These strictures result from fibroblast proliferation and increased collagen deposition in the bowel wall (Fig. 11.44). The fibrosis extends along lymphatics and vascular planes and also involves the serosa and pericolonic tissues. Sclerosing lymphangitis, proliferative endophlebitis, and endarteritis are the end result of many of the inflammatory and fibrosing processes.
Some CD patients develop distinctive polypoid lesions in stricturing areas. These consist of proliferations of vessels, nerves, and muscular tissue, sometimes referred to as neuromuscular hamartomas. Grossly, one sees a cluster of sessile polyps covering normal mucosa. Although the lesions have
been described as hamartomas, it is more likely that they represent reparative lesions (Fig. 11.45).
been described as hamartomas, it is more likely that they represent reparative lesions (Fig. 11.45).
 FIG. 11.41. Vasculitis in Crohn disease. Not all cases of vasculitis are as dramatic as those illustrated in Figure 11.40. This patient with CD had only minimal vascular inflammation. Such changes might be seen in a patient with severe ulcerative colitis, so that these features may show histologic overlap. |
Pseudopolyps
Several types of polypoid lesions develop in CD. One type consists solely of inflammatory and regenerative tissues (Figs. 11.46 and 11.47). These fingerlike polyps arise in both the small and the large bowel. They contain granulation tissue and variable degrees of inflammation, sometimes covered by regenerating surface epithelium. Sometimes pseudopolyps are removed endoscopically. Other polyps contain mucosa, muscularis mucosae, edematous submucosa, submucosal fibrosis, and smooth muscle hyperplasia. These represent residual mucosal islands.
 FIG. 11.42. Neural hyperplasia in Crohn disease. A: Low magnification showing the presence of prominent ganglia and supporting neural elements in this muscularis propria. B: Higher magnification. |
Histologically, giant pseudopolyps consist of complex processes that branch and fuse to form a honeycomb pattern (Fig. 11.48). They contain an inflamed mucosa with intramucosal hemorrhage and fibrosis (Fig. 11.48). The lamina propria and surface epithelium become heavily infiltrated by plasma cells, eosinophils, lymphocytes, and neutrophils. The latter sometimes form crypt abscesses. Granulomas may also be present. Erosions, granulation tissue, and pyloric gland metaplasia can also be present. The lamina propria consists of small blood vessels, loose fibrous tissues, and smooth muscle fibers derived from the muscularis mucosae.
Displaced Epithelium
It is not uncommon to encounter displaced epithelium in resection specimens of CD patients. This entity is referred to as enteritis cystica profunda or colitis cystica profunda when it affects the small bowel or colon, respectively (Fig. 11.49). Enteritis cystica profunda occurs less commonly than its colonic counterpart, colitis cystica profunda. Displaced epithelium results from epithelial implantation into the submucosa, muscularis propria, or serosa following mucosal ulceration or the formation of mucosal microdiverticula, a common event in CD patients. Mucosal repair following regeneration of an ulcer leaves the detached epithelium buried in the submucosa. It eventually becomes covered by an intact mucosa (Fig. 11.49). Displaced epithelium also results from epithelialization of fissures or fistulous tracts. The displaced epithelium often becomes cystically dilated, containing large mucin accumulations.
Grossly, the bowel wall appears thickened. The cut surface of the bowel discloses the presence of numerous cystic submucosal spaces. These are often quite prominent and glisten because of their mucinous content. The mucosa overlying such lesions usually demonstrates histologic evidence of active or healed CD. Histologically, one sees mucus-filled cysts in the submucosa, muscularis propria, and serosa. These are lined by cuboidal to columnar epithelium containing numerous goblet cells, enterocytes, and Paneth cells, all supported by a normal lamina propria. Sometimes the cyst lining disappears due to pressure atrophy from large intracystic mucinous accumulations.
Sometimes it is difficult to determine whether the displaced epithelium represents an invasive mucinous carcinoma or merely displaced epithelium, especially when lamina propria does not surround the glands or when the benign epithelium produces excessive amounts of mucin, resulting in large mucinous cysts containing scant epithelial elements (Fig. 11.50). Features that help to rule out malignancy include the absence of desmoplasia, the presence of surrounding lamina propria, and an absence of cytologic atypia within the displaced glands. Cytologic atypia and areas of desmoplasia around angular, irregularly shaped glands characterize invasive cancers, particularly of the nonmucinous type.
In some cases, it may be impossible to determine whether one is dealing with displaced epithelium or an invasive cancer. Sometimes careful sampling and examination of the surface epithelium helps resolve the diagnostic dilemma. If the surface epithelium appears dysplastic, the possibility of an invasive lesion increases.
Serosal and Mesenteric Changes
The subserosa becomes considerably thickened, often as the result of hyperplasia of the subserosal fatty tissues, edema, fibrosis, acute and chronic inflammation, and granuloma formation. Nodular lymphoid aggregates are very common, and these may resemble serosal miliary granulomas grossly. The serosa may also become covered with a fibrinous precipitate or a fibropurulent exudate. The mesenteric changes closely parallel those seen in the serosa. The draining lymph nodes often become enlarged and frequently contain lipogranulomas.
Superficial Crohn Disease
The microscopic features of superficial CD are those of classic CD with aphthous ulcers, fissures, hypertrophy of the muscularis mucosae, and submucosal nerves with associated nodular lymphoid aggregates and granulomas in skip areas. However, the Crohn-type inflammatory changes remain limited to the mucosa and submucosa. Microscopically, there is no or minimal transmural inflammation and no fissures extend below the submucosa. Rare lymphoid nodules are present in the subserosa adjacent to the muscularis propria. The diagnosis is based on the association with classic CD in other segments of the same resection specimen.
Patients with both long and short segment superficial CD may have watery diarrhea. Obstructive symptoms and evidence of a stricture affect a small number of such patients, and these patients typically have transmural CD elsewhere in the surgical specimen. The gross mucosal appearance of superficial CD consists of a cobblestoned pattern that is more diffuse and more finely nodular than that seen in classic CD. The bowel wall tends to be thin and pliable rather than thick and rigid.
Histologic Features of Proximal Gastrointestinal Lesions
The villous architecture in the proximal small intestine varies from normal to a complete loss of villi and a flattened mucosa covered by an abnormal surface epithelium infiltrated by large numbers of neutrophils. Areas of flattening may lie adjacent to more normal-appearing tissues. In the duodenum, the most severe damage occurs proximal to the ligament of Treitz. The mucosa may contain crypt abscesses, erosions, granulation tissue, pyloric metaplasia, increased numbers of plasma cells, and neutrophils, often in the
absence of granulomas. When only minimal changes are present, one sees acute inflammation consisting of focal neutrophilic collections in the lamina propria and surface epithelium. Surface cells vary from normal, to cuboidal, to completely flattened. Some appear vacuolated and others are frankly megaloblastic, presumably due to coexisting vitamin deficiencies. Intraepithelial lymphocytes may be mildly increased, but are not present in the number typically seen in celiac disease. Neutrophils often infiltrate the epithelium in large numbers. Noncaseating granulomas are sometimes
seen, and are often present on a background of lymphocytic and plasmacytic inflammation. A normal biopsy does not exclude the possibility of involvement by CD, since the inflammation is usually patchy.
absence of granulomas. When only minimal changes are present, one sees acute inflammation consisting of focal neutrophilic collections in the lamina propria and surface epithelium. Surface cells vary from normal, to cuboidal, to completely flattened. Some appear vacuolated and others are frankly megaloblastic, presumably due to coexisting vitamin deficiencies. Intraepithelial lymphocytes may be mildly increased, but are not present in the number typically seen in celiac disease. Neutrophils often infiltrate the epithelium in large numbers. Noncaseating granulomas are sometimes
seen, and are often present on a background of lymphocytic and plasmacytic inflammation. A normal biopsy does not exclude the possibility of involvement by CD, since the inflammation is usually patchy.
 FIG. 11.47. Inflammatory pseudopolyps. A: The inflammatory pseudopolyps present in this photograph differ from those shown in Figure 11.46, in that they represent residual islands of mucosa and submucosa. They contain a prominent submucosal core. The surrounding tissues are ulcerated down to the level of the muscularis propria. B: Higher magnification of the pedunculated lesion indicated by the arrow in A. One can see the central fibrovascular submucosal core with a covering of granulation tissue and extravasated red cells. C: Higher magnification of the lesion. |
Gastric biopsies show some degree of abnormality in as many as 75% of patients with CD (104,105). The most commonly identified alteration is focal infiltration of the gastric pits and glands by inflammatory cells (Fig. 11.51). These infiltrates may include neutrophils, T lymphocytes, and histiocytes in variable numbers. This focal inflammation affects both the neck region and deep aspects of the gastric glands, and is more commonly seen in the antrum than in the body of the stomach. In addition, granulomas may be seen in from 9% to 16% of patients (104,105) (Fig. 11.51).
 FIG. 11.48. Filiform polyp in Crohn disease. This long filiform polyp was one of dozens present in the colon. They are characterized by long submucosal extensions covered by regenerative mucosa. |
The major differential diagnosis is with Helicobacter pylori gastritis. H. pylori gastritis may also demonstrate chronic active inflammation, but the infiltrates are almost entirely neutrophilic, and localize to the neck region of the glands. The presence of deep active inflammation should alert the pathologist to the possibility of CD. However, the possibility of H. pylori infection should be ruled out with the use of special stains in all patients demonstrating any form of chronic active gastritis. It is important to note that some patients with CD may have superimposed H. pylori infection.
Crohn disease may affect the esophagus, and when it does, it may be difficult to separate the lesions from other forms of granulomatous esophagitis, especially if one is unaware that the patient has known Crohn disease (Fig. 11.52). Clinically, severe forms of esophageal Crohn disease may simulate carcinoma because of the presence of an irregular, stenotic esophageal segment.
Crohn Disease of the Orogenital System
Oral vesicular lesions and aphthous ulcers affect 49% of patients with CD. Typical CD is usually present in the gut,
but occasionally CD first presents as oral lesions. Lesions may develop in the lips, epiglottis, and aryepiglottic folds.
but occasionally CD first presents as oral lesions. Lesions may develop in the lips, epiglottis, and aryepiglottic folds.
 FIG. 11.52. Esophageal Crohn disease. Figures A and B are from the esophagus of the child whose stomach is depicted in Figure 11.51. A: The esophageal squamous mucosa shows nonspecific inflammation and regenerative changes. B: Although no granulomas were present in this biopsy, a multinucleated giant cell is present in the submucosa. |
Oral lesions appear nodular and firm. Biopsy demonstrates the presence of chronic inflammatory cells and granulation tissue. Numerous large, well-formed, noncaseating granulomas containing epithelioid cells, giant cells, and peripheral lymphocytes may also be present. Patients with anal or perianal disease often have vaginal involvement characterized by the presence of nonspecific inflammation, fissures, and fistulae. Occasionally, granulomas are present (Fig. 11.53).
Evaluation of Resection Margins in Crohn Disease
Frozen sections of resection margins are unnecessary and should be avoided (280). This is because the rate of recurrence in CD following surgical resection is not influenced by the status of the resection margins (106). Factors that do affect the risk of postoperative recurrence of CD include extent of disease at the time of surgery and the indication for surgery, with those who failed medical therapy or had perforating disease having a higher risk of recurrence (106,107). Smoking is also a factor affecting disease recurrence (108).
Complications
The complications of CD are listed in Table 11.10. The extraintestinal and neoplastic manifestations are discussed
later in this chapter. Complications also result from therapy. These include steroid-related osteonecrosis often affecting the hip or knee, as well as secondary viral or bacterial infections.
later in this chapter. Complications also result from therapy. These include steroid-related osteonecrosis often affecting the hip or knee, as well as secondary viral or bacterial infections.
TABLE 11.10 Complications of Crohn Disease | |
|---|---|
|
Ulcerative Colitis
Incidence
In recent decades, the incidence of UC in the United States and in Europe has risen, whereas in other countries the incidence has plateaued (2,87,109). It is likely that two factors have contributed to this increase: (a) improved survival of incident cases and (b) diagnosis of milder cases due to increased use of sigmoidoscopy and fecal occult blood testing in the community. UC mostly affects young white people, but there is an increasing recognition that the disease affects many ages and many ethnic groups (2). The incidence of UC inversely correlates with smoking and clinical relapses have been associated with smoking cessation (110).
Clinical Features
UC demonstrates a wide clinical spectrum affecting all age groups, with a predominance of the disease in young and middle-aged persons. The peak age of incidence is the 3rd decade. Women are more commonly affected than men. Mean age at diagnosis is 32 years (111). The disorder is less common in black persons than white persons. Fifty to sixty percent of patients present with an insidious onset of vague abdominal discomfort. Symptoms vary from those of mild rectal irritation to an acute severe colitis. In children, growth failure, characterized by decreased linear growth and delayed sexual maturation, often represents the first sign of disease. Patients with UC develop this complication less commonly than CD patients (112).
Diarrhea, hematochezia, urgency of defecation, attacks of crampy abdominal pain, and perianal soreness are common in early stages of the disease. Abdominal pain is usually less severe than in CD. Approximately 10% of patients initially present with severe colitis characterized by abdominal pain, more than 40 bloody stools per day, fever, tachycardia, weight loss, and hypoalbuminemia. When UC remains limited to the left colon, constipation rather than diarrhea may result because colonic spasm results in stool retention in the right colon where the normal absorptive capacity is unimpaired.
Disease onset is abrupt in approximately 30% of patients. The disease may be explosive, with a sudden onset of acute diarrhea, frequent bloody stools, continuous abdominal pain, anorexia, rapid weight loss, chronic iron deficiency anemia, and a persistent fever. Acute and massive rectal bleeding affects up to 3% of patients (111). The bleeding originates from large denuded areas of the mucosa in the face of widespread telangiectatic lamina propria vessels. In contrast, the bleeding seen in CD usually originates from a localized source such as an eroded blood vessel in the submucosa or deeper layers.
Characteristically, UC is a chronic mucosal disease with relapses and spontaneous remissions. It usually starts in the rectum and then spreads more proximally. Most patients have distal disease at the time of first attack, but some have more proximal disease, including total colonic involvement. There are several major clinical presentations: (a) acute fulminating colitis, in which the whole colon and rectum are affected with extensive and deep ulcerations; (b) continuous colitis, in which the symptoms persist from the onset and vary in severity (usually only affecting the left side of the colon); and (c) recurrent colitis, in which the attacks are limited and separated by varying periods of remission. Disease distribution usually remains relatively constant, with about 50% of patients in clinical remission in any one time. Relapses are unpredictable except that the disease activity in foregoing years indicates a 70% to 80% probability that the disease will continue the following year (113). The cumulative probability of having a relapsing course is 90% after 25 years of disease. Activity in the first 2 years of diagnosis significantly correlates with having an increased probability of 5 consecutive years of disease activity. The probability of maintaining work capacity after 10 years is 92.8%, with a range of 90.8% to 94.8%.
UC progresses to a more serious form in 53.8% of patients. Factors associated with disease progression include toxic colitis, extent of disease at diagnosis, presence of joint symptoms, younger age at diagnosis, and severe bleeding (111). Various infections (CMV, Salmonella, and Clostridium difficile), medications, and intervening ischemic disease also exacerbate UC (Table 11.11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree