Voiding Disorders
NEUROPHYSIOLOGY OF VOIDING
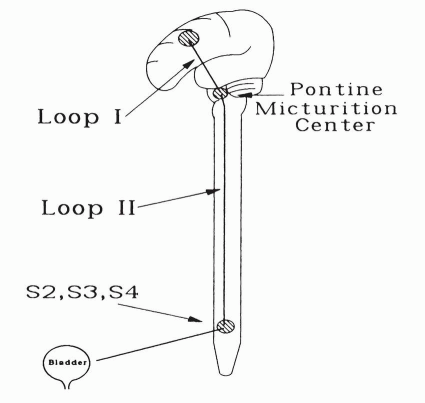
The act of micturition is a complex reflex function under voluntary control. The following diagram gives a simplified way of understanding the general neurologic innervation of the bladder and sphincter mechanisms. The coordination of the micturition reflex (i.e., detrusor contraction with sphincter relaxation) is controlled by the brain stem (pontine) micturition center via the long spinal (loop II) pathways to the sacral cord (S2, S3, and S4). This in turn is under voluntary control by suprapontine higher functions via loop I.
|
Detrusor hyperreflexia with a coordinated external sphincter is caused by suprapontine lesions involving loop I (e.g., stroke, Parkinson’s disease, and tumors) as well as nonneurologic local causes (e.g., infection, outlet obstruction, tumor, stone, and foreign body).
Detrusor hyperreflexia with external sphincter dyssynergia is generally caused by suprasacral spinal lesions involving loop II (e.g., tumor, multiple sclerosis, myelodysplasia, and spinal arteriovenous malformations).
Detrusor areflexia can result from interruption of sacral reflex arcs (e.g., diabetic neuropathy, multiple sclerosis, herniated discs,
and spinal cord tumors), as well as direct myogenic causes (e.g., prolonged urinary retention). Areflexia also occurs during the period of spinal shock after suprasacral spinal cord injury.
and spinal cord tumors), as well as direct myogenic causes (e.g., prolonged urinary retention). Areflexia also occurs during the period of spinal shock after suprasacral spinal cord injury.
CLASSIFICATIONS OF DYSFUNCTIONAL VOIDING
Many classification systems have been promoted for categorizing voiding disorders based on either neuroanatomic, urodynamic, or functional criteria. The Wein classification system is a beautifully simplistic functional categorization based on the failure of the bladder to store or empty. It serves most clinical voiding disorders well, whether of neurogenic or nonneurogenic origin, and helps guide one toward the correct treatment options.
Functional Classification of Voiding Disorders
|
Failures to store because of the bladder simply include involuntary bladder contractions, low compliance, and hypersensitivity, whereas outlet problems are simply due to inadequate outlet resistance. Failures to empty because of the bladder are a result of poor or no bladder contractility, whereas outlet problems are from mechanical (e.g., benign prostatic hyperplasia [BPH], stricture, etc.) or functional (dyssynergia) obstruction. Combination deficits can also occur as in spinal cord injury (detrusor hyperreflexia and sphincter dyssynergia).
Detrusor hyperreflexia refers to involuntary bladder contractions on urodynamic studies caused by a neurologic disorder, whereas involuntary contractions without a neurologic cause are termed detrusor instability. More popular today is the general term overactive bladder that refers to the symptoms of frequency and urgency without urodynamic confirmation of detrusor hyperreflexia or instability.
URODYNAMICS
Urodynamics is the study of lower urinary tract physiology. It is a complex field that includes uroflowmetry, cystometry, urethral pressure profilometry, and electromyography. Even a brief
overview of all these areas is beyond the scope of this manual. Only basic uroflowmetry and cystometry will be covered because they are generally all that are required for most clinical urodynamic workups. Remember that a detailed history is the foundation of any evaluation of a voiding disorder.
overview of all these areas is beyond the scope of this manual. Only basic uroflowmetry and cystometry will be covered because they are generally all that are required for most clinical urodynamic workups. Remember that a detailed history is the foundation of any evaluation of a voiding disorder.
Urinary Flow Rate/Residual Urine
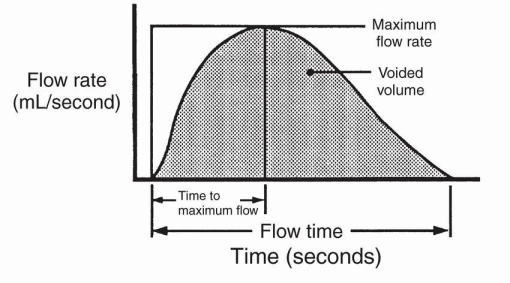
The combination of a uroflow followed by determination of the residual urine is the most useful test in the study of any voiding disorder. Urinary flow rate is best recorded on an electronic flowmeter, which plots the flow pattern in a graphic representation of instantaneous flow rate versus voiding time.
Peak uroflow rate is the only objective measure of functional bladder outlet obstruction, and it is directly dependent on the volume voided. Peak flows measured when the voided volume was <150 mL should be disregarded.
|
Use of this flow nomogram allows a more accurate determination of outflow resistance by removing the effect of intravesical volume on flow rate. Peak flow rates more than two standard deviations below the mean are highly suggestive of outflow obstruction.
|
Cystometry
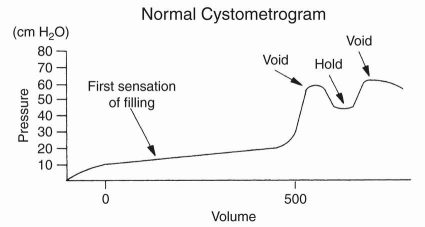
Cystometry is generally utilized to evaluate bladder filling and storage. A cystometrogram is a pressure/volume curve obtained by filling the bladder with a fluid (either water or carbon dioxide) at a constant infusion rate while monitoring changes in intravesical pressure. The patient is asked to inhibit any urge to void during the study. Any detrusor contractions >15 cm H2O are considered abnormal or uninhibited contractions. A voiding phase cystometrogram may be obtained at the end of the study when the patient has a strong urge to void by asking him or her to voluntarily urinate around the catheter.
Data to be noted during the cystometrogram include the following:
Volume at first sensation of filling (proprioception)
Volume at sensation of fullness
Volume at desire to void
Occurrence of a voluntary detrusor contraction when asked to void
Ability to inhibit a voluntary detrusor contraction
|
▪ Normal Cystometrogram
A normal cystometrogram should demonstrate a first sensation of filling at 100 to 200 mL, normal accommodation with continued filling and good compliance (i.e., <10 cm H2O change in intravesical pressure), and a sensation of fullness and desire to urinate at 350 to 450 mL. Asking the patient to produce a voluntary detrusor contraction at the end of the study is often unsuccessful because of the patient’s inability to properly relax in the test setting. Normal sensation and compliance with an absence of uninhibited contractions are all that are needed to consider the study normal.