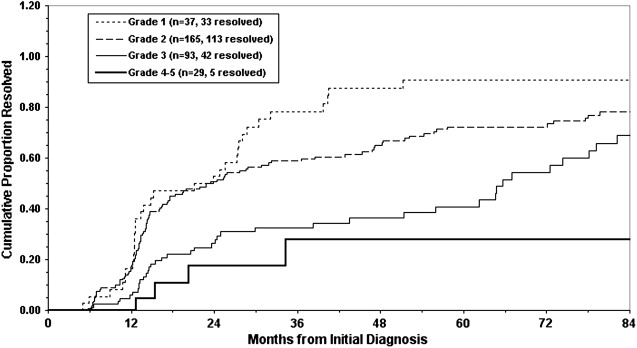
There has been an emergence of a therapeutic nihilistic attitude about the surgical treatment of vesicoureteral reflux (VUR). Evidence-based reviews have questioned whether surgical treatment is beneficial for children with VUR. Even the use of prophylactic antibiotics, which have traditionally been the first-line therapy recommended for virtually all patients with VUR, has come under scrutiny after several randomized controlled trials found them to have no effect on decreasing the risk of urinary tract infections (UTIs) in children with VUR. Grade is the strongest predictor of VUR resolution, with high-grade VUR being much less likely to resolve. Other factors that negatively influence resolution include lower bladder volume or pressure at onset of reflux, older age, female sex, bilateral VUR, ureteral duplication, abnormal or scarred kidneys, and bladder dysfunction. These factors can be used, along with grade, in computer models or nomograms to improve the ability to predict spontaneous resolution.
There has been an emergence of a therapeutic nihilistic attitude about the surgical treatment of vesicoureteral reflux (VUR). Evidence-based reviews have questioned whether surgical treatment is beneficial for children with VUR. Even the use of prophylactic antibiotics, which have traditionally been the first-line therapy recommended for virtually all patients with VUR, has come under scrutiny after several randomized controlled trials found them to have no effect on decreasing the risk of urinary tract infections (UTIs) in children with VUR. This issue is now the primary focus of the current randomized, double-blinded, placebo-controlled trial in children with VUR and UTIs in the United States—the RIVUR trial. This nihilistic pattern challenges the effort that was put forth decades ago to evaluate children with UTIs for anatomic abnormalities, primarily VUR. Now more than ever, urologists treating VUR face a difficult decision process in deciding which patients should be followed conservatively and which should be offered operative correction. Factors influencing this decision include the risk of developing a UTI, and associated risk factors for UTIs such as voiding dysfunction, risk of development of new renal scars, and chance for spontaneous resolution. It is through consideration of these factors for each individual patient that the urologist tries to optimize the selection of patients who will benefit most from operative therapy. This review explores the important questions that guide the determination of who benefits from surgical treatment. The first question to be answered is, what does surgical correction of VUR do for patients?
Benefits of surgical treatment of VUR
In the 1990s, the first American Urological Association (AUA) panel to develop guidelines for the treatment of VUR was convened, and their summary statement was published in 1997. This meta-analysis of multiple prior treatment options gave recommendations for the treatment of boys and girls with primary VUR from birth through age 10 years. The panel stratified their recommendations based on whether or not renal scarring was present. Surgical treatment was recommended for patients initially older than 1 year with grade V or bilateral grades III and IV if renal scarring was present. No consensus was reached as to what to do at the opposite end of the spectrum, such as those with persistent grades I to II VUR without renal scarring.
Surgical correction of VUR can be accomplished either by ureteral reimplantation or by endoscopically injecting a bulking agent at the ureterovesical junction. The success rates for ureteral reimplantation is routinely reported to be greater than 95% for grades I to IV, with slightly lower success rates for grade V. Endoscopic treatment is a less successful but shorter outpatient procedure with minimal morbidity. Published success rates have been reported to be more than 90%, but a recent meta-analysis probably gives a more realistic estimate. A single injection is successful for 67% of patients, and with a second injection the aggregate success rate increases to 87% of patients. There is a significantly lower success rate for a third injection (34%); thus, after a second attempt at endoscopic injection, failures should be treated by other means. There is no debate that reflux can be corrected with surgery. More important are the benefits children may receive by no longer having VUR.
Only a few randomized studies compare observation on prophylactic antibiotics with surgical correction. The largest study was the International Reflux Study. A summary of randomized studies of surgical correction of VUR is shown in Table 1 . The main benefit demonstrated in these studies is that children are significantly less likely to develop pyelonephritis after surgical correction of VUR. In the International Reflux Study, the overall rates of UTIs in the medical and surgical arm at 5 years were about 30%. In the United States, the rate of pyelonephritis was 8% for the patients treated surgically versus 21% in those treated medically. In addition, only 10% of the medically treated patients had resolution of VUR at 5 years and only 47% at 10 years, whereas virtually all of the surgically treated patients were free of VUR. Renal growth, the incidence of new renal scars, rates of hypertension, and progression to renal failure do not seem to be altered by surgical treatment. Although the benefits of surgical correction of VUR have not been what was initially hoped, the surgical treatment of VUR has a low complication rate, high success rate, and has not been harmful to renal function. There has been only one randomized study of patients treated endoscopically, which examined primarily rates of VUR present at 1 year after treatment. In this study, 61 patients were randomized with 40 undergoing endoscopic treatment with dextranomer/hyaluronic acid (Dx/Ha). After 12 months, VUR was present in 62% of the medically treated patients and 31% of the patients treated endoscopically. UTIs were reported in 9 (22%) surgical patients and in none of the patients on prophylaxis; however, the details of the UTIs (pyelonephritis, cystitis, or asymptomatic bacteruria) were not given. A meta-analysis of studies of endoscopic treatment shows a lower incidence of febrile UTIs after treatment. Considering what is known about the benefits of surgical correction of VUR, the focus should be on selecting patients for treatment by identifying those at risk for recurrent pyelonephritis and those in whom VUR will not spontaneously resolve.
| Study | Description | Summary of Results |
|---|---|---|
| Birmingham Reflux Study | Randomized controlled trial (RCT) of severe VUR. Antibiotic prophylaxis vs ureteral reimplantation | No difference in rates of UTI, renal growth, new or progressive scarring after 5 years |
| International Reflux Study (Europe, United States) | RCT of children age <11 y with grade III or IV VUR. Antibiotic prophylaxis vs ureteral reimplantation | No difference in overall rate of UTI or new scar formation at 5 years. Significantly lower rate of pyelonephritis in the surgical group |
| Smellie et al | RCT of children age 1–12 years with bilateral grades III–V VUR with bilateral scarring. Antibiotic prophylaxis vs ureteral reimplantation | At 4 and 10 years no difference in renal function, rates of hypertension or renal failure, or renal growth in patients treated medically vs ureteral reimplantation |
| Capozza and Caione | RCT of children age >1 year with grades II–IV VUR. Antibiotic prophylaxis vs endoscopic injection of Dx/Ha | More UTIs in the Dx/Ha-treated group. Reflux was resolved in 69% of the Dx/Ha-treated vs 38% treated with prophylactic antibiotics at 1 y |
Ureteral reimplantation versus endoscopic injection
The controversial topic of whether VUR should be treated with ureteral reimplantation or endoscopic injection is one fueled with many divergent opinions and treatment philosophies. While the AUA Reflux Guidelines did not recommend endoscopic therapy as a surgical option, this was due to a lack of availability of a United States Food and Drug Administration approved agent Since 2001, dextranomer/hyaluronic acid copolymer (Dx/Ha) (Deflux, Oceana Therapeutics, Edison, NJ) has been available in the United States. The guidelines are currently being revised and will likely include endoscopic injection as an option for surgical treatment. The choice of technique is one that needs to be individualized to the patient. Open ureteral reimplantation has a long track record of efficacy for all grades of VUR. Endoscopic correction success has been shown to be grade dependent, with most studies suggesting it is more effective for lower grades. Table 2 shows the efficacies for a single injection based on grade of VUR. There are few long-term studies of patients with endoscopic treatment. Recurrence of VUR seems to be partially dependent on the properties of the agent used. Long-term recurrence of VUR for bovine glutaraldehyde crosslike collagen was 87% at 3 years versus a recurrence rate of 13% at a median of 3 years for Dx/Ha. Most studies of endoscopic treatment of VUR report the success rate at 6 to 12 weeks. In 1 series of 246 ureters successfully treated endoscopically with Dx/Ha that were retested at 12 months, 27% showed recurrent VUR. Most of those that recurred at 1 year were higher grades (III–V) of VUR. The only long-term follow-up study beyond 5 years was in patients treated with polytetrafluoroethylene. In this series there was a 5% recurrence at 10 years. Studies have reported that febrile UTIs after successful endoscopic treatment with Dx/Ha is a predictor of recurrent VUR. There is no consensus on which patients should undergo ureteral reimplantation or endoscopic injection. One should consider the efficacy based on the individual’s grade of VUR, age, infection history, and renal function. There have been no studies evaluating the risk of new scars in patients who have recurrent VUR and pyelonephritis after endoscopic therapy.
| Grade of VUR | % Success (Ureters) |
|---|---|
| I | 79% |
| II | 79% |
| III | 72% |
| IV | 62% |
Ureteral reimplantation versus endoscopic injection
The controversial topic of whether VUR should be treated with ureteral reimplantation or endoscopic injection is one fueled with many divergent opinions and treatment philosophies. While the AUA Reflux Guidelines did not recommend endoscopic therapy as a surgical option, this was due to a lack of availability of a United States Food and Drug Administration approved agent Since 2001, dextranomer/hyaluronic acid copolymer (Dx/Ha) (Deflux, Oceana Therapeutics, Edison, NJ) has been available in the United States. The guidelines are currently being revised and will likely include endoscopic injection as an option for surgical treatment. The choice of technique is one that needs to be individualized to the patient. Open ureteral reimplantation has a long track record of efficacy for all grades of VUR. Endoscopic correction success has been shown to be grade dependent, with most studies suggesting it is more effective for lower grades. Table 2 shows the efficacies for a single injection based on grade of VUR. There are few long-term studies of patients with endoscopic treatment. Recurrence of VUR seems to be partially dependent on the properties of the agent used. Long-term recurrence of VUR for bovine glutaraldehyde crosslike collagen was 87% at 3 years versus a recurrence rate of 13% at a median of 3 years for Dx/Ha. Most studies of endoscopic treatment of VUR report the success rate at 6 to 12 weeks. In 1 series of 246 ureters successfully treated endoscopically with Dx/Ha that were retested at 12 months, 27% showed recurrent VUR. Most of those that recurred at 1 year were higher grades (III–V) of VUR. The only long-term follow-up study beyond 5 years was in patients treated with polytetrafluoroethylene. In this series there was a 5% recurrence at 10 years. Studies have reported that febrile UTIs after successful endoscopic treatment with Dx/Ha is a predictor of recurrent VUR. There is no consensus on which patients should undergo ureteral reimplantation or endoscopic injection. One should consider the efficacy based on the individual’s grade of VUR, age, infection history, and renal function. There have been no studies evaluating the risk of new scars in patients who have recurrent VUR and pyelonephritis after endoscopic therapy.
| Grade of VUR | % Success (Ureters) |
|---|---|
| I | 79% |
| II | 79% |
| III | 72% |
| IV | 62% |
Pyelonephritis in patients with VUR
If the main benefit of treating VUR is the prevention of pyelonephritis and its associated sequelae, then the main focus in selecting patients for surgical correction of VUR should be those who present with recurrent pyelonephritis and those who are at greatest risk for recurrent pyelonephritis after diagnosis. Although the former can be selected at presentation after appropriate evaluation, it is difficult to predict which children will constitute the 10% to 20% of patients who will have a subsequent UTI per year. The presence of renal scarring, as detected on a dimercaptosuccinic acid (DMSA) renal scan, has been proposed as a way of identifying these patients. Patients with VUR and an abnormal renal scan have, in a retrospective series, been shown to have much higher likelihood of having a breakthrough infection if they also had dilating (grades III through V) VUR. The incidence of breakthrough infections was 60% in those with an abnormal DMSA renal scan, versus only 6% of those with a normal DMSA scan. In addition, patients with an abnormal DMSA renal scan (renal scarring) in general have a lower likelihood of spontaneous resolution of VUR. Whether the scarring is directly involved in this increased risk or is simply a marker of a worse anatomic defect at the ureterovesical junction is unknown. There have been limited studies of DMSA scans in lower grades of VUR; thus, whether scarring is as important in these grades is unknown.
VUR is typically present in less than 50% of patients who have acute pyelonephritis. In a meta-analysis of studies evaluating postpyelonephritic scarring, the incidence of permanent scarring in patients with an initial DMSA scan showing pyelonephritis was 41%. There may be some geographic variations, with differing rates from 25% to 49% across the world. Renal scarring was strongly associated with VUR in patients after acute pyelonephritis. Renal scarring after acute pyelonephritis is a rare finding in patients without VUR. In the International Reflux Study, the risk of new renal scarring was low in children after the age of 6 years. This finding is being challenged by reports of children with acute pyelonephritis presenting at all ages, showing that the risk of developing renal scars is present even at older ages. Surprisingly, the risk was not increased in infants younger than 1 year. These findings may indicate that there is not a safe age after which there should be little concern for the development of new renal scars. In the International Reflux Study there was no difference in the progression and development of new scars in the medically and surgically corrected patients, despite a higher number of patients with pyelonephritis in the medically treated group. These contrary findings may be due to identifying preexisting scars in older patients or selection bias in the International Reflux Study that may have precluded older children with new scars from being enrolled.
Whereas it used to be widely believed that all scarring was postinfectious, it is now clear that renal abnormalities associated with VUR can precede infection. In patients with antenatal hydronephrosis and VUR, more than one-third have abnormalities detected on DMSA scans before the development of UTIs. These areas of abnormality are believed to be regions of hypoplasia or dysplasia, which are postulated to be caused by abnormal embryogenesis of the kidney associated with the abnormal development of the ureterovesical junction that leads to VUR. There is currently no way to differentiate abnormalities that are postinfectious versus congenital on initial DMSA scan or intravenous pyelography. In patients with prenatal hydronephrosis, it is unclear whether the abnormal DMSA scans will predict the likelihood of subsequent episodes of pyelonephritis or decreased chances for spontaneous resolution. Because most of these patients are male, the risk of infection may be more influenced by other factors, such as circumcision status.
Effect of age and sex on VUR resolution
Up until the widespread use of DMSA scanning to detect pyelonephritis and renal scarring in patients with febrile UTIs, it was generally believed that children younger than 6 years, particularly infants, were at the highest risk for pyelonephritis-induced scarring. The scarring in these studies was typically detected by intravenous pyelogram, which may take years to become visible after the infectious event that triggered the scar. If the infant’s kidneys are more susceptible to scarring, then why do the studies using DMSA fail to document permanent scarring more often in those with follow-up imaging after pyelonephritis? In a study by Garin and colleagues, initial DMSA scan indicated pyelonephritis in all patients (median age 2), but scarring developed in only 6%. Most underwent a scan 6 months after the original but only repeated the scan if they had another UTI. While this question remains unanswered, one can hypothesize that “new scars” that develop over time in patients followed with VUR simply are too tiny to detect radiographically when they form in the infant’s kidney. The changes being detected by intravenous pyelograms may be the result of the abnormal growth of the kidney following injury from the infection. An infant’s kidneys undergo significant growth over the first few years of life, and just as a small surgical scars grows larger with the child, it is likely that some small areas of renal scarring will become more noticeable with the child’s growth and become apparent only after they are older. Because most recent studies have not repeated DMSA renal scans that were normal at presentation, it cannot be assuredly concluded that an initial normal DMSA is a guarantee of a patient being free from renal scarring throughout life and therefore not at risk for sequelae from VUR. Progression and new scar formation is one of the secondary outcomes being measured in the RIVUR trial, and will hopefully help answer whether the kidneys really are more susceptible to scarring in infancy.
In cases of VUR presenting as antenatal hydronephrosis, boys are more commonly affected than girls. Boys more often have bilateral and higher grade VUR at presentation. As noted previously, up to 40% of these patients may have preexisting abnormalities on DMSA scan in the absence of UTIs. In patients presenting with UTIs, the majority are female. Approximately 8% of females will experience a UTI before the age of 7 years versus only 2% of boys. Recurrence of infection will occur in up to 30% of these children. Breakthrough infections are more common in females than males. While in general the resolution rates for males and females with a given grade and laterality of VUR are similar, there have been studies that show a slightly better rate for resolution of low-grade VUR in males over time. In addition, there is good evidence that boys with VUR who present in the first year of life have significantly better rates of resolution for high grades (IV and V) compared with older children and females. Rates of resolution of up to 29% at 1 year following diagnosis for grades IV and V have been reported. After 1 year, the resolution rate drops significantly and is similar to females. One study compared the resolution of infants with normal kidneys to those with bilateral abnormal kidneys (defined as abnormal DMSA scan or renal ultrasound). These investigators found that patients with the best chance for spontaneous resolution had normal kidneys, whereas none of those with bilateral abnormal kidneys resolved (100% vs 0%) at a mean age of 16 months. The patients with a single normal kidney had a 50% resolution rate at 16 months of age.
When the effect of age is considered independently, there is a decreasing chance for reflux resolution in patients with grade III reflux, particularly with bilateral VUR. In the 1997 AUA guidelines, the chances of spontaneous resolution over a 5-year period in a child younger than age 2 years with bilateral grade III VUR was reported to be approximately 50%, versus 15% if the child was older than 6 years. In predicting early resolution of VUR (within 2 years of diagnosis), age younger than 2 years has been shown to be a significant factor independent of grade. Given these data, patients with the highest likelihood of spontaneous resolution are young male children, younger than the age of 2, with normal kidneys.
Grade of VUR: the strongest predictor
There is no controversy regarding the importance of grade in predicting the chances of spontaneous resolution and likelihood of finding associated renal scarring. As the grade of VUR increases, the chances of spontaneous resolution decrease. Multiple studies have shown that the rate of renal scaring increases with increasing grades of VUR. The same is true with congenital renal abnormalities occurring in patients with VUR detected prenatally with no infection history. Nondilating (grades I and II), older age at presentation, and fewer episodes of pyelonephritis are associated with less risk of renal scarring at diagnosis and chances of developing progressive renal scarring. Fig. 1 shows the rate of spontaneous resolution in a published series examining multiple variables to predict VUR resolution. Fig. 1 clearly shows the consistent finding of high rates of spontaneous resolution for nondilating VUR (80%–90%) and the much lower likelihood of resolution of high grade VUR. Other associated factors that can help predict VUR resolution are reviewed below.