Urothelial Neoplasms with Inverted Growth Patterns
INVERTED UROTHELIAL PAPILLOMA
This is a benign tumor of the urinary bladder comprising less than 1% of urothelial neoplasms. Cystoscopically, they appear as solitary, raised, pedunculated, or, rarely, polypoid lesions with a smooth surface (1). Lesions occur in a wide age range of patients (10-94 years), with a peak frequency in the sixth and seventh decades; there is a striking male predilection (2, 3), as is the case with most urothelial neoplasms. Tumor size varies from small (less than 3 cm) to large (up to 8 cm). Most lesions are solitary and present with hematuria.
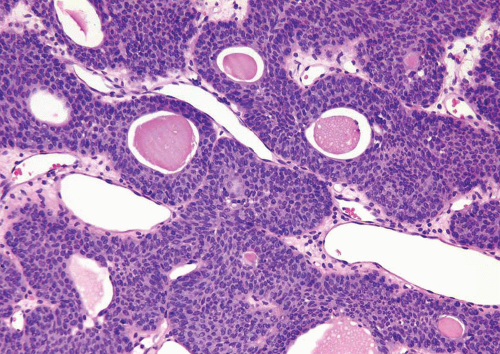
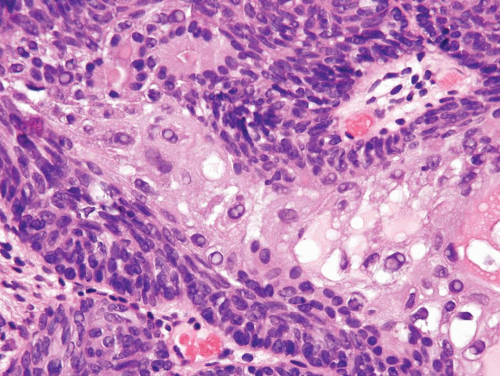
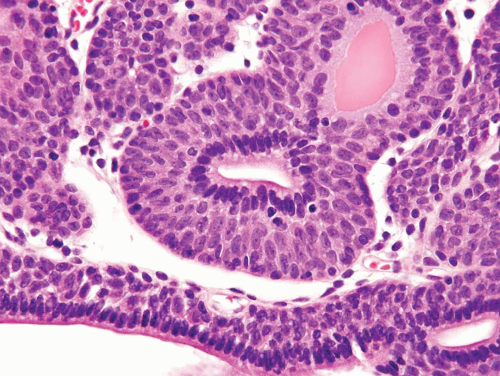
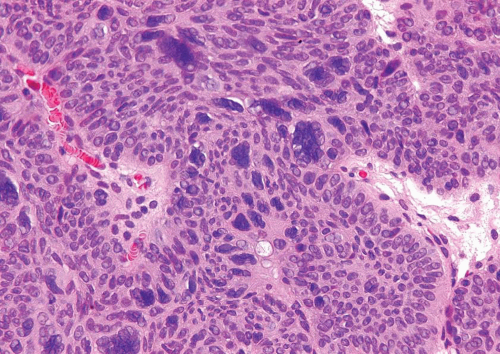
Histologically, two variations have been described: trabecular and glandular (1). In our opinion, cases of the glandular subtype overlap in their morphology with florid cystitis cystica and glandularis, and we do not use the term inverted papilloma, glandular type. The trabecular type is the classic lesion that most pathologists think of when considering inverted papilloma, histologically showing cords and trabeculae of cells arising from a smooth surface and invaginating into the lamina propria (Figs. 4.1, 4.2 and 4.3) (efigs 4.1-4.22). Because these endophytic proliferations represent inversion of papillae, the periphery is composed of darker cells that are often palisaded (the basal cells), and the central portions show maturing cells occasionally with superficial cells lining central luminal spaces filled with colloid material (Figs. 4.4, 4.5 and 4.6). It is not uncommon to see focal nonkeratinizing squamous and less commonly true glandular differentiation within the center of the urothelial cords (Figs. 4.7, 4.8). The surrounding stroma is fibrotic and nonreactive without inflammation.
Cytologic atypia is minimal to absent, although occasionally atypia of the degenerate type (smudged, hyperchromatic, and occasionally multinucleated cells) may be present, albeit focally (Fig. 4.9) (efigs 4.23, 4.24). Exceptional cases may have the classic features of benign inverted urothelial papilloma, yet have focal nondegenerative atypia. One of the authors has studied inverted papillomas with very focal atypia subdivided into the following groups: (a) areas containing prominent nucleoli, (b) foci with atypical squamous features, and (c) foci with areas of dysplasia, approaching the level of carcinoma in situ (CIS) (Fig. 4.10) (efigs 4.25-4.32). These lesions are controversial, as some experts consider that any neoplastic (nondegenerative) atypia should lead to the diagnosis of urothelial carcinoma with inverted features. Others consider that if the lesion is otherwise architecturally and cytologically classic for inverted papilloma with the exception of focal cytological atypia, it is justified to diagnose these lesions as inverted papilloma with a comment on the atypia. In the only study to investigate this phenomenon, albeit with only a few cases and limited follow-up, the clinical course was benign (4). Regardless of the nomenclature used, any atypical features in an inverted urothelial papilloma warrant periodic cystoscopic follow-up.
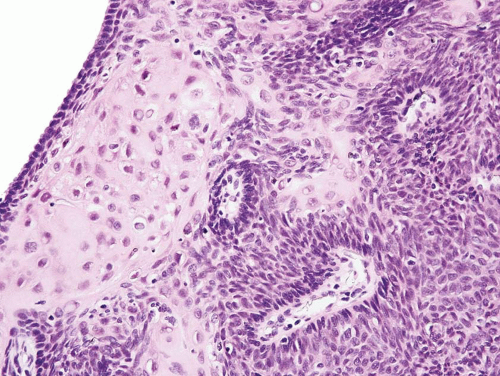
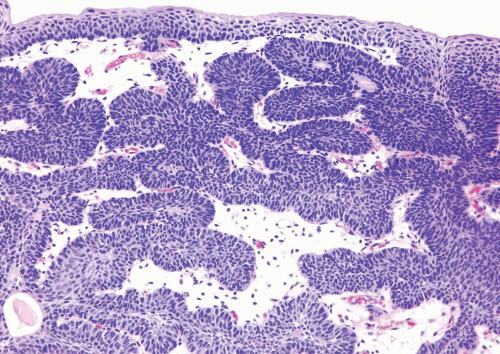 FIGURE 4.1 Inverted urothelial papilloma with focal downgrowth from overlying benign urothelium (upper right). |
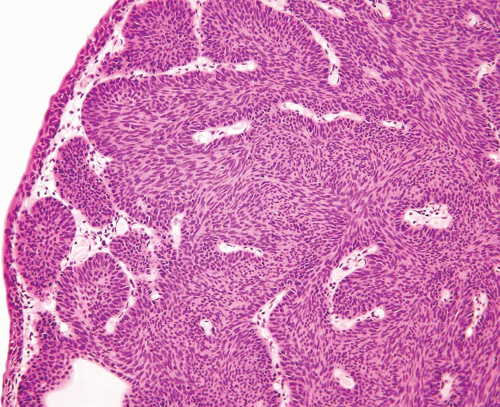 FIGURE 4.2 Inverted urothelial papilloma with undermining overlying benign urothelium. There is prominent spindling in this case with peripheral palisading. |
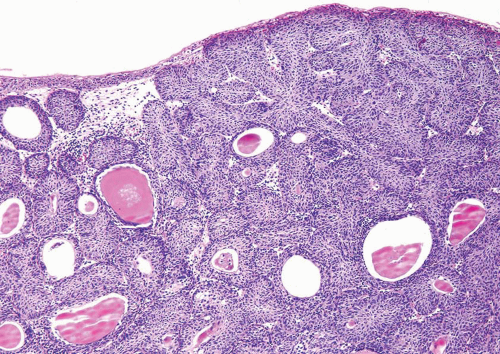 FIGURE 4.3 Inverted urothelial papilloma with undermining overlying benign urothelium. Note colloid cysts. |
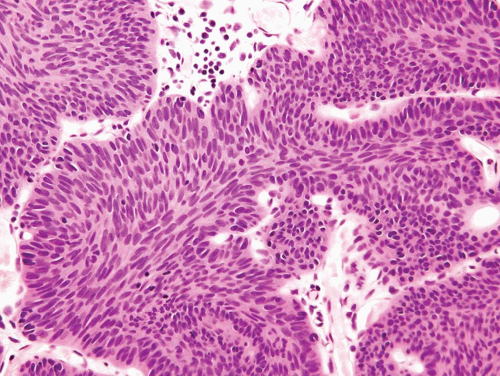 FIGURE 4.4 Inverted urothelial papilloma with cords of epithelium showing peripheral palisading and central streaming of urothelium parallel to the cords. High power of Figure 4.2. |
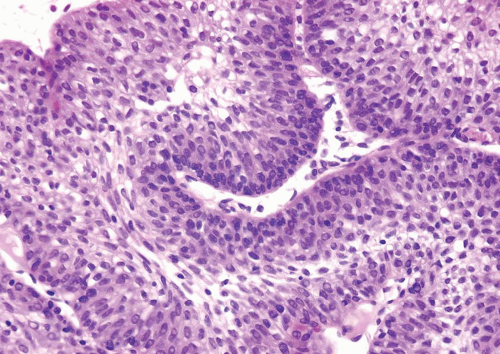 FIGURE 4.5 Inverted urothelial papilloma with peripheral palisading and central streaming of urothelium. |
Mitotic figures are rare and are only seen at the periphery of the trabeculae. The trabeculae are orderly, of relatively uniform width, with considerable ramifications and interanastomosis. The urothelium in the center of the trabeculae tend to stream parallel to the cords. Occasionally, there may be marked von Brunn nest proliferation in the adjacent mucosa. Paneth cell-like neuroendocrine differentiation is exceptionally rare (5). Other unusual variants include those with xanthomatous or vacuolated cytoplasm (Figs. 4.11, 4.12) (6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree